Inadequate information management, especially during patient handoff, contributes to a large part of health care-related adverse events. The Committee for Quality of Care and Patient Safety of the Asociación Española de Pediatría has developed this document to provide an overview of handover practices in different paediatric care settings (emergency, inpatient, intensive care, neonatal and primary care). It describes resources to achieve safe and effective communication in all these settings, such as standardised handoff tools. It also proposes recommendations for the prevention of medication errors during the handover process, to improve safety in interhospital and intrahospital patient transfer, and to optimise communication and continuity of care in chronically ill and medically complex children.
El manejo deficiente de información, en especial durante la transferencia o el traspaso de cuidados, contribuye a gran parte de los eventos adversos relacionados con la asistencia sanitaria. El Comité de Calidad Asistencial y Seguridad en el Paciente de la Asociación Española de Pediatría ha confeccionado este documento para ofrecer una aproximación a los procesos de transferencia en distintos ámbitos asistenciales pediátricos: urgencias-emergencias, hospitalización, cuidados intensivos, neonatología y atención primaria. Se describen recursos para lograr una comunicación segura y efectiva en todos estos ámbitos, empleando, entre otros métodos, herramientas estandarizadas de transferencia. Se proponen también recomendaciones para la prevención de errores de medicación durante los procesos de transferencia, la mejora de seguridad durante los traslados y derivaciones entre ámbitos, y también para un mejor traspaso de información asistencial en los niños y adolescentes con enfermedades crónicas y complejidad asistencial.
Errors and omissions in the management of information during care delivery pose a threat to the safety of the patient1 and have been found to cause more than 70% of adverse events in health care settings.2
The necessary skills to achieve safe communication in health care are not taught, honed or practiced within the official curriculums of medical and allied health degrees, speciality training programmes or continuing education programmes.3 In contrast, in the civil aviation sector, mandatory and standardised practice guidelines for communications in air traffic have been developed4 in the framework of a global air safety improvement culture, with excellent results.5
There are particularities in the field of paediatrics that contribute to information errors. One is the age of the patients themselves, which frequently precludes them from participating in the management of information about their own health problem. Other factors are that paediatric patients have several caregivers, who may not be coordinated, the growing medical complexity of many paediatric patients and substantial or situations in which the health care system is heavily burdened, increasing the volume of information that is exchanged among professionals in different care settings.
In developing this document, Committee on Health Care Quality and Patient Safety of the Asociación Española de Pediatría (AEP, Spanish Association of Paediatrics) sought to offer paediatricians an approximation to the specific issues in their care settings and tools to achieve effective and safe communication in health care.
Patient handoff. Concept and real-world practice scenariosThe term handoff, or handover, refers to the transfer of patient care responsibility between health care professionals through the effective communication of all the necessary health-related information, current diagnoses, needs and treatment goals. Its purpose is to ensure the continuity of care and guarantee patient safety during transitions of care among all involved parties.
Patient handoffs are considered critical junctures at which errors are more likely take place in the communication of information. They encompass a large number of everyday activities, but the following are particularly important for patient safety:
- •
Referrals between different care settings.
- •
Shift changes.
- •
Intrahospital and interhospital transfers.
- •
Requests for assessments or changes in care.
- •
Discharge home or to a hospital-at-home unit.
- •
Unexpected changes in the condition of the patient that require involvement by other providers.
During handoffs, information may be communicated in different forms or a combination thereof: orally (in person, by telephone, by videoconference) or in writing. In the case of oral handoffs, information should be exchanged face-to-face by the professionals directly involved in care delivery. In some cases, in a practice that is discouraged, the handoff is delegated through the participation of an intermediary that later conveys the information to another professional who was absent at the time of the handoff, so that the necessary interaction between the professionals in charge of the patient does not take place.
