The following of a strict gluten-free diet (GFD) is essential in the control of coeliac disease. The aim of this study was to determine the adherence to a GFD in coeliac patients and to evaluate the factors that could influence this adherence.
Material and methodsA descriptive observational study was carried out, in which gluten immunogenic peptides (GIP) were determined in faeces using a semi-quantitative method, and the Coeliac Dietary Adherence Test was completed. Sociodemographic and clinical details were collected, and an ad hoc questionnaire was prepared.
ResultsOf the 80 patients included, 92.5% were adherent according to the GIP and 86.3% according to Coeliac Dietary Adherence Test (acceptable agreement; Kappa: 0.31, P = .004). The large majority (83.3%) of patients with positive GIP gave negative anti-transglutaminase antibodies in the latest determination. Current age and time of onset were significantly associated with adherence. Those with a positive GIP had a mean age of 5 years more (P = .0001) and were 52 months more on a GFD (P = .025). One quarter of those surveyed considered the diet difficult to follow. Just under two-thirds (60%) considered that the variability in the eating site was an important factor in leading to infringements, with children’s parties being the main area where they occurred (66.7%). The lack of variety (61.4%) and the increased cost (98.6%) of gluten-free foods is highlighted.
ConclusionsThe adherence to the GFD is generally good. The analysis of GIP helps to detect non-adherent patients that would pass unnoticed in other circumstances. Measures must be established in order to maintain good long-term adherence, taking into account the risk factors and difficulties detected.
La realización estricta de una dieta sin gluten (DSG) es fundamental para el control de la enfermedad celiaca. El objetivo del estudio fue analizar la adherencia a la DSG en celiacos y evaluar factores que pudieran influir en la misma.
Material y métodosEstudio observacional descriptivo. Se realizó una determinación de péptidos inmunogénicos del gluten (GIP) en heces con método semicuantitativo y se cumplimentó el cuestionario Celiac Dietary Adherence Test. Se recogieron datos sociodemográficos, clínicos y se elaboró una encuesta ad hoc.
ResultadosSe incluyeron 80 pacientes. El 92,5% eran adherentes mediante GIP y 86,3% con Celiac Dietary Adherence Test (concordancia aceptable; Kappa: 0,31, p = 0,004). El 83,3% de los pacientes con GIP positivos tenía la última determinación de anticuerpos antitransglutaminasa negativos. La edad actual y el tiempo de evolución se asociaron significativamente con la adherencia. Aquellos con GIP positivos tenían de media 5 años más (p = 0,0001) y llevaban 52 meses más de DSG (p = 0,025). Una cuarta parte de los encuestados consideraba difícil realizar la dieta. El 60% consideraba que la variabilidad en el lugar de comida era importante para inducir transgresiones, siendo las fiestas infantiles el principal lugar donde sucedían (66,7%). Se destaca la escasa variedad (61,4%) y el elevado coste (98,6%) de los alimentos sin gluten.
ConclusionesLa adherencia a la DSG es en general, buena. El análisis de GIP permitió detectar a pacientes no adherentes que en otras circunstancias pasarían desapercibidos. Se deben establecer medidas para mantener una buena adhesión de manera prolongada, considerando los factores de riesgo y dificultades detectados.
Coeliac disease (CD) is the most frequent chronic gastrointestinal disorder in Western countries. At present, the only effective treatment is adhering to a lifelong gluten-free diet (GFD).1
The results of studies that analyse adherence to GFD are very heterogeneous, which may be due to differences in definitions and methods used for evaluation.2 Adherence can be affected by different factors such as age, age at diagnosis, sex, duration of disease, availability and cost of gluten-free products, access to dieticians and CD associations and product labelling.3,4 Poor adherence can result in poor symptom control and an increased risk of gastrointestinal cancer.5,6
Assessing adherence is not a simple task. Commonly used approaches to monitor adherence include clinical evaluations, serological tests, biopsy examinations and questionnaires.7 One widely used instrument is the Celiac Disease Adherence Test (CDAT), which assesses factors such as perceived self-efficacy, motivation for adherence, associated symptoms, knowledge of the disease, risk behaviours and subjective perception of adherence.8,9 This questionnaire, like other instruments used historically, identifies the consequences of continued exposure to gluten, but does not detect exposure itself. It is known that occasional minor exposures, frequently resulting from cross-contamination or lack of awareness, may trigger autoimmune mechanisms and cause oxidative stress, chronic inflammation and histological damage.1
Tests for detection of gluten immunogenic peptides (GIPs) are a recently described method that allows early identification of the consumption of small amounts of gluten.10–12 These peptides are small protein fragments that resist digestion and are partly excreted in the faeces, and account for most of the immunotoxic reactions to gluten. They interact with the immune system of patients with CD, triggering a response against a variety of antigens.13
Gluten immunogenic peptides can be detected in stools between day 2 and 7 after ingestion12 and can also be detected in urine. There is a correlation between the amount of gluten consumed and the amount of GIP excreted in the faeces. The detection of GIPs also appears to correlate to future histological damage.13
The primary objective of our study was to assess the adherence of patients with CD to a GFD through the measurement of GIP levels in stool and the administration of a questionnaire, and the secondary object was to analyse potential factors associated with adherence.
