About 0.2–6.1% of newborns in the developed world have been conceived by assisted reproductive techniques (ART). Higher rate of major and minor malformations have been described in this population, but the multiple possible confounders associated make it difficult to establish a direct causal relationship and the specific factors involved.
Material and methodsTo determine the risk of these malformations in our population, a collaborative prospective controlled cohort study was designed. We collected the specific ART-data related to the clinical gestation of women treated in a period of 2 years in the Reproduction Unit from a Spanish public tertiary-level hospital. 231 out of 267 newborns of these gestation (88%) participated in the study and were assessed by a pediatrician with expertise in Clinical Genetics and Dysmorphology at 12–20 and 26–40 months of age. At the same time a controlled group of children naturally conceived (NC) was selected according to the following criteria: the next NC newborn belonging to the same group of maternal and gestational age, and type of gestation (single or multiple). 230 controls were chosen and 208 participated in the study (90%).
ResultsMajor malformations were presented in 7.8% of the ART-children and 7.2% of the controls, without founding statistically differences between groups. However, differences were found in the risk of some minor malformations such as capillary malformations and pigmentary lesions, higher in the ART-group. A recurrent pattern of craneofacial anomalies was also unexpectedly detected.
ConclusionsIn spite of the high rate of major congenital malformations detected, there were no differences between groups. Thus, our results suggest that ART may affect the normal embryonic development but in a milder way than other confounding factors do. The facial phenotype identified has not previously been described, either the higher risk of capillary malformations and pigmentary lesions. More studies are needed to confirm this association.
En torno al 0,2–6,1% de los recién nacidos en los países desarrollados han sido concebidos por técnicas de reproducción asistida (TRA). Se han descrito tasas más altas de malformaciones congénitas (MC) mayores y menores en esta población, pero los múltiples posibles factores de confusión asociados hacen difícil establecer una relación de causalidad directa con estos procedimientos y conocer los factores específicos implicados.
Material y métodoSe realizó un estudio prospectivo de cohorte controlado con el objetivo de determinar el riesgo de MC en niños-TRA. Se recogieron los datos específicos de la TRA de una cohorte de gestaciones clínicas de mujeres tratadas en la Unidad de Reproducción de un hospital público de tercer nivel durante dos años; 231 de 267 (87%) niños nacidos de dichas gestaciones-TRA participaron en el estudio y fueron valorados por un pediatra con formación en Genética Clínica y Dismorfología a los 12–20 y a los 26–40 meses de edad. De forma simultánea se seleccionó una cohorte de niños concebidos de forma natural (CN), de acuerdo con los criterios: siguiente recién nacido al caso del mismo grupo de edad materna, edad gestacional y tipo de gestación (única o múltiple); 230 niños CN fueron seleccionados y 208 (90%) participaron en el estudio.
ResultadosSe detectaron MC mayores en el 7,8% de casos y en el 7,2% de controles, sin existir diferencias estadísticamente significativas entre ellos. Sí se identificaron diferencias en algunas malformaciones menores como las malformaciones capilares y lesiones pigmentarias, más frecuentes en el grupo TRA. Además, se identificó de forma inesperada un patrón craneofacial recurrente en el grupo TRA.
ConclusionesA pesar de las altas tasas de MC mayores, no se detectaron diferencias significativas entre grupos, pero sí entre algunas anomalías menores, lo que sugiere que las TRA tienen un impacto leve sobre el desarrollo embrionario. El fenotipo facial identificado no ha sido descrito previamente, así como el mayor riesgo de lesiones pigmentarias y malformaciones capilares. Son necesarios más estudios que corroboren estas asociaciones.
Assisted reproductive technology (ART) has been used for more than 40 years. Since its introduction, it is estimated that 0.2%–6.1% of children in European countries have been conceived with the help of these techniques.1 The potential association between the use of ART and the development of congenital malformations (CMs) has been the object of extensive study. The prevalence of CMs is estimated at 2%–3% in the general population and has remained stable in recent years (https://eu-rd-platform.jrc.ec.europa.eu/eurocat_en2). Although most authors report higher proportions of CM in individuals born after ART,3–7 the evidence is still inconclusive, as there are also studies in which these differences disappear after adjusting outcomes for factors such as maternal age or ART-related variables.8,9 Still, the most recently published systematic review and meta-analysis10 did find an increased risk of CM in singleton births after ART (relative risk [RR], 1.41; 95% confidence interval [CI], 1.30–1.52), although this increased risk was not found in individuals fruit of multiple gestations (RR, 1.18; 95% CI, 0.98–1.42).