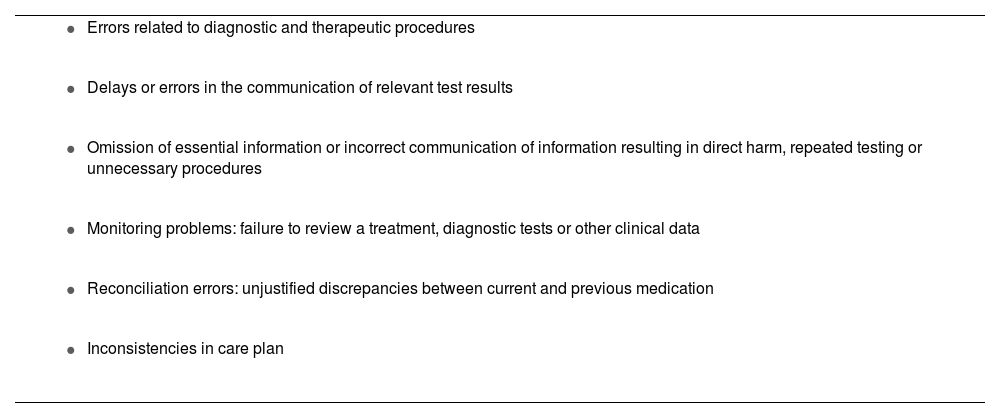
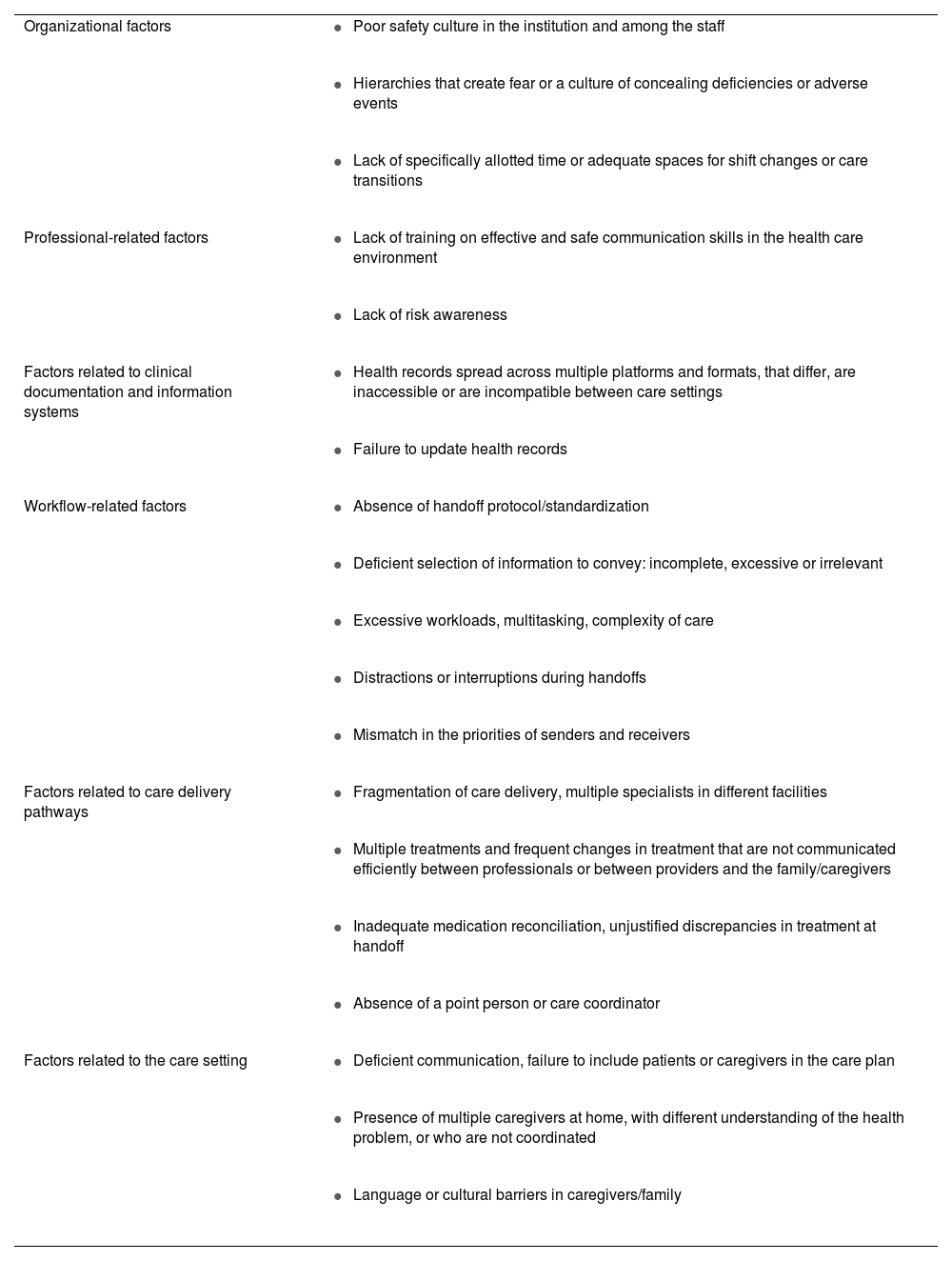
Adverse event reporting and real-world clinical practice data evince that the transfer of information can be inadequate and that it can be improved, as it leads to errors of different nature (Table 1). There are various factors that cause or contribute to poor communication and safety risks at the level of the organization, care delivery pathways and workflows and the health care staff (Table 2).