Material and methodsWe conducted an observational descriptive study. The study period went from January 1 to December 31, 2018. We included patients with CD diagnosed based on the classic criteria14 or the 2012 criteria of the European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN)15 that had been following a GFD for at least 1 year and managed at the Gastroenterology and Nutrition Unit of a tertiary care university hospital. We excluded patients with a final diagnosis of non-coeliac gluten sensitivity and patients lost to follow-up.
Study designWe reviewed the health records to obtain data on the diagnosis and follow-up of CD. We collected data on the following sociodemographic variables: residential setting (rural or urban, defined based on a threshold of 5000 inhabitants), parental educational attainment (no education, primary education, secondary education, university degree), socioeconomic status (middle–low, middle–high) and family history of CD.
We collected the most recently recorded anti-tissue transglutaminase (tTG) antibody levels, measured by the standard laboratory technique (chemiluminescent immunoassay). We considered values of anti-tTG of less than 10 U/mL negative.
Patients collected from 2 to 4 g of faeces the day before visiting the hospital and kept them refrigerated at home, following the directions of the test manufacturer. The day of the visit, the stool samples were submitted to the biobank of the hospital, where they were stored at a temperature of −80 °C until 24 h before testing. The samples were tested with the iVYCHECK GIP stool® immunochromatographic assay. This assay uses monoclonal antibody G12, which selectively binds peptide 33-mer, the most immunodominant peptide in individuals with CD. Since this is a semiquantitative test, the possible results are positive (>0.3 µg de GIP/g stool) or negative.
The legal guardians of the patient completed the CDAT questionnaire at the time of the stool sample collection. It comprises 7 items scored on a scale from 1 to 5 (minimum possible score, 7; maximum, 35). Scores of less than 13 indicate good adherence. The CDAT is a clinically relevant and easy to use tool that allows standardised evaluation.8
A questionnaire specifically designed for the study was completed, too, which asked close-ended questions about factors related to adherence to GFD, satisfaction with gluten-free food and the sources of information used by families (Table 1). We classified patients based on their satisfaction with gluten-free foods into 2 groups: dissatisfied (very dissatisfied/dissatisfied/hardly satisfied) and satisfied (satisfied/very satisfied).
Adherence questionnaire.
| Item | Answer choices |
|---|---|
| Is it hard to follow the diet? | Yes |
| No | |
| In case you consider it hard, check the main reason | Financial |
| Dislikes gluten-free diet | |
| Craves forbidden foods | |
| Does not know which foods are allowed | |
| Which is the setting where the most transgressions occur? | School |
| Home | |
| Grandparent home | |
| Home of a different relative | |
| Birthdays and parties | |
| Which do you think is the strongest contributor to poor adherence? | Financial concerns |
| School cafeteria | |
| No benefit from GFD | |
| Insufficient information | |
| Restaurants | |
| Comorbidities | |
| Insufficient understanding | |
| Eating in different places | |
| Limited availability | |
| Degree of satisfaction with each characteristic of gluten-free foods: | 1. Very dissatisfied |
| 2. Dissatisfied | |
| Taste | 3. Little satisfied |
| Texture | 4. Satisfied |
| Variety | 5. Very satisfied |
| Price | |
| What are your sources of information? | Books |
| Relatives | |
| Other people with CD | |
| CD associations | |
| Nutritionist | |
| Internet | |
| PC physician |
PC, primary care.
We used the median and interquartile range (IQR) to describe quantitative variables. We described categorical variables using percentages. We assessed the normality of the distribution of quantitative variables by means of the Kolmogorov–Smirnov test. We used the chi square test to compare proportions. Medians were compared with the t test for independent samples or the Mann–Whitney U test as applicable based on the distribution. We used the kappa index to assess concordance. We defined statistical significance as a p-value of less than 0.05. The statistical analysis was performed with the software SPSS version 22.