There are fewer studies on the subject of minor anomalies. Still, the use of ART has been described as a risk factor for infantile haemangioma,11 and great proportions of children of subfertile couples that used ART have been found to have minor anomalies considered clinically insignificant based on the classification of Merks et al.12 Between 50% and 54% presented this type of anomalies,13 most frequently infantile haemangioma (2%–5%), inguinal or umbilical hernia (1%–3%), hypospadias (1%–2%) or cryptorchidism (1%–2%).
Many authors have also attempted to determine whether outcomes differ between in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) and other ART-specific factors, but results have been inconclusive. Some authors have reported a higher incidence of CMs in association with ICSI14–16 and others a higher risk associated with IVF,17 while more recent studies have found no differences.18,19 There is also no clear evidence that the risk of CMs increases with frozen embryo transfer (FET),20 and further research is still needed.
In light of the above, the primary objective of our study was to assess whether there was an increased risk of major and minor CMs in a cohort of Spanish children aged up to 3 years born after ART, independently of maternal age, singleton/multiple order pregnancy, preterm birth and other possible confounders.
We also analysed ART-related factors that could be at play in the detected malformations.
Material and methodsWe designed a prospective, observational, controlled cohort study. The study was approved by the Ethics Committee of the Hospital Clínico Universitario Virgen de la Arrixaca (HCUVA). Participation in the study required signed informed consent, which was procured in adherence with the principles of the Declaration of Helsinki.
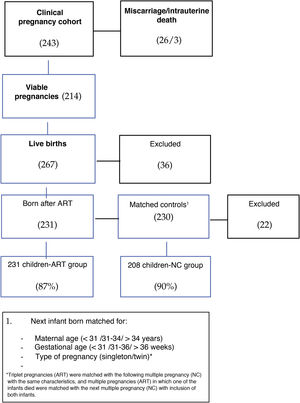
Selection of cohort of clinical pregnancies achieved through ARTFirst, we selected a cohort of clinical pregnancies (evidence of a heartbeat on week 7–8 of gestation) in women that underwent IVF, ICSI or preimplantation genetic diagnosis (PGD) between May 2012 and May 2014 in the fertility unit of the HCUVA, a public tertiary care hospital that has partnership agreements with 5 private clinics. In the period under study, there were 243 clinical pregnancies, 26 miscarriages and 3 cases of intrauterine foetal demise. Fig. 1 presents the cohort selection process.
In this phase, we collected the following data:
- -
Epidemiological characteristics: country of origin, age at initiation of treatment and personal and family history of the parents, maternal body mass index, duration and causes of infertility.
- -
Treatment-related variables: type of ART, type of ovarian stimulation and suppression used, complications, number of retrieved eggs and fertilized eggs, embryo quality, day of embryo transfer, cryopreservation, etc.
In the second phase, we reached out to couples that had viable pregnancies (214) by telephone to invite them to participate. We informed them of the objectives of the study and that it would require 2 health evaluations in their children before age 3 years. For those who agreed to participate, we scheduled appointments for an assessment with a paediatrician with specialised training on clinical genetics and dysmorphology.
Selection of matched controlsConcurrently, we assessed a control group that was selected applying the following criteria:
Naturally conceived infant (NC) born after a case that belonged to the same categories for the following variables:
- -
Maternal age (≤30; 31–34; 35–39 years).
- -
Gestational age: ≤30, 31–36, ≥37 weeks.
- -
Type of gestation (singleton or multiple).
In the control group (230 controls), we excluded families that agreed to participate in the initial contact by telephone but subsequently:
- -
Missed the scheduled visit twice.
- -
After being selected as controls turned out to have used some form of ART (artificial insemination, IVF, etc.).
- -
Chose to drop out of the study.
In this phase, we carried out the clinical evaluations: one at age 12–20 months and the other at age 26–40 months, all between September 2014 and June 2017.
In these evaluations, we collected data on the pregnancy, delivery and neonatal period (Fig. 2) and carried out a comprehensive physical examination, including a thorough morphological assessment. We classified major anomalies according to the International Classification of Diseases, 10th revision (ICD-10, https://www.mscbs.gob.es/estadEstudios/estadisticas/normalizacion/CIE10/Clasif_Inter_Enfer_CIE_10_rev_3_ed.diag.pdf21) and minor anomalies based on the classification proposed by Merks et al.12
Statistical analysisTo pursue the objectives of the study, we analysed the data in 2 phases:
In the first phase, we assessed differences in major and minor CMs at age 26–40 months in children born after ART (cases) and NC children (controls) and other general characteristics that could interfere with the interpretation of the results (perinatal disease, exposure to toxic substances, etc.). In the second phase, we analysed the case cohort and ART-related data to identify factors potentially involved in the development of CMs.
