Sjögren-Larsson syndrome (OMIM #270200) is a neurocutaneous disorder characterised by congenital ichthyosis, intellectual disability and spasticity.1 It is caused by changes in the ALDH3A2 gene, which encodes the fatty aldehyde dehydrogenase (FALDH) enzyme, involved in the oxidation of aldehydes to fatty acids.2,3
We described the different clinical and genetic characteristics of 3 cases diagnosed in our department.
Patient 1, a girl, was the first child of non-consanguineous parents with an unremarkable history. She was born at 36 weeks’ gestation, exhibiting mild erythroderma that progressed to ichthyosis vulgaris (based on the findings of the skin biopsy) (Fig. 1).
She was referred to the paediatric neurology department at age 17 months due to severe axial hypotonia with instability in sitting and ichthyosis. The findings of the metabolic, neurophysiological and neuroimaging tests at the time were normal.
Although the patient did not present with additional signs of syndromic ichthyosis,4 comparative genomic hybridization testing was performed, which detected a 159.6 kb deletion in region 17p11.2, hg19 (chr17:19424245-19583843) that contained the ALDH3A2 gene. Sequencing of the other ALDH3A2 allele revealed a frameshift variant in exon 1 (c.86_96del, p.Ala29Aspfs*21) that gave rise to a truncated protein.
The segregation analysis of the family revealed that both changes were inherited (one from each parent).
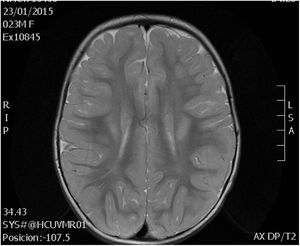
A magnetic resonance imaging (MRI) scan performed at age 2 years found myelination defects (Fig. 2). Currently, at age 6 years, the patient has mild intellectual disability and axial hypotonia with spasticity in the lower extremities that precludes independent walking.
The patient has experienced 5 episodes of typical febrile seizures that did not require antiepileptic medication. She has not developed vision abnormalities to date.
Patients 2 and 3 are sisters in a family with no known consanguinity. At birth, at 34 and 36 weeks’ gestation, respectively, both presented with moderate ichthyosis described as “lamellar”. They developed the ability to sit at around 9 months and independent walking between ages 4 and 6 years. Patient 2 retains independent walking at age 22 years. Both sisters developed signs of spasticity in the first 2 years of life, and Sjögren-Larsson syndrome was suspected due to the detection of myelination defects on neuroimaging.
Both patients developed typical febrile seizures, language delay and mild intellectual disability.
At ages 14 and 16 years, respectively, inclusions were detected in the ocular fundus.
The diagnosis was based on enzyme activity assays in fibroblasts and sequencing of the ALDH3A2 gene. Both patients were homozygous for the previously described variant c.471+1delG (NM_000382.2).
The family segregation analysis confirmed that both parents were carriers of the variant.
As of June 2020, there were 280 reported variants of the ALDH3A2 gene in 182 individuals with Sjögren-Larsson syndrome (Leiden Open Variation Database [LOVD], PubMed). Some, like c.471+1delG, detected in patients 2 and 3, have been described in many European families. However, the variants detected in patient 1 were novel.5
A previous review of cases reported in Spain identified 4 cases diagnosed in adulthood after detection of the characteristic ocular or cutaneous lesions, and only 1 diagnosed in childhood.6
The c.86_96del variant produces a shift in the reading frame and results in a truncated protein. However, the presence of another start codon downstream suggests the possibility of a protein missing the first 32 amino acids (of the 508 of the full protein) that could maintain some residual activity and result in an attenuated phenotype.
We believe that it is important to be aware of the association of congenital ichthyosis with neurologic impairment as one of the known neuroichthyotic syndromes and of the presence of carriers of these variants in Spain to facilitate early diagnosis and the establishment of an accurate phenotype/genotype correlation. Patient 1, who had a deletion and a variant that had not been previously described presented with more severe axial hypotonia and milder ichthyosis compared to patients 2 and 3, who had a previously described variant.
Please cite this article as: Villar-Vera C, Cuesta Peredo A, Monfort-Belenguer L, Abellán Sanchez MR, Martínez-Costa C. Síndrome de Sjögren-Larsson en España; descripción de 3 nuevos casos. An Pediatr (Barc). 2021;95:203–204.