Funding and ethical considerationsThe study was approved by the Ethics Committee of the Hospital Universitario Central de Asturias (file no. 31/18). We obtained informed consent from every participant.
ResultsThe initial selection included 168 patients. We excluded 17 (9 without CD, 7 with non-coeliac gluten sensitivity, 1 with gluten allergy). Another 38 did not participate (we were unable to contact 17, 6 had moved, 15 refused) and 33 were excluded because they did not provide a stool sample. The final sample included 80 patients (39 male, 41 female), with a median age at time of enrolment in the study of 10.85 years (IQR, 7.64). The median age at diagnosis was 24 months (IQR, 18). Anti-tTG values were elevated at diagnosis in 73 patients (median anti-tTG, 126 U/mL; IQR, 93.5). Patients had been on a GFD for a median of 81.5 months (IQR, 84). Table 2 summarizes the sociodemographic characteristics of the patients, and Table 3 the clinical characteristics.
Sociodemographic characteristics.
| Patients (n) | Percentage (%) | |
|---|---|---|
| Total | 80 | 100 |
| Usual residence | ||
| Urban setting | 65 | 81.3 |
| Rural setting | 14 | 17.5 |
| Did not answer | 1 | 1.2 |
| Parental educational attainment | ||
| No education | 0 | |
| Primary | 7 | 8.7 |
| Secondary | 27 | 33.7 |
| University | 45 | 56.3 |
| Did not answer | 1 | 1.3 |
| Socioeconomic status | ||
| Middle–low | 20 | 25 |
| Middle–high | 57 | 71.2 |
| Did not answer | 3 | 3.8 |
| Relatives with CD | ||
| None | 49 | 61.3 |
| Father | 1 | 1.2 |
| Mother | 6 | 7.5 |
| Sibling | 9 | 11.3 |
| Did not answer | 15 | 18.7 |
Clinical characteristics.
| Presentation | Patients (n) | Percentage (%) |
|---|---|---|
| Classic | 58 | 76.3 |
| Latent/oligosymptomatic | 22 | 23.7 |
| Symptoms at diagnosis | ||
| Failure to thrive | 39/74 | 52.7 |
| Diarrhoea | 37/74 | 50 |
| Classic CD symptoms | 32/74 | 43.2 |
| Vomiting | 12/74 | 16.2 |
| Anorexia | 9/74 | 12.2 |
| Diagnostic tests | ||
| Genetic + serological tests | 73/77 | 94.8 |
| Duodenal biopsy | 33/77 | 42.9 |
| Gluten challenge | 3/76 | 3.9 |
| Abnormal findings at diagnosis | ||
| Ferropenia | 23/74 | 31.1 |
| Iron-deficiency anaemia | 9/74 | 12.2 |
| Hypertransaminasaemia | 10/74 | 13.5 |
| Steatorrhea | 3/74 | 4.1 |
| Genetic variants | ||
| DQ2 0501* and DQ2* 0201 | 58/64 | 90.6% |
| DQ2 0501* | 4/64 | 6.3% |
| DQ2* 0201 | 1/64 | 1.6% |
| DQ8 | 3/64 | 4.7% |
| Comorbidities | ||
| Atopic dermatitis | 8/78 | 10.3 |
| Diabetes mellitus | 1/78 | 1.3 |
| Thyroid disorder | 2/78 | 2.6 |
| Hepatitis | 1/78 | 1.3 |
| Arthritis | 0/78 | |
| Dermatitis herpetiformis | 0/78 | |
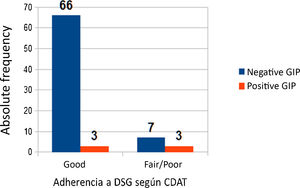
The results of the GIP test were negative in 74 patients (92.5%). Based on the CDAT, 69 (86.3%) exhibited good adherence and 10 poor adherence. Of the 69 patients with good adherence, 3 had a positive GIP test. On the other hand, of the 10 patients with poor adherence, 7 had negative GIP tests (kappa, 0.31, P = .004) (Fig. 1).