Safety incidents or risk situations associated with a deficient exchange of information between different professionals or between professionals and patients or caregivers.
|
|
|
|
|
|
Factors that increase the risk of errors in information management and deficient communication in health care settings.
| Organizational factors |
|
| |
| |
| Professional-related factors |
|
| |
| Factors related to clinical documentation and information systems |
|
| |
| Workflow-related factors |
|
| |
| |
| |
| |
| Factors related to care delivery pathways |
|
| |
| |
| |
| Factors related to the care setting |
|
| |
|
Different measures that can be applied to all care settings have been proposed to address the safety problems involved in patient handoff:
- 1
Improving the communication skills of health care professionals. Medical organizations and scientific societies have proposed making these skills a required component of educational curricula, including the use of simulation.
- 2
Promoting the participation of patients, family members and other caregivers through effective two-way communication with health care providers. Practices such as bedside handoff during shift changes in inpatient and emergency care settings provide relevant visual information to professionals, allow clarification of doubts in situ and offer patients and caregivers the opportunity to participate in care delivery. They also promote a humanised and patient-centred care approach.
- 3
Facilitating the reporting of adverse events and incidents related to errors in the communication of information.
- 4
Implementing the use of specific tools for patient handoff for the professionals involved in care transitions.
These tools are standardised handoff models that use checklists to facilitate a structured and homogeneous management of essential information, thereby preventing the omission of critical data. The goal is to create a shared mental model so that information is transferred with an objective, comprehensive and organised structure.
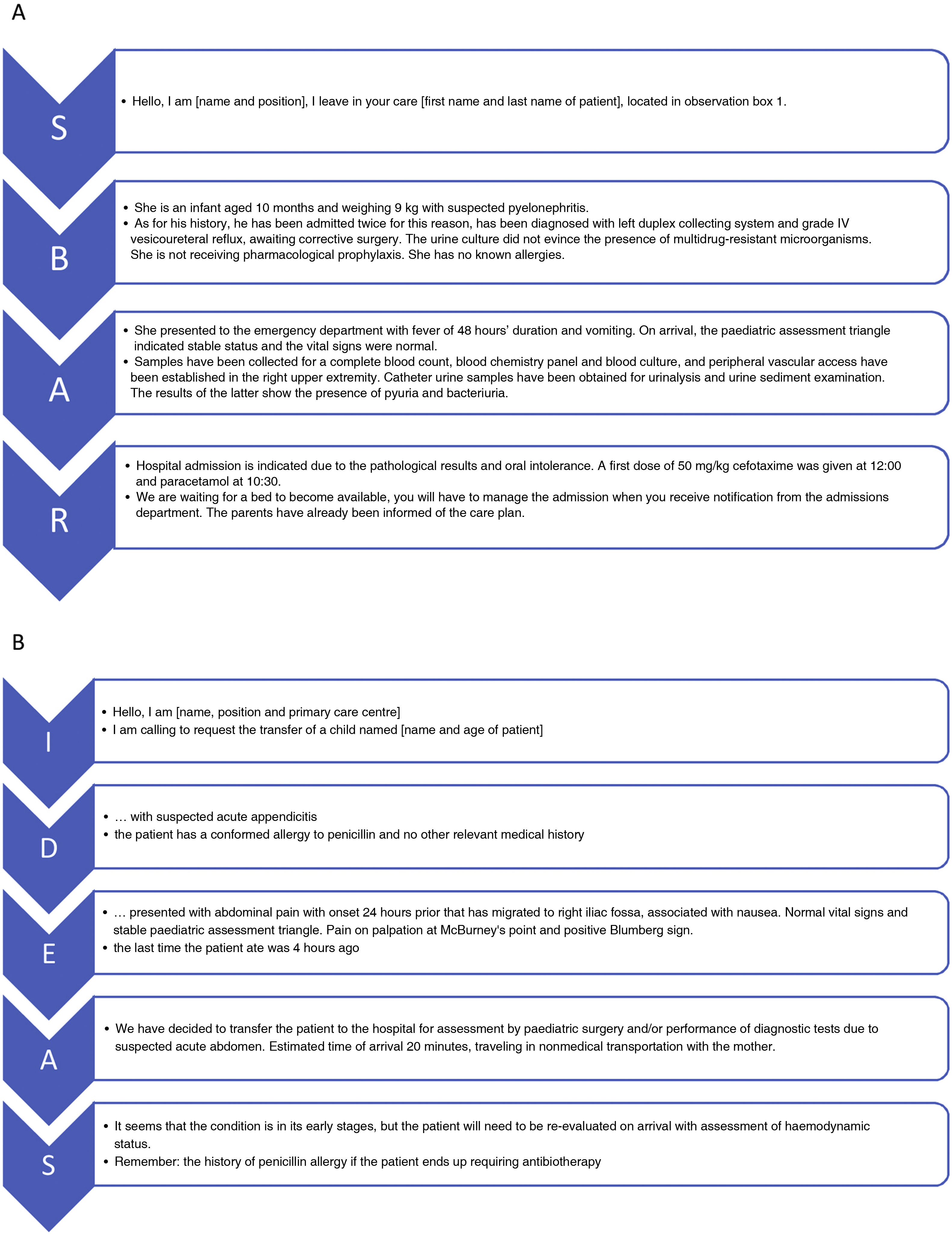
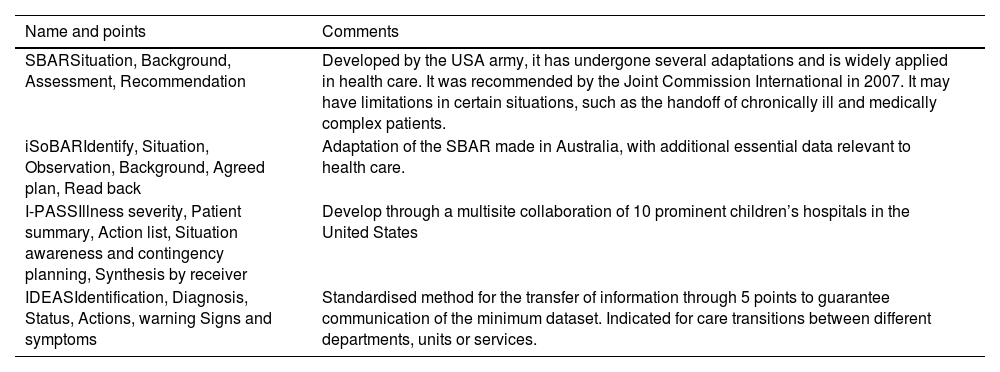
