Diabetes Mellitus 1 (DM1) is the second most frequent chronic disease, and the most frequent endocrine-metabolic disorder in childhood. The estimated prevalence is between 1.1 and 1.4 / 1000 children under 15 years years-old. In Andalusia the prevalence is higher (1.7 per thousand).
The objective of the study is to evaluate health-related quality of life (HRQoL) and adherence to treatment, specifically in the paediatric population of Andalusia.
MethodsA multicentre cross-sectional observational analytical study was conducted on a sample of 178 patients from six hospitals with a Paediatric Endocrinology Unit. Each patient received two questionnaires; quality of life (PedsQL version 3.0) and adherence to the self-care recommendations (SCI-R) treatment. The demographic, clinical, metabolic control data, and possible complications were also collected.
ResultsHigh levels were obtained in both adherence and health-related quality of life (HRQoL). Adherence was inversely related to age and HbA1c. The health-related quality of life (HRQoL) was associated with the use of a continuous real-time glucose monitoring system (MCG-TR) combined with continuous subcutaneous insulin infusion (CSII), as well as with a lower number of severe hypoglycaemia and renal complications. The mean HbA1c was 7.1%. 12,9% of patients used ISCI. 83.2% used capillary glycemia exclusively, while 16.8% used some interstitial glucose monitoring device.
ConclusionsThis is the first study in Andalusia that analyzes the health-related quality of life (HRQoL) of pediatric patients. The results show high levels of adherence and health-related quality of life (HRQoL), as well as good metabolic control.
La Diabetes Mellitus 1 (DM1) es la segunda enfermedad crónica y el trastorno endocrino-metabólico más frecuente en la infancia. Se estima una prevalencia entre 1.1 y 1.4/1000 menores de 15 años. En Andalucía la prevalencia es mayor (1,7 por mil).
El objetivo del estudio es analizar la calidad de vida y adherencia al tratamiento, centrándonos en la población pediátrica de Andalucía.
MétodosEstudio analítico observacional transversal multicéntrico. La muestra fue de 178 pacientes de seis hospitales con Endocrinología Pediátrica. A cada paciente se le entregaron dos cuestionarios; la encuesta de calidad de vida (PedsQL versión 3.0) y adherencia al tratamiento SCI-R. Además, se recogieron datos demográficos, clínicos, del control metabólico, y complicaciones.
ResultadosSe obtuvieron niveles altos tanto en la adherencia como en la calidad de vida. La primera se relacionó de forma inversa con la edad y la HbA1c, aunque el coeficiente fue tan bajo que no permite sacar conclusiones significativas. La calidad de vida, se asoció con el uso de sistema de monitorización continua de glucosa en tiempo real (MCG-TR) integrado con ISCI, así como con menos hipoglucemias graves y complicaciones renales.
La HbA1c media fue 7,1%. El 12,9% de los pacientes usaban ISCI. El 83,2% empleaban exclusivamente la glucemia capilar, mientras que el 16,8% usaba algún dispositivo de monitorización de glucosa intersticial.
ConclusionesSe trata del primer estudio realizado en Andalucía que analiza la calidad de vida en pacientes pediátricos. Los resultados muestran niveles altos de adherencia y de calidad de vida, además de un buen control metabólico.
Type 1 diabetes mellitus (T1D) is the second most frequent chronic disease and the most frequent endocrine and metabolic disorder in the paediatric population. Its prevalence is estimated at 1.1–1.4/1000 inhabitants1,2 aged less than 16 years. The prevalence in the region of Andalusia, Spain, is greater (1.7/1000).3
Since the publication in 1993 of the Diabetes Control and Complications Trial,4 there has been rigorous evidence of the importance of maintaining adequate metabolic control, mainly defined as a lower level of glycated haemoglobin (HbA1c), to prevent chronic complications, improve quality of life in young patients2,4 and reduce the direct costs of the disease.5–7
The goal of treatment is to maintain normoglycaemia for the largest possible amount of time, to which end insulin regimens have been progressively adapted to achieve insulin levels closer to physiological levels and systems for continuous glucose monitoring and continuous insulin delivery have been developed. In the past decade, with the development of continuous subcutaneous insulin infusion (CSII) systems, there has been a shift from the multiple dose insulin injection (MDI) therapeutic approach. Various studies have found improved metabolic control with CSII systems.8–10 The data available for Spain3 show that approximately 12% of paediatric patients use CSII. However, the difference between autonomous communities in Spain is very significant, as in Andalusia only 5.5% of patients used insulin pumps in 2014.