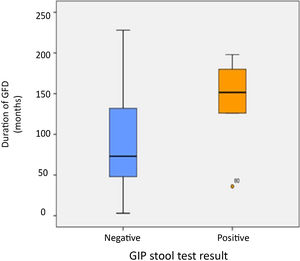
We found that adherence based on the GIP test results was significantly associated with age and duration of disease. Patients with positive GIP tests were 5 years older, on average, than patients with negative results (P = .0001). All patients with positive GIP results were aged more than 13 years. In addition, patients with positive GIP results had been following a GFD for a median of 52 months longer compared to patients with negative results (P = .025) (Fig. 2). When it came to anti-tTG antibodies, 83.3% of patients with positive GIP results had negative anti-tTG results, while 2.9% of patients with negative GIP results had positive anti-tTG results. We did not find an association between adherence and age at diagnosis or adherence and the sociodemographic characteristics under study (Table 4).
Analysis of association of study variables with adherence.
| GIP + | GIP − | P | |
|---|---|---|---|
| Age (years) | 15.25 (IQR, 3.5) | 9.85 (IQR, 7.6) | .0001 |
| Duration of disease (months) | 140.5 ± 58.31 | 88.82 ± 52.88 | .03 |
| Age at diagnosis (months) | 41.5 ± 44.51 | 31.8 ± 25.06 | .4 |
| Sex (male) (n) | 3/17 (17.6%) | 14/17 (82.4%) | .7 |
| Sex (female) | 3/12 (25%) | 9/12 (75%) | |
| Residential setting (urban) (n) | 5/5 (100%) | 60/74 (81.1%) | .6 |
| Residential setting (rural) | 0/5 | 14/74 (18.9%) | |
| Does not understand diet (yes) (n) | 1/6 (16.7%) | 5/6 (83.3%) | .4 |
| Does not understand diet (no) | 4/54 (7.4%) | 50/54 (92.6%) | |
| Information from association (yes) (n) | 4/41 (9.8%) | 37/41 (90.2%) | .7 |
| Information from association (no) | 2/33 (6.1%) | 31/33 (93.9%) | |
| Information from dietitian (yes) (n) | 1/11 (9.1%) | 10/11 (90.9%) | 1 |
| Information from dietitian (no) | 5/63 (7.9%) | 58/63 (92.1%) | |
| Presentation (classic) (n) | 5/6 (83.3%) | 53/70 (75.7%) | 1 |
| Presentation (other) | 1/6 (16.7%) | 17/70 (24.3%) | |
| Socioeconomic status (middle–low) (n) | 3/5 (60%) | 17/72 (23.6%) | .1 |
| Socioeconomic status (middle–high) | 2/5 (40%) | 55/72 (76.4%) | |
| Satisfaction with gluten-free foods (yes) (n) | 1/19 (5.3%) | 18/19 (94.7%) | 1 |
| Satisfaction with gluten-free foods (no) | 4/51 (7.8%) | 47/51 (92.2%) | |
| Parents with university education (n) | 1/5 (20%) | 44/74 (59.5%) | .2 |
| Parents without university education | 4/5 (80%) | 30/74 (40.5%) | |
| First-degree relative with CD (yes) (n) | 0/16 | 16/16 (100%) | .3 |
| First-degree relative with CD (no) | 5/49 (10.2%) | 44/49 (89.8%) |
CD, coeliac disease; GIP, gluten immunogenic peptide.
Table 5 presents the main challenges to following a GFD and the main setting of transgressions from the GFD. Some of the factors that could be important contributors to poor adherence were variations in eating setting (eating in different places, n = 16; eating in restaurants more than twice a week, n = 13; school lunchroom, n = 10), financial concerns,11 insufficient information,6 insufficient understanding5 or limited availability.4 None of the participants reported absence of benefits from the GFD or comorbidities as important factors.
Barriers to following a gluten-free diet and setting of transgressions.
| Parents | Children | |
|---|---|---|
| Barriers to adhering to GFD | ||
| Found the GFD difficult | 16 (21.1%) | 18 (25.7%) |
| Financial reasons | 10 (71.4%) | 2 (11.8%) |
| Dislikes allowed foods | 2 (14.3%) | 3 (17.6%) |
| Craves prohibited foods | 2 (14.3%) | 8 (47.1%) |
| Does not know which foods are allowed | 4 (23.5%) | |
| Setting of transgressions from GFD | ||
| Birthday parties | 20 (80%) | 21 (75%) |
| School | 2 (8%) | 5 (17.8%) |
| Grandparent’s home | 2 (8%) | 1 (3.6%) |
| Relative’s home | 1 (4%) | 1 (3.6%) |
GFD, gluten-free diet.
When it came to the gluten-free foods, 21 patients were dissatisfied and 48 satisfied with the taste, 31 were dissatisfied and 39 satisfied with the texture, 43 dissatisfied and 27 satisfied with the variety, and 69 dissatisfied and 1 satisfied with the price. Eighty percent of patients with a positive GIP test were dissatisfied with the taste, texture or variety of gluten-free foods.