There is a growing number of these standardised models that have been validated and proven extremely useful6–9 (Table 3). Most of these tools use acronyms formed with the initial letters of the critical contents that must be included in the information sequence that serve as mnemonic devices. Fig. 1 presents two clinical scenarios that illustrate the structure of the contents covered in each of the items of the two most widely used handoff methods in our region, SBAR and IDEAS. Depending on the care setting, these tools may require adaptations as to the quantity and complexity of the relevant information, and the number of professionals involved in the handoff process.
Widely used patient handoff tools.
| Name and points | Comments |
|---|---|
| SBARSituation, Background, Assessment, Recommendation | Developed by the USA army, it has undergone several adaptations and is widely applied in health care. It was recommended by the Joint Commission International in 2007. It may have limitations in certain situations, such as the handoff of chronically ill and medically complex patients. |
| iSoBARIdentify, Situation, Observation, Background, Agreed plan, Read back | Adaptation of the SBAR made in Australia, with additional essential data relevant to health care. |
| I-PASSIllness severity, Patient summary, Action list, Situation awareness and contingency planning, Synthesis by receiver | Develop through a multisite collaboration of 10 prominent children’s hospitals in the United States |
| IDEASIdentification, Diagnosis, Status, Actions, warning Signs and symptoms | Standardised method for the transfer of information through 5 points to guarantee communication of the minimum dataset. Indicated for care transitions between different departments, units or services. |
Example of the use of handoff tools in 2 hypothetical clinical scenarios: A) SBAR method applied to the handoff of a patient under observation in the emergency department during a shift change and B) IDEAS method in the telephonic referral of a patient from the primary care centre to the emergency department of a hospitals. IDEAS: Identification, Diagnosis, Status (E for Estado, in Spanish), Actions, warning Signs/Symptoms. SBAR: Situation, Background, Assessment, Recommendation.
These systems use different formats (oral, print, digital…). The information conveyed during any handoff, including oral information, must be documented in the patient’s health record, the indispensable record of clinical activity.