Diabetes, the paradigm of chronic disease in childhood, affects the quality of life of the patient. Although numerous studies have compared quality of life in adults, the paediatric literature on the subject is scarce.11–14
The aim of our study was to assess the quality of life and adherence to treatment in a cohort of Andalusian patients with T1D aged less than 16 years and analyse the association between these two variables.
MethodsStudy designWe conducted a multicentre cross-sectional observational and analytical study over a 6-month period (February-July 2018). We included patients aged 2–16 years with a duration of T1D of at least 1 year that provided signed informed consent to participate in the study. We excluded patients with any other form of diabetes, a duration of diabetes of less than 6 months or with comorbidities that may impact quality of life or affect comprehension of the questionnaire. Once the questionnaires were submitted, we automatically excluded those with more than 3 items left blank or, in the case of the proxy report, those that were not filled out by the main caregiver.
The study was approved by the Ethics Committee of the Hospital de Málaga, which coordinated the project. We calculated that the sample size needed to achieve a precision of 5.3% in estimating a proportion in a normal asymptotic distribution with a 95% confidence interval (bilateral) considering the known prevalence would be of 220 cases, assuming a loss of 15%.
We selected cases randomly and proportionally to the number of eligible patients managed in the paediatric endocrinology clinics of the 6 participating hospitals in Andalusia: Hospital Serranía de Ronda, Hospital General San Agustín (Linares), Hospital Materno-Infantil de Jaén (Jaen), Hospital Materno-Infantil de Jerez (Jerez), Hospital Universitario Virgen Macarena (Seville) and Hospital Materno-Infantil de Málaga (Malaga). We included a specific number of patients from each centre based on the total number managed at the site. We gave the questionnaires to the 3 patients that had the earliest appointments in the clinic in the morning until we obtained the necessary sample size. We also stratified by age group (2–4, 5–7, 8–12 and 13–16 years) to obtain a homogeneous sample based on the actual prevalence of the disease.
QuestionnairesEach patient and/or parent was given 2 questionnaires: the Pediatric Quality of Life Inventory (PedsQL) version 3.0 Type 1 Diabetes Module15 and, to assess adherence to treatment, the Self Care Inventory-Revised Version (SCI-R16). The former is considered the best instrument to assess quality of life in children. There are different versions with the language adapted for age (ages 2–4; 5–7; 8–12 and 13–18). This questionnaire is completed by the patients themselves if they are older than 8 years and otherwise completed by a caregiver. There is no version for children under 2 years. The questionnaire covers a recall period of 7 days and consists of 5 scales with a total of 28 items: diabetes symptoms (11 items), treatment barriers (4 items), treatment adherence (7 items), worry (3 items), and communication (3 items). All items are scored on a 5-point Likert scale ranging from 0 (never) to 4 (almost always). After questionnaires were submitted, we calculated the mean total score and transformed it to a scale from 0 to 100. High scores indicate few problems and therefore a high quality of life.
The SCI-R16 for assessment of adherence was completed by a parent if the patient was aged less than 11 years or by the patient if aged more than 11 years. We analysed the following variables: checking blood glucose levels with a blood glucose meter, checking ketone levels, correct dose of insulin infusion; adherence to adequate carbohydrate portions and reading food labels, response to episodes of hypoglycaemia. The questionnaire comprises 15 items scored on a scale from 1 (never) to 5 (always).
In addition, we collected data on the following:
- -
Demographic characteristics: age at diagnosis, duration of disease, sex and pubertal stage.
- -
Metabolic control (data collected in the electronic health records database during previous follow-up visits): treatment modalities (MDI or CSII), use of flash glucose monitoring systems or integrated real-time continuous glucose monitoring/insulin (RT-CGM/CSII) systems. We assessed the degree of metabolic control based on the mean of the two latest HbA1c measurements, whether capillary or venous. Lastly, we recorded the number of episodes of severe hypoglycaemia (defined as episodes that the patient could not resolve independently and required intervention by a third party) in the past year. We also collected data on episodes of diabetic ketoacidosis, comorbidities and complications of diabetes.