The most frequently used sources of information were the internet (48) and CD associations (41). Other reported sources were books,25 other patients with CD,24 physicians, 20 relatives16 and dietitians.11
DiscussionIn our study, we assessed adherence using GIP tests and the CDAT. Overall, we found good adherence of patients to the GFD. The agreement between the 2 methods under study was acceptable.
The reported proportion of good adherence ranges between 40% and 92% in different studies.16 The selection of the method for monitoring adherence must be based on its accuracy, invasiveness, time and cost of each, taking into account the limitations of the available options. Endoscopy with biopsy examination could be considered the gold standard for assessing the condition of the mucosa, but it is invasive and costly.1 Clinical improvement usually reflects good adherence, but cannot be applied to patients that are identified through screening and are asymptomatic at the time of diagnosis.16,17
In many countries, the dietitian is responsible for the follow-up, performed through a clinical interview, a method deemed objective and non-invasive. The limitation of this approach is that it is not standardised, which limits its precision, reproducibility and comparability. Furthermore, there is a scarcity of dietitians, and the self-reporting of adherence reduces the accuracy of the assessment.18 Leffler et al. consider this method adequate for detection of unintentional gluten consumption.8 Other authors have reported a high correlation to mucosal changes.19 The British Society of Gastroenterology recommends seeing a dietitian at diagnosis and subsequently at least once a year.20
Questionnaires are useful tools but there are few of them, they are subjective and none is adapted to Spanish save for the CDAT, the translation of which has been validated.9 This questionnaire has exhibited good sensitivity and specificity in comparison with standard methods. Leffler et al. consider its performance superior to anti-tTG testing. In our study, 86.3% (69/89) of patients adhered to the GFD based on the CDAT, and the questionnaire was highly acceptable and easy to perform. Although the agreement between the CDAT and the GIP stool test was acceptable, we observed that half of the patients with a positive GIP test had good adherence based on the CDAT. Similar results have been found in other studies, like the one by Comino et al.,21 in which 79% of participants had good adherence based on questionnaire results and 69.2% of patients with a positive GIP test result reported adhering to the GFD based on the questionnaire responses.
A low percentage of patients with negative GIP tests (2.9%) had positive anti-tTG results, which could correspond to false negative results in the GIP test. Different studies have reported a sensitivity for this test ranging from 7522 to 95%.23 The possibility that the discrepancy is due to false positive results in the antibody test is less likely, as the specificity of the antibody test is of nearly 100%.15,24
Serological testing is the most frequently used method to date, although the correlation between the normalization of antibody levels and clinical and histological recovery is not always good. In some cases, antibody levels do not normalise despite adherence to the diet on account of their long half-life and because they reflect immune activity rather than mucosal damage.19 In addition, serological tests may fail to detect occasional exposure.25 On the other hands, there are patients with mucosal damage that have normal serological test results.1 All the patients in our study met the diagnostic criteria for CD, yet anti-tTG values at diagnosis were only elevated in 73 patients. Moreno et al.13 reported a significant association between GIP levels and the severity of histological changes but did not observe an association between mucosal recovery and serological test results. Therefore, a normal anti-tTG test result is not reliable for assessing adherence.1
Detection of GIPs helps identify gluten intake/transgressions earlier than other methods, such as serological testing.23 Two methods are used to measure GIP levels: quantitative ELISA and semiquantitative rapid testing by means of immunochromatography, the latter of which we used in our study. Several studies have previously used this marker to estimate adherence, generally finding percentages of adherence between 70.2% and 84%.21,23 In our study, 92.5% of patients exhibited adherence based on this method.
Measurement of GIP levels can detect transgressions that would go undetected with serological tests.21,26,27 More than 80% of patients with a positive GIP test in our study had negative anti-tTG tests, a percentage that was similar to that reported in previous studies (71%21 and 73%27). These results highlight the ineffectiveness of anti-tTG antibodies in detecting isolated transgressions.
Knowing the different factors that affect adherence is essential to the development of interventions aimed at improving it.5 The literature describes a decrease in adherence with increasing age,3,21,26,28 probably attributable to a greater degree of supervision in patients of younger age. It also describes poorer adherence in association with greater age at diagnosis6 and male sex.26,29 In our study, we found poorer adherence in older patients, but did not find an association with age at diagnosis or sex.