The use of these tools, combined with other interventions, has improved the safety of handoffs, with a 23% reduction in medical errors and a 30% reduction in preventable adverse events.10 The standardisation of patient handover processes with the introduction of these tools is associated with an increased in the perceived satisfaction and sense of control of professionals and greater patient safety, in addition to reducing the time required to exchange information during shift changes.11
The mere dissemination of handoff tools does not guarantee an improvement in the communication between professionals and health care users during handoffs. Their introduction must be accompanied by organizational changes in workflows and the training of professionals through performance-based educational activities (such as practical workshops and in situ simulation exercises).
Patient handoff and information management in specific care settingsPaediatric emergency careIn this setting, the transfer of information takes place in a fast-paced context with a high risk of safety incidents related to the management of information. Some of the contributing factors are unstructured communication, high patient volume, difficulty accessing information, pending results or consultations, multiple changes in treatment and in the providers in charge or difficulty referring patients to other departments or units in the hospital.12
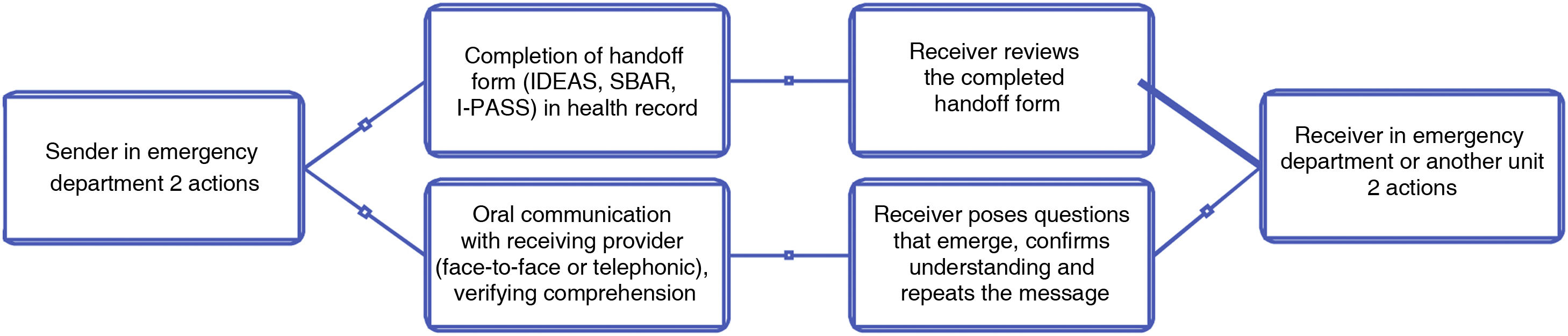
Interventions aimed at improving communication must comprehend all phases of urgent and emergency care: prehospital care, transport, arrival to the emergency department, shift changes, consultations with specialists, admission, referral to other specialised facilities or discharge home. Specific strategies to standardise each of these care transitions must be developed based on the participants, location (centralized or at bedside), method of information exchange, use of adjuncts (standardised tool or inhouse checklist) and the relevant information that must be conveyed.13 In the emergency setting, in addition to the use of handoff checklists, the use of a structured two-way back-and-forth approach to information sharing, known as “closed loop” communication, is recommended14 (Fig. 2).
Paediatric inpatient careAny hospitalization entails the communication of a substantial volume of information, often shifting, between multiple professionals involved in the care of other patients and over successive shifts. To guarantee patient safety and care quality in this environment, care transition practices need to be protocolized and integrated in the routine workflows of the different hospital settings.15 At times, standardised handoff tools need to be adapted to specific settings,16 with formats and contents suited the specific needs of the different specialities, the level of medical complexity and the expertise of the participants.