We have expressed continuous variables as mean and standard deviation. We used normality tests and multiple linear regression models with stepwise variable selection and the Akaike information criterion (AIC) for all SCI-R and PedsQL groups and for the SCI-R and PedsQL in the total sample with the purpose of assessing the impact on these scores of changes in the following variables: HbA1c concentration (treated as a continuous variable), presence of complications, treatment with MDI or CSII and others such as current age, number of severe hypoglycaemia episodes or the type of glucose monitoring system used. We defined statistical significance using a confidence level of 95%, considering a p-value of less than 0.05 significant. We used the Spearman correlation coefficient (rho) to assess the correlation between adherence to treatment and quality of life. We interpreted coefficients of 0.1−0.29 indicative of a weak correlation, coefficients of 0.3−0.49 indicative of a moderate correlation, and coefficients of 0.5 or greater indicative of a strong correlation. The statistical analysis was performed with the software R (version 3.5.0).
ResultsSample characteristicsWe selected 220 patients, and the final sample consisted of 178 after exclusion of 42 patients.
In the final sample, 51.1% of the patients were male, the mean age at diagnosis was 6.1 years and the mean age at the time of the study was 10.6 years. The mean duration of disease was 4.7 years, with a duration of more than 5 years in 67% of the patients (Table 1).
Demographic characteristics of the sample.
| Current age (years) | 10.6 (3.62) |
|---|---|
| Median age (min-max) | 11 (2−17) |
| Male sex | 51.1% |
| Continuous subcutaneous insulin infusion (CSII) HbA1c (%)Duration of diabetes (> 5 years)Severe hypoglycaemic episodes | 12.9%7.1 (0.87)4.7 (2.80)67%5.5% |
| Renal complications | 1% |
| Glucose monitoringExclusive capillary measures | 83.2% |
| Flash glucose monitoring | 9.5% |
| RT-CGM | 7.3% |
HbA1c, glycated haemoglobin; RT-CGM, real-time continuous glucose monitoring.
We found that 12.9% of patients used a CSII system. Also, 83.2% monitored glucose levels exclusively through capillary blood measurements, while 16.8% used some form of interstitial glucose measuring device; among the latter, 9.5% used a flash glucose monitoring system (FreeStyle), while 7.3% used integrated RT-CGM/CSII systems. In this sample, all of the latter used Medtronic MiniMed 640 G pumps connected to an Enlite/Guardian sensor, as this was the only system funded by the public health system of Andalusia.
The mean HbA1c level concentration was 7.1%, and 25% of patients had concentrations of 7.5% or higher.
In the sample, 5.5% of the patients experienced severe episodes of hypoglycaemia. Since the disease duration was short, only 1% of patients had renal complications in the form of microalbuminuria, and when it came to comorbidities, 8.4% had coeliac disease and 8.3% autoimmune thyroiditis.
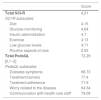
In the analysis concerning adherence to treatment, we found a mean score of 4.21 ± 0.32. The lowest score corresponded to the preventative/routine aspects of care, while the highest scores corresponded to management of low blood glucose levels and the administration of insulin (Table 2). Overall, the SCI-R score was inversely correlated to the HbA1c concentration and to age, although the correlation coefficient was too low to be considered significant (Table 3).
Total and subscale scores of the SCI-R and PedsQL.
| Score | |
|---|---|
| Total SCI-R | 4.21 |
| SCI-R subscales: | |
| Diet | 4.15 |
| Glucose monitoring | 4.64 |
| Insulin administration | 4.7 |
| Exercise | 4.13 |
| Low glucose levels | 4.71 |
| Routine aspects of care | 2.93 |
| Total PedsQL | 72.29 |
| [0,1–2] | |
| PedsQL subscales | |
| Diabetes symptoms | 68.73 |
| Treatment barriers | 77.4 |
| Treatment adherence | 71.9 |
| Worry related to the disease | 64.34 |
| Communication with health care staff | 79.08 |
Results of the regression model with stepwise variable selection for the SCI-R scores by group and for the total sample.
