Visceral leishmaniasis (VL) is a zoonosis that can be caused by more than 20 species, including Leishmania donovani and Leishmania infantum, which are endemic to the Mediterranean basin.1
The paediatric population and immunocompromised individuals are at highest risk of this disease.2,3
The prolonged incubation period and nonspecific clinical manifestations of VL pose challenges to its diagnosis, which may result in delayed diagnosis and an increase in morbidity and mortality.
Thus, we hypothesised that given the suspicion of VL, performance of an abdominal ultrasound scan could be helpful, as the presence of splenic nodules (SNs) could be indicative of this disease.4–6
We conducted a retrospective longitudinal single-centre observational and analytical study. We collected data on demographic, clinical and laboratory variables for the period between January 2012 and December 2019 in a tertiary care children’s hospital in a highly endemic region, including very patient aged less than 15 years with a diagnosis of VL, and performing a comparative analysis with the statistical software SPSS® version 25.0 based on whether or not they had SNs.
During the study period, VL was diagnosed in 20 patients, of who 45% (n = 9) had SNs.
Since the aim of the study was to characterize the group of patients with SNs, we describe the main findings in this group, and summarise the results for the main clinical variables in both groups in Table 1.
Demographic, clinical and laboratory data.
| Variable | With SNs (n = 9) | No SNs (n = 11) | P |
|---|---|---|---|
| Median (IQR) or n (%) | Median (IQR) or n (%) | ||
| Age at diagnosis (months) | 8 (4−60) | 21 (5−156) | .038 |
| Sex (male) | 5 (55.6%) | 5 (45.5%) | 1 |
| Sex (female) | 4 (44.4%) | 6 (54.5%) | 1 |
| Rural setting | 8 (88.9%) | 5 (45.5%) | .07 |
| Contact with dogs | 7 (77.7%) | 4 (36.3%) | .07 |
| Fever (days) | 12 (8−20) | 14 (5−30) | .824 |
| Length of stay (days) | 8 (6−20) | 14 (5−30) | .056 |
| Haemophagocytic syndrome | 3 (33.3%) | 5 (45.5%) | .670 |
| Hepatomegaly | 8 (88.9%) | 7 (63.6%) | .31 |
| Lymph node enlargement | 2 (22.2%) | 1 (9.1%) | .56 |
| Elevation of C-reactive protein (mg/L) | 27.29 (2.53–74–8) | 88 (17.48−170) | .031 |
| Minimum haemoglobin (g/dL) | 8.80 (5.30−9.50) | 7.0 (5.60−9–90) | .88 |
| White blood cells (per mm3) | 4180 (2680−8430) | 2800 (670−6400) | .075 |
| Lymphocytes (per mm3) | 2980 (1530−8000) | 1795 (260−3300) | .045 |
| Platelets (per mm3) | 96 000 (64 000−201 000) | 60 000 (16 000−129 000) | .056 |
IQR, interquartile range; SN, splenic nodule.
P values of less than 0.05 are presented in boldface.
We found a slight predominance of male versus female patients (55.6% vs 44.4%); 88.9% of the patients resided in rural areas, 77.7% had had contact with dogs and 75% had spent time in the countryside. None of the patients had comorbidities.
From a clinical perspective, we ought to highlight that all patients presented with the classic triad of fever, cytopenia and splenomegaly. In addition, the physical examination revealed hepatomegaly in 88.9% of the patients and lymph node enlargement in 22.2%.
As concerns the blood counts, 100% of patients presented with anaemia, with a median haemoglobin (Hb) concentration of 8.80 g/dL (IQR, 5.30–9.50), and 22.2% required transfusion of packed red blood cells. Other types of cytopenia detected in the sample were neutropenia (77.8%) and thrombocytopenia (88.9%).
In 100% of cases, leishmaniasis was diagnosed based on serological testing. A bone marrow aspirate sample was obtained only in 2 patients, with the PCR test detecting L. infantum in one of them and visualization of the amastigote form of the parasite in the microscopic examination in the other case. In 2 other patients, the workup included PCR testing of peripheral blood for detection of Leishmania, which was negative in both.
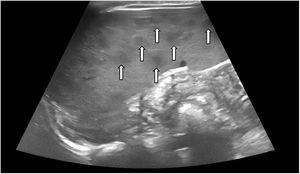
Every patient underwent an abdominal ultrasound scan at admission, which evinced splenomegaly and multiple multifocal hypoechoic subcentimetre nodular lesions (Fig. 1). The time elapsed to resolution of SNs ranged from 2 to 20 months.
Treatment consisted in intravenous administration of liposomal amphotericin B liposomal at a dose of 4 mg/kg/day for 5 days and a sixth dose on day 10, which achieved a favourable response. Secondary haemophagocytic syndrome developed in 33.3% of the patients, which was diagnosed based on the fulfilment of a minimum of 5 clinical or laboratory criteria (cytopenia, splenomegaly, hypertriglyceridemia, fibrinogen < 1.5 g/L, ferritin > 500 μg/L, elevation of soluble CD25, haemophagocytosis in the bone marrow). None of the patients required admission to the intensive care unit. None of the patients experienced relapse and there were no deaths.
As regards statistically significant differences between the groups, we found a lower age in the group with SNs, with a median age of 8 months (IQR, 4−60 months) compared to 21 months in the group without SNs (IQR, 5−156 months) (P = .038). We also found higher lymphocyte counts (P = .045) and lesser elevation of C-reactive protein with a median level of 27.29 mg/L in the group with SNs (IQR, 2.53−74.8) compared to 88 mg/L in the group of patients without SNs (IQR, 17.48−170) (P = .038) (Table 1).
Given how challenging the diagnosis of VL proves to be in some cases, performance of abdominal ultrasound for detection of SNs should be considered to guide the diagnosis.4–6 However, it is important to be aware that these lesions are not pathognomonic of VL, and that the differential diagnosis, depending on the context, must rule out the possibility of metastasis, haematomas, cavernomas, infarction, lymphomas and abscesses.4–6
The use of other imaging techniques, such as CT, MRI or PET/CT has been studied5 and not found to be superior compared to ultrasonography, while entailing drawbacks such as exposure to radiation or the need of sedation in paediatric patients.4
Our study constitutes the largest case series of patients with VL and SNs described to date. In conclusion, we believe that the sonographic detection of splenic nodules in patients with clinical and laboratory features suggestive of VL, such as fever, splenomegaly and cytopenia, could be very useful, although microbiological tests are always required to confirm the diagnosis.
Please cite this article as: Casero-González MM, Izquierdo-Palomares L, Cañuelo-Ruiz O, Montero-Yéboles R, de la Torre-Aguilar MJ, Ruiz-Sáez B. Nódulos esplénicos como signo guía de leishmaniasis visceral en población infantile. An Pediatr (Barc). 2022;97:66–68.