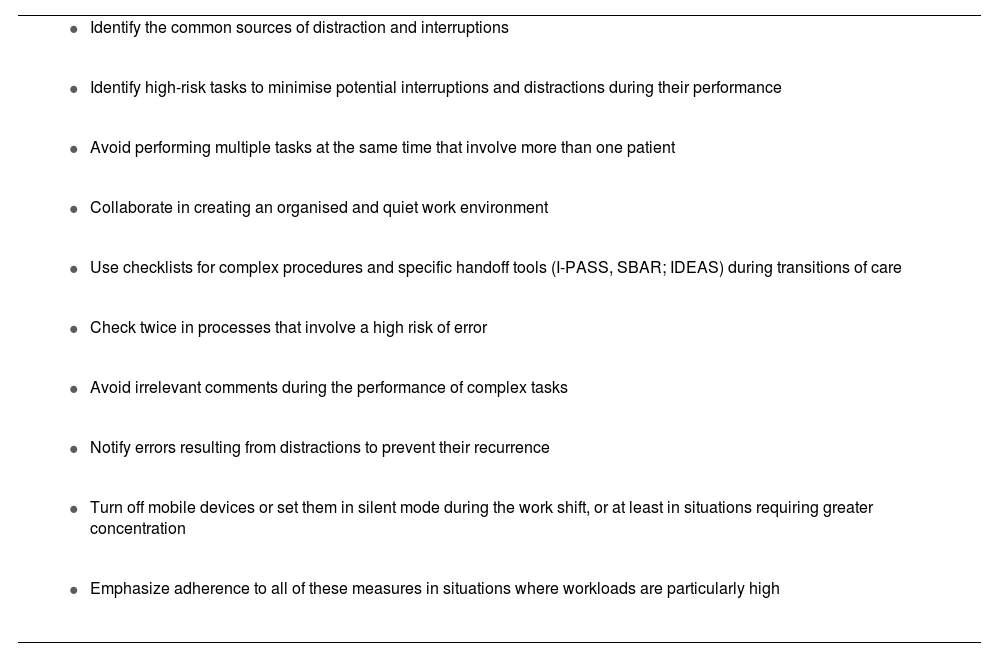
Emphasis has also been placed on the need to promote conditions in hospital settings that facilitate the transfer of information, free from distractions or interruptions17 (Table 4).
Recommendations for the prevention of distractions and interruptions in hospital settings.
|
|
|
|
|
|
|
|
|
|
Adapted from the 10 Principles of the Sociedad Española de Pediatría Interna Hospitalaria (SEPIH, Spanish Society of Paediatric Internal Medicine).17.
The medical complexity of patients managed in these units increases the risk of deficiencies in the relay of information. For this reason, the use of standardised handoff systems is recommended, such as the SBAR (Table 3), the one that has been studied most extensively in the intensive care setting.18
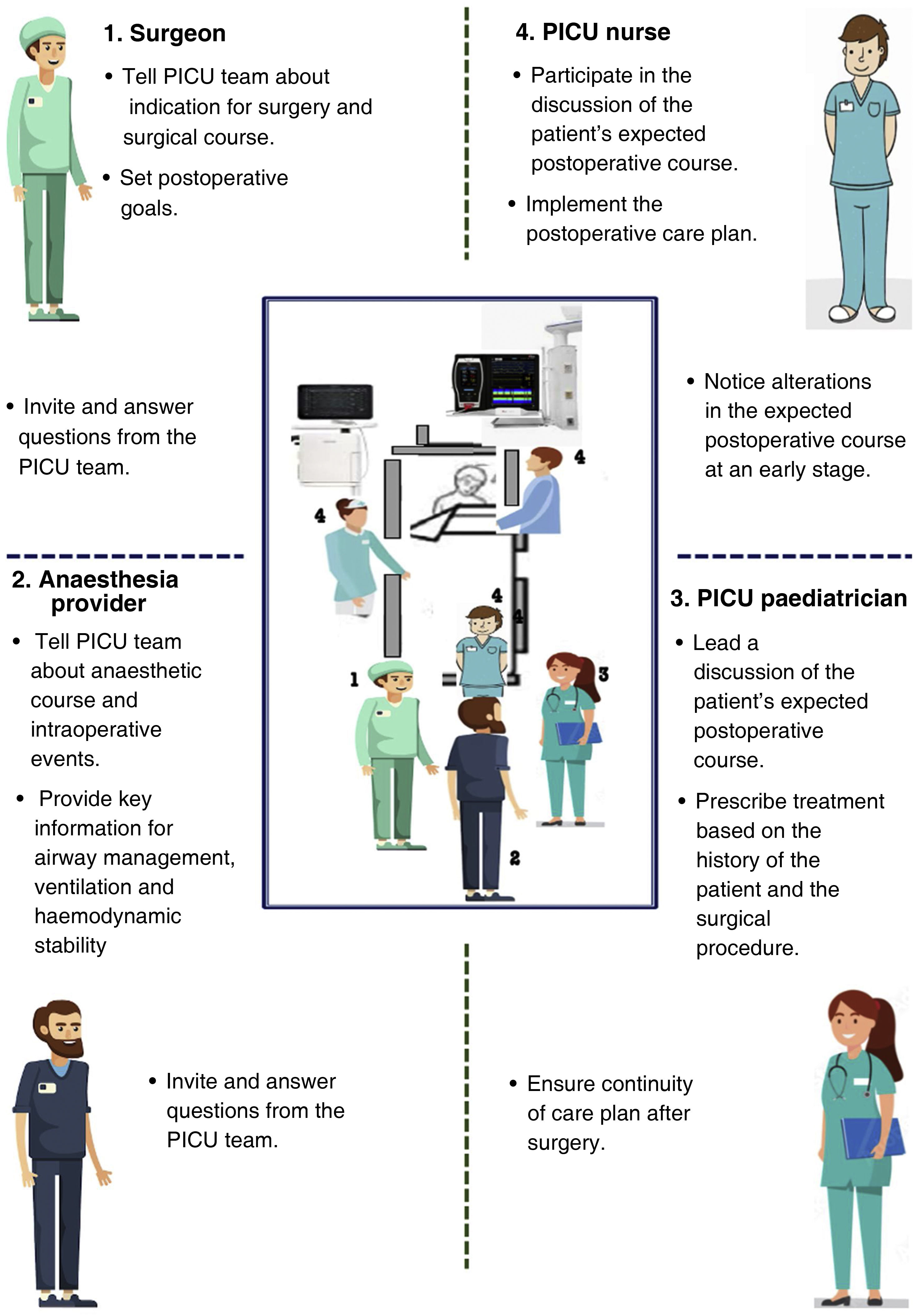
Each unit should adapt handoff protocols to their particular circumstances and to the objectives of the handoff, depending on whether the care transition is due to a shift change, the transfer to another unit, patient discharge or a procedure.19,20 In highly complex postoperative handoffs,21 the multidisciplinary care team must be agile and coordinated and have an accurate exchange of relevant information supported by the use of a checklist to prevent the omission of critical data22 (Fig. 3).
Neonatal careCommunication between professionals and handoff processes amount to a substantial proportion of neonatal care delivery.23 In addition, this field requires the integration of maternal and neonatal information and the involvement