| Coef (SD) | P | |
|---|---|---|
| Diet | ||
| HbA1c | −0.13 (0.05) | .02 |
| Current age | −0.05 (0.01) | < .01 |
| Renal complications | −1.07 (0.41) | .03 |
| Glucose monitoring | ||
| Current age | −0.02 (0.01) | < .01 |
| Insulin administration | ||
| Current age | −0.02 (0.008) | < .01 |
| Exercise | ||
| HbA1c | −0.18 (0.08) | .01 |
| Renal complications | 0.87 (0.14) | .10 |
| Hypoglycaemia | ||
| HbA1c | −0.04 (0.04) | .20 |
| Self-care routine | ||
| Current age | −0.01 (0.01) | .30 |
| Continuous subcutaneous insulin infusion (CSII) | 0.50 (0.13) | < .01 |
| Renal complications | −0.54 (0.37) | .17 |
| Total SCI-R score | ||
| HbA1c | −0.07 (0.03) | .02 |
| Current age | −0.02 (0.007) | < .01 |
| Continuous subcutaneous insulin infusion (CSII) | 0.14 (0.07) | .07 |
| Renal complications | −0.39 (0.21) | .06 |
Coef (SD), coefficient (standard deviation); HbA1c, glycated haemoglobin.
Table 3 shows detailed results of the analysis by dimension of the SCI-R, of which the salient findings were that the HbA1c concentration was correlated to the diet and exercise dimensions and the use of a CSII system was positively correlated to the routine care dimension, the latter being the strongest correlation found in our analysis.
As for the analysis concerning quality of life, the mean total score in the PedsQL was 72.29 ± 8.29. We ought to highlight that we found a direct association with real time continuous glucose monitoring and with a lower number of episodes of severe hypoglycaemia, and that these correlations were strong and only exceeded in strength by the presence of renal complications (a variable that was difficult to assess due to the small number of patients in this subset, although the association was strong) (Table 2). Table 4 presents detailed results for the analysis by subscale. The most salient finding was that the use of the integrated RT-CGM/CSII system was positively correlated to treatment adherence and worry related to the disease, the latter being a strong correlation. Lastly, age was positively correlated to treatment adherence, although this correlation was weak.
Results of the regression model with stepwise variable selection for the PedsQL scores by group and for the total sample.
| Coef (SD) | P | |
|---|---|---|
| Summary of first subscale, diabetes symptoms | ||
| Freq. severe hypoglycaemia | −10.47 (6.83) | .12 |
| Flash vs capillary | −2.265 (2.98) | .44 |
| RT-CGM vs capillary | 7.709 (4.28) | .07 |
| Summary of second subscale, treatment barriers or limitations | ||
| Freq. severe hypoglycaemia | −10.36 (7.53) | .05 |
| Renal complications | 17.75 (9.19) | .17 |
| Summary of third subscale, treatment adherence | ||
| Current age | 0.64 (0.21) | .01 |
| Renal complications | 8.80 (6.04) | .14 |
| Flash vs capillary | −2.19 (2.14) | .81 |
| RT-CGM vs capillary | 8.65 (3.18) | < .01 |
| Summary of fourth subscale, worry related to diabetes | ||
| Freq. severe hypoglycaemia | −22.85 (11.07) | .04 |
| Flash vs capillary | −3.52 (4.83) | .46 |
| RT-CGM vs capillary | 15.02 (6.94) | .03 |
| Summary of fifth subscale, communication with health care providers | ||
| HbA1c | −3.101 (2.13) | .14 |
| Total PEDSQL | ||
| HbA1c | −1.28 (0.88) | .14 |
| Freq. severe hypoglycaemia | −11.60 (5.14) | .02 |
| Renal complications | 14.26 (6.22) | .02 |
| Flash vs capillary | −1.95 (2.23) | .38 |
| RT-CGM vs capillary | 6.52 (3.20) | .04 |
Coef (SD), coefficient (standard deviation); HbA1c, glycated haemoglobin; RT-CGM, real-time continuous glucose monitoring.
We did not find a statistically significant association between adherence to treatment and quality of life assessed by means of the SCI-R and PedsQL scores (Spearman rho, 0.18; P > .05).
DiscussionThis is the first study that analyses quality of life and adherence to treatment in paediatric patients in Andalusia using validated scores like the PedsQL15 and the SCI-R.16
Our results showed high scores in the scale used to assess adherence to treatment, especially in the management of low blood sugar and insulin administration. Our patients being able to adequately correct low glucose levels, knowing how to administer insulin correctly, knowing how to rotate the site of injection and how to adjust the dose suggest that paediatric endocrinology units are educating patients very effectively. The lowest score corresponded to routine care. When we investigated the reason for this, we found that all respondents had replied “never” to the item about carrying a medical alert card.
