Sickle-cell disease is one of the most frequent inherited diseases, and its prevalence is growing in Spain due to immigration.1 The term “sickle cell” refers to the distorted crescent shape that red blood cells (RBCs) develop due to the polymerization of their atypical form of haemoglobin, haemoglobin S, which results from a point mutation in the haemoglobin beta gene. The distorted shape of the RBCs and their interaction with other blood cells, plasma factors and the vascular endothelium cause their destruction and obstruction of small vessels, producing inflammation and ischaemia.2 This can lead to various complications, acute and chronic.
One of the most frequent and severe complications is acute chest syndrome (ACS), which is the second leading cause of admission in affected individuals and is associated with significant morbidity and mortality. It is a form of acute lung injury caused by lung infarction and inflammation with or without atelectasis possibly associated with respiratory infection.3
For more than 20 years, hydroxyurea (HU) has been used as a disease-modifying treatment. It has been found to reduce the frequency of pain episodes in these patients in addition to other acute complications, including ACS.4 However, studies have not been performed to determine whether it can modify the course of ACS, reducing the severity of the episodes.
We conducted a study to analyse whether chronic treatment with HU had an impact on the severity of ACS episodes requiring admission in our hospital.
We conducted a retrospective study of ACS episodes in paediatric patients (aged 0-17 years) with sickle cell disease managed between 1987 and 2019 in a secondary care hospital in the Community of Madrid, Spain. The collection and analysis of data on patients with sickle cell disease (all of them included in the nationwide REHem register) was approved by the ethics committee of the hospital, the Department of Child Protection and the Spanish Agency on Data Protection, and was promoted by the Sociedad Española de Hematología y Oncología Pediátricas (Spanish Society of Paediatric Haematology and Oncology, SEHOP) The statistical analysis was performed with the software SPSS® version 25.
The study included 64 episodes of ACS in 23 of the 48 patients with sickle cell disease managed at the hospital. The median duration of follow-up was 36 months (range, 0-216 meses). The median age at the time of the episode was 3.7 years (range, 0.8-16.8). Each patient experienced a median of 2 episodes (range, 1-9). In 26.6% of the episodes, the patient was being treated with HU, but we only considered it actual treatment in 20.3% of the total (n = 13), as we excluded from this count patients that did not appear to adhere to the treatment because they had not exhibited any significant increase in the mean corpuscular volume. The median time elapsed from initiation of treatment with HU to the first episode of ACS was 6 months.
We conducted a comparative analysis of 2 groups in the sample, the group of patients that was receiving HU (and adhering to treatment) (n = 13) and the group that did not receive HU (n = 51). We assessed whether there were statistically significant differences between the groups in the parameters used to define the severity of an ACS episode: length of stay, degree of haemoglobin reduction, degree of radiographic involvement, need of transfusion and type of transfusion (simple transfusion vs exchange transfusion/erythrocytapheresis), need of intravenous analgesia or opiates, need of oxygen therapy, admission to the intensive care unit and death. The eligibility for simple transfusion and erythrocytapheresis/partial manual exchange transfusion was determined in every case by the same person (ACB, one of the authors of the study) (see Table 1).
Indications for performance of simple transfusion and partial manual exchange transfusion/erythrocytapheresis in patients with sickle cell disease admitted due to an episode of ACS.
| Indications for simple transfusion |
| Mild/moderate episode de ACS with reduction of Hb by at least 2 g/dL relative to baseline or Hb < 7 g/dL with hypoxemia |
| Indications for partial manual exchange transfusion/erythrocytapheresis |
| Severe ACS episode with multilobar involvement, pleural effusion and hypoxemia |
| Multilobar involvement that does not improve with simple transfusion |
| Multilobar involvement in patient with a previous history of recurrent severe ACS episodes |
| Rapid progression and clinical deterioration with hypoxaemia and need of high flow/invasive ventilation |
| Moderate episode of ACS (single lobe involvement) without significant reduction in Hb level and without hypoxaemia but with persistent symptoms (high fever, local hypoventilation and chest pain requiring IV morphine) after 14 days of inpatient care |
ACS, acute thoracic syndrome; Hb, haemoglobin; IV, intravenous.
We compared some baseline characteristics in the 2 groups to determine whether they were comparable (sex, age, year of admission), and found no significant differences between them.