of other essential professionals (obstetricians, midwives),24 which increases the complexity of exchanging information and the risk of errors. This is also the case of neonatal care delivery in the maternity ward and in the referrals of neonates to primary care or outpatient speciality clinics for follow-up. As is the case in other fields, the risk of errors during handoff increases with increasing medical complexity in and patients who require multidisciplinary care, such as neonatal surgical patients.
Some of the proposed strategies to improve handoffs in this field include the integration of labour and delivery and neonatal health record systems, shared referral protocols, standardised discharge summaries, PDCA (plan, do, check and act) cycles supported by clinical simulation or the use of specific standardised handoff tools.25
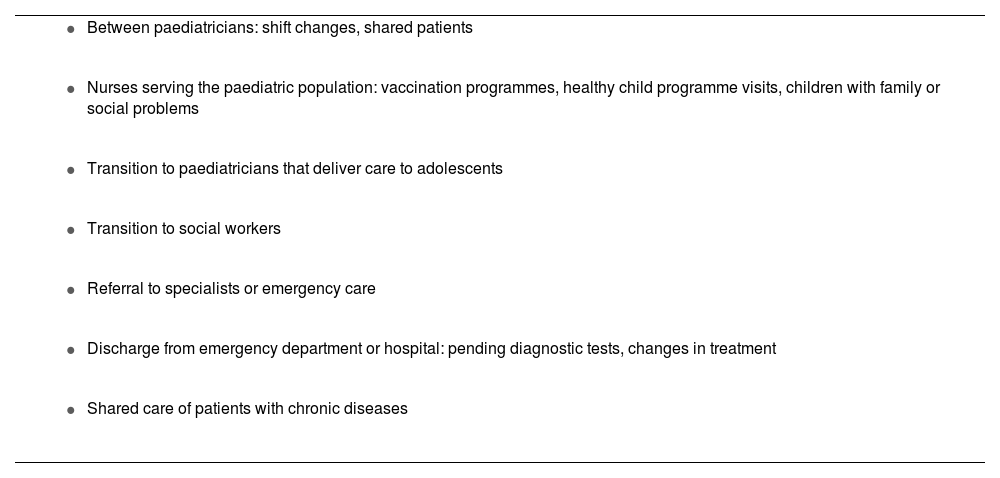
Primary careAlthough interventions that entail transitions of care are commonplace in primary care practice (Table 5), few studies have assessed these processes at this level of care.26
Most common situations involving patient handoffs at the primary care level.
|
|
|
|
|
|
|
The circumstances under which primary care is delivered increase the risk of errors in the management of clinical information and warrant the implementation of specific improvement strategies. The high workloads and patient volume of primary care clinics require an emphasis on pending tasks and medication changes, both in handoffs within the primary care level and in transitions to other care settings.