Patients with lower HbA1c concentrations adhered better to treatment, but the correlation coefficient for this association was low, so we cannot generalize this finding. In any case, it is reasonable to assume that patients with lower HbA1c concentrations were more involved, methodical and thorough in following recommendations On the other hand, we found an inverse association between age and adherence, although once again the correlation was weak, which precludes us from drawing clear conclusions.
We also found high quality of life scores. Although the differences based in the HbA1c concentration were not statistically significant, we found a strong correlation between the use of continuous glucose monitoring (integrated RT-CGM/CSII) and a better quality of life, in spite of having to be connected to the pump continuously and to replace the glucose sensor every 6 days and carry out the necessary calibrations. In clinical practice, only 12.9% of patients used CSII pumps and only 7.3% the integrated RT-CGM/CSII system. We ought to highlight that patients with real time continuous glucose monitoring had a high score in the worry subscale, probably due to these patients being more involved in self-care. Continuous subcutaneous insulin infusion is considered a very effective treatment modality and offers significant benefits to children and adolescents, such as improved glycaemic control, a reduction in the incidence of severe hypoglycaemic episodes and a reduction in the HbA1c concentration.10,17–19 However, despite the evidence, the use of this systems is still not widespread, mainly due to a lack of funding from health care systems and the scarcity of health professionals trained in their use.17
These systems have been proven to reduce the frequency of severe hypoglycaemia,17 to which we ought to add that the reduction in the frequency of these episodes was associated to a better quality of life in our sample. All of the above leads us to believe that these new treatment modalities should be used more frequently.20,21
A multicentre study conducted in Spain in 20141 in patients with T1D aged less than 18 years assessed quality of life in 267 patients throughout the country. The characteristics of the sample were very similar to those of the sample in our study, with a mean age of 11 years, a median duration of diabetes of 5 years, 53.2% male patients and a mean HbA1c concentration of 7.4 (SD, 0.9). Patients were stratified based on their HbA1c concentration (≥ 7.5% vs < 7.5%). The authors found a mean PedsQL score of 71.6 (SD, 12.9), which was very similar to the score in our sample (72.29 ± 8.29).
Other relevant studies include the Global TEENs Study,22 published in 2017, or the study conducted in 2019 in the Community of Madrid,23 which also assessed quality of life using the PedsQL 3.0 module. One limitation is that the first also included adult patients, with an age range of 8–25 years. Some of their salient findings were a lower quality of life in female patients and in the group aged 18–25 years. Both studies concluded that patients with better metabolic control had a better quality of life.23
We ought to mention that in our study, dividing patients based on whether they had good control (HbA1c < 7.5%) or poor control (>7.5%) was a considerable limitation, as most patients maintained good glycaemic control and thus the proportion corresponding to the “poor control” group was not significant. For this reason, we used the HbA1c concentration as a continuous variable, finding a correlation between greater HbA1c concentrations and lower scores in treatment adherence and quality of life. Ideally, more reliable parameters should be used, such as changes in blood glucose or the time within the target range, the time in hyperglycaemia and the time in hypoglycaemia, although this would require all patients to use a continuous interstitial glucose monitoring system. At present, funding has already been allocated to discontinuous blood glucose monitoring in the paediatric population in Andalusia, so it would be very interesting to continue this line of research.
Among the limitations of the study, we ought to highlight that despite a large initial sample size (220 patients), the final analysis only included 178 patients due to poor questionnaire completion. It would probably have been better to make a point of explaining how to correctly complete them. Another limitation was that we could not include children aged less than 2 years because there is no version of the PedsQL for this age group. In terms of the sample, there may have been selection bias, for while patients were selected by chance, those who did not attend the visits had no chance of being selected and were likely to have poorer glycaemic control.
Despite these limitations, we believe that the findings of this study are fairly representative of quality of life and adherence to treatment in the paediatric population with T1D in Andalusia.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Casaño MA, Del Mar Alonso Montejo M, Gea IL, Manuel Jiménez Hinojosa J, Mata MAS, Macías Fet al. Estudio de calidad de vida y adherencia al tratamiento en pacientes de 2 a 16 años con diabetes mellitus tipo 1 en Andalucía. An Pediatr (Barc). 2021;94:75–81.