Many authors have described poorer adherence with increasing duration of disease.6 The studies conducted by Comino et al. have found a higher frequency of transgression in patients that had been longer on a GFD.21,26 In opposition, other authors have found poorer adherence in patients that had been on the GFD for less than 3 years.29 In our study, we found that patients with transgressions had been on the GFD for nearly 4.5 more years compared to patients that did not.
Socioeconomic status seems to have an impact as well, as the price of gluten-free products is higher.6 Based on the 2019 report on the price of gluten-free products of the Federación de Asociaciones de Celiacos de España (Federation of Coeliac Disease Associations of Spain), there is an average difference of 935.46 euro/year between buying gluten-containing and gluten-free products. Medical prescription has been proposed as a factor that could facilitate adherence,4,5 as it could lower the out-of-pocket costs for families of patients with CD. Reduced access to gluten-free foods could hinder adherence in rural areas, despite the considerable increase in the distribution of these products in recent years. In ours study, all patients that reported transgressions lived in urban areas, and 60% were of middle/low socioeconomic status.
To obtain more information about adherence, we specifically developed another questionnaire. We selected for inclusion the items that seemed most relevant after reviewing the existing literature on the subject. Approximately one fourth of respondents considered adherence to the GFD challenging. Parents most frequently reported financial reasons for it, and children the craving of forbidden foods. The same reasons have been described by other authors. One study found that most respondents considered the GFD difficult to follow (70% of parents and 82.5% of children), and one of the most frequent reasons children gave for it was not knowing what they could eat.30 Other reasons previously described included unpleasant taste, transgression associated with being asymptomatic or that the restrictions did not compensate for the benefits.5,6
Some of the factors that seem to be the main contributors to poor adherence are difficulty in finding gluten-free products, the small range of products, difficulty interpreting food labels and financial concerns.3–5 In our study, the factor mentioned most frequently was a change in the setting of food consumption, followed by financial concerns and, less frequently, a lack of availability, information or understanding. Although some authors have reported that the main setting of transgressions is the home,30 the findings of other authors were in agreement with ours, as non-adherence mainly occurred outside the home.31
In regard to the sensory properties and cost of gluten-free foods, a large portion of the patients reported dissatisfaction with the price or variety of these products but being satisfied with their taste and texture. These variables have been analysed in different populations with similar results.31
When it comes to the sources of information, the literature shows significant heterogeneity. In our study, as was the case in others, the most important sources used were the internet and CD patient associations,4,5 in addition to books and other individuals with CD. Fewer patients mentioned physicians or dietitians, who are the main sources of information reported in other studies.30,32
The limitations of this study include its retrospective design, the small sample size and it being conducted in a single centre, which reduces its external validity and precludes the generalization of its results. In addition, there was a considerable loss to follow-up, which could have resulted in selection bias and compromised the validity of the results, as more motivated or better-adhering individuals could have participated in greater numbers. Another important aspect is that patients knew when they were going to collect stool samples, which may have led to intentional avoidance of transgressions. However, since this method has only been introduced recently in our setting, it is likely that its impact on the avoidance of transgressions is no different from the impact of having an upcoming follow-up appointment.
Our study assessed a method used to detect short-term GFD transgressions that can be complementary to traditionally used tests evaluating adherence in the long term. The GIP stool test allows identification of non-adhering patients that would otherwise go undetected. The high cost of gluten-free food products (parents) and the craving for forbidden foods (children) were factors identified by participants as important contributors to poor adherence. The main reason for transgressions was changes in the setting where food was consumed, with children’s parties being the main setting for GFD transgressions. These factors should be taken into account in the long-term followup of these patients.
FundingThe study was partially funded with a grant from "Fundación Nutrición y Crecimiento".
Conflicts of interestThe authors have no conflicts of interest to declare.
Previous presentations: “Estudio de la adherencia terapéutica a la dieta sin gluten en pacientes celiacos”, presented at the XXVI Congress of the SEGHNP, May 16–18, 2019 in Santander, Spain; and the IX Workshop on Paediatric Gastroenterology and Nutrition, October 4–5, 2019 in Ribadesella, Spain.
“Análisis de la calidad de vida relacionada con la salud en pacientes celiacos”, XXXII Memorial Guillermo Arce y Ernesto Sánchez-Villares, November 15–16, 2019.
Please cite this article as: Fernández Miaja M, Díaz Martín JJ, Jiménez Treviño S, Suárez González M, Bousoño García C. Estudio de la adherencia a la dieta sin gluten en pacientes celiacos. An Pediatr (Barc). 2021;94:377–384.