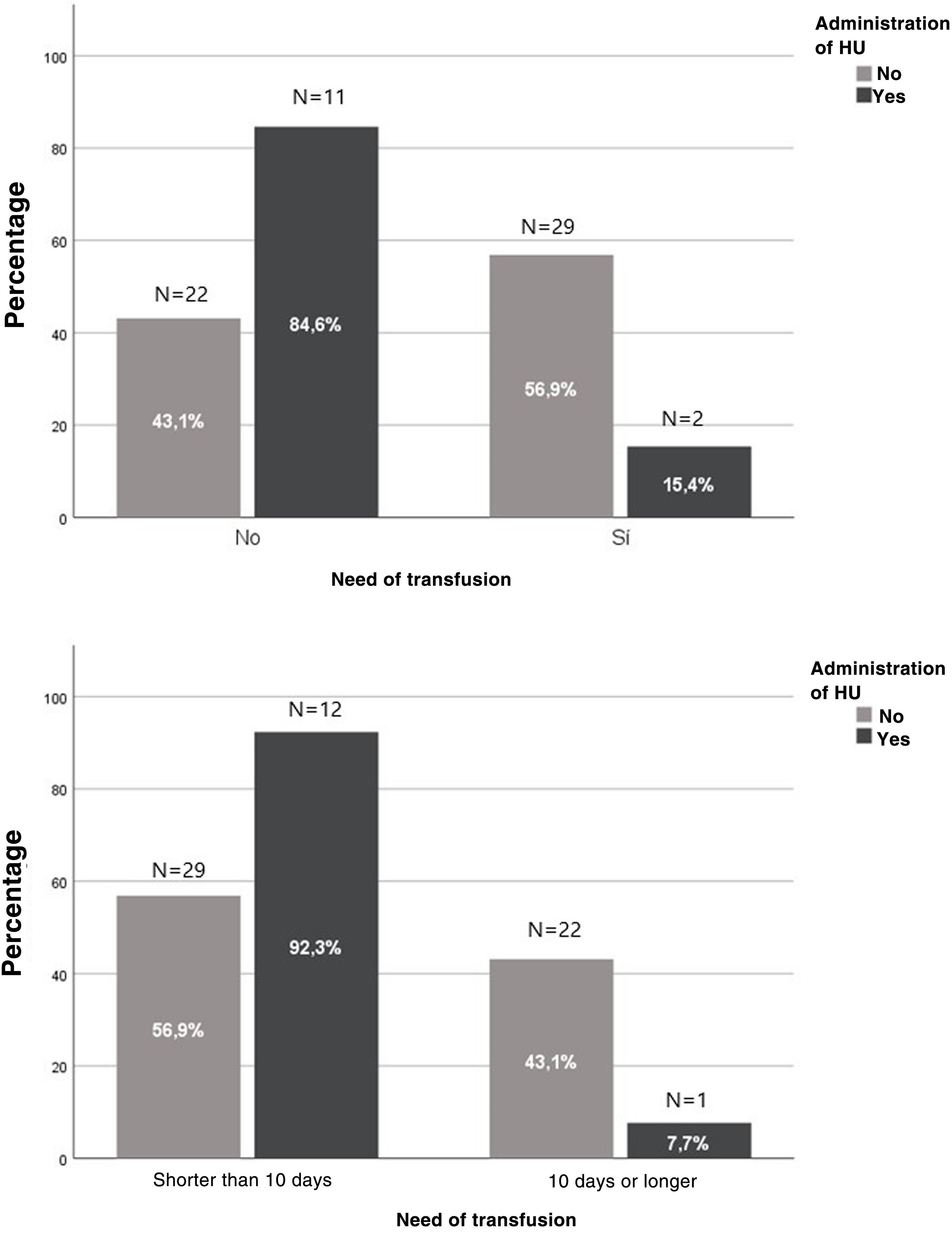
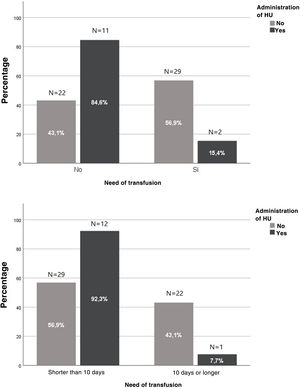
In the group treated with HU, we found a decrease in the risk of transfusion from 56.9% to 15.3% (OR, 0.138; 95% confidence interval [CI], 0.028-0.687; P = .012). In addition, only 9 patients required erythrocytapheresis/partial manual exchange transfusion, all in the group not treated with HU (P = .019). We also found a reduction in the frequency of hospitalization longer than 10 days from 43.1% to 7.7% in the treated group (OR, 0.11; 95% CI, 0.013-0.910; P = .022) (Fig. 1).
There are biases in this study due to its retrospective design and the significant difference between the numbers of treated and untreated patients, the latter group being very small. In addition, the study covered many years, so the management of the patients was probably not homogeneous, especially in the oldest cases. However, our study seems to suggest that treatment with HU can have an impact not only in reducing the frequency of episodes of ACS, but also their severity.
Please cite this article as: González-Pérez C, Gómez-Carpintero García A, Cervera Bravo Á. Influencia de la hidroxiurea en la gravedad de los episodios de síndrome torácico agudo en pacientes con drepanocitosis. An Pediatr (Barc). 2022;97:63–65.