Measures for the effective and safe transfer of all relevant information must also be taken in the scheduled handoff of adolescent patients from paediatric care to family and community medicine physicians.27 In the case of patients with chronic illness,28 a “warm hand off” between the paediatric and adult care teams is recommended, with participation of the patient and the caregivers.29 This care transition does not match the usual scale of information transfer. It is not a punctual action, but rather requires adequate anticipation and planning by a multidisciplinary team specifically trained and qualified to deliver adolescent care. Families and patients, especially those with special health care needs, require guidance to adapt to the adult care system, and patient safety and care continuity must be ensured during the entire transition process.
Care transitions between settings, intrahospital and interhospital transfersTransitions of care involve the handoff of patients between different care settings and providers, with priorities and work patterns differing between the sending and receiving care teams.30 These transitions are considered vulnerable moments that require meticulous handling of clinical information.
The communication of information is one of the most relevant steps in neonatal and paediatric transport, given the severity of illness in most of these patients. Care teams must devote the necessary effort to verify and summarise the relevant clinical information, which is of vital importance in critically ill or medically complex patients. Although the traditional method, the referral form filed in the health record, is still used and valuable, it must be supplemented with the use of standardised handoff tools, oral and written, providing the opportunity to pose questions and to ensure adequate comprehension of the information.31
Medication and prevention of medication errorsPatient handoffs are a significant source of medication errors (MEs), most frequently caused by failures in the communication between health care professionals or between professionals and patients or their caregivers.32,33 The greater vulnerability and probability of errors in paediatric patients call for the implementation of prevention strategies in any transition of care.
During handoffs, prescriptions must be communicated in adherence to good clinical practice guidelines,34–36 with express statement of any changes, guaranteeing correct medication reconciliation and thus avoiding unexplained discrepancies. Some of the recommendations are:
- 1
For each drug, state: active ingredient, dose, frequency, route of administration and duration, in addition to information on the last administered dose.
- 2
Convey the dose in mass units or international units, rather than volume units or dosage forms (eg, number of capsules).
- 3
For oral liquid medication to be administered by the caregivers, express the dose in volume units as well, in ml or mL (never in “cc”).
- 4
Include the weight of the child and, in patients with renal failure, the glomerular filtration rate.
- 5
Verify that the information includes any drug allergies.
- 6
Review whether the patient is taking any other products with pharmacological activity (homeopathy, phytotherapy…) and assess the potential interactions.
- 7
Document any changes made.
- 8
Carry out the medication reconciliation process. This entails obtaining a full list of previous medications, comparing it with current prescriptions and analysing and resolving any unjustified discrepancies.
- 9
If the patient requires at-home care, caregivers will be provided the necessary information and guidance, both orally and in written form (updated medication form), verifying that caregivers understood the provided information.
Children with chronic diseases, especially those that are medically complex, experience more adverse events due to deficient handling of medical information.37 This risk increases during care transitions between settings or to the caregivers at home, where the care of the patient frequently involves medication.
Among the specific improvement strategies that have been proposed is the individualized care plan, with a standardised structure and up-to-date essential information, made accessible to all professionals involved in care delivery, either urgent or scheduled.38
The patient care plan must be revised and updated on an ongoing basis in response to clinical or setting changes to ensure it accurately reflects current specific goals. In inpatient care, updated summaries should be made at close enough intervals to reflect the main unresolved issues, optimise the coordination of providers, define actions to be undertaken in the case of intercurrent disease or exacerbations and ensure the appropriate fit of diagnostic and therapeutic measures.39
Comprehensive care delivery in these patients benefits from the appointment of roles as the coordinating paediatrician or nurse care manager, who centralize the organization of care and optimise communication between all involved parties.
Key moments (medication reconciliation, hospital admission/discharge, transitions from paediatric to adult care…) require the participation of parents or other active caregivers and, whenever possible, the patient as well.40 This improves communication overall, and therefore the safety of patient handoffs.
ConclusionHandoffs encompass a large number of actions of crucial importance to patient safety. Communication in this context must be clear, unequivocal, fluid and in compliance with good practice guidelines, like other aspects of diagnosis or treatment.
All parties involved (institutions, professionals and families) must be aware of the important risks associated with a deficient exchange of information during transitions of care.
Training aimed at improving communication skills achieves noticeable improvements in health care quality and patient safety and should be included in the education of all paediatric providers. Standardised handoff systems are a very useful resource in care transitions and, consequently, should be integrated in everyday clinical practice.
These improvement measures must be accompanied by changes in the organization and dynamics of care delivery, and adapted to each care setting and the needs of patients and their families.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank Aurora Madrid Rodríguez and Dr Carles Luaces Cubells for all the support they provided in the development of this article.