The variables that we analysed as potential ART-related risk factors were: less than 4% of sperm with normal morphology (Kruger criteria), causes of sterility, baseline levels of follicle-stimulating hormone (FSH) and estradiol, preconception folic acid supplementation, type ART (IVF, ICSI, FET or PGD), day of embryo transfer, number of transferred embryo, ovarian stimulation and suppression protocol, history of ovarian hyperstimulation syndrome (estradiol >3000 pg/mL and compatible sonographic features), mean number of retrieved eggs, fertilised eggs and viable embryos, embryo quality based on the ASEBIR classification.
To analyse the association between qualitative variables, we used the χ2 test and the Fisher exact test for 2 × 2 contingency tables. To compare quantitative variables in 2 groups, we used the Student t test or Mann–Whitney U test based on whether or not the data followed a normal distribution. To compare more than 2 groups, we used analysis of variance (ANOVA) if the data were normally distributed, and otherwise the Kruskal–Wallis test.
We also performed a multivariate analysis, using multiple logistic regression if the dependent variable was dichotomous, multinomial regression if the dependent variable was polytomous and multiple linear regression if the dependent variable was quantitative and normally distributed. We used transformation methods to achieve a normal distribution when necessary. The covariates included in the multivariate analysis were those that exhibited a significant association in the preceding univariate analysis.
We defined statistical significance in hypothesis testing as a p-value of less than 0.05. The statistical analysis was performed with the software StataCorp (2017) Stata Statistical Software Release 15 (StataCorp LLC, College Station, TX, USA).
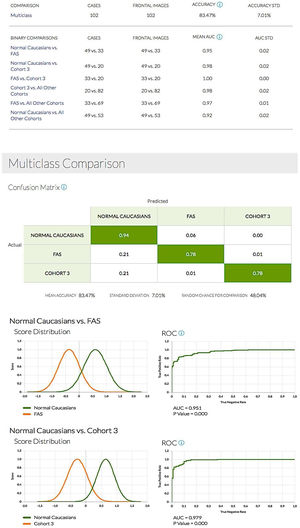
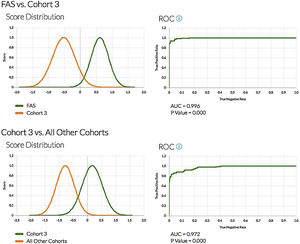
Lastly, due to the chance finding of a recurrent craniofacial pattern in the ART cohort during the evaluations, we used the facial recognition software developed by the Face2gene team (http://suite.face2gene.com22) and, in collaboration with them, analysed 3 groups of patients: 50 Caucasian controls matched for age, 34 children with foetal alcohol syndrome and 20 children born after ART. The goal was to see whether the software, which converts a photograph of the patient into mathematical facial descriptors to build a face grid,23 could differentiate the 3 phenotypes.
ResultsGeneral characteristics of the cohorts under studyTable 1 shows that the 2 cohorts under study were comparable in terms of the frequency of multiple pregnancy and preterm birth and the mean maternal age, among other variables. However, the comparative analysis identified some statistically significant differences. Preconception folic acid supplementation, conception after more than 1 year of trying and female offspring were more frequent in mothers in the ART group, while monochorionic multiple pregnancies were more frequent in the control group.
Comparison of general characteristics of cases and controls.
| Cases | Controls | P | |
|---|---|---|---|
| Sex (female) | 55.8% | 40% | .001 |
| Mean MA | 33.41 | 33.42 | .400 |
| MG | 23.5% | 24% | .350 |
| Monochorionic MG | 11% | 31% | .017 |
| Preterm birth | 24.6% | 23.5% | .780 |
| Mean GA (weeks) | 37.7 | 37.8 | .690 |
| Tobacco | 13.8% | 17.8% | .258 |
| Toxin exposure | 16% | 19% | .300 |
| TTC >1 year | 94% | 7.9% | <.001 |
| PCFAS | 65% | 42% | <.001 |
| FHx of major CM* | 7.35 | 11% | .245 |
| FHx of genetic disorder | 2.6% | 2.4% | .897 |
FHx, family history; GA, gestational age; MA, maternal age; MG, multiple gestation; PCFAS, preconception folic acid supplementation; TTC, time to conception.
We found major CMs in 7.8% of children born after ART, most frequently cardiac malformations (52%; 10/19): surgically treated pulmonary valve stenosis,1 bicuspid aortic valve,1 mitral valve insufficiency,1 atrial septal defect (ASD)6 and ventricular septal defect (VSD).3 Another 21% (4/19) were central nervous system (CNS) malformations: hydrocephalus and dysmorphic lateral ventricles,1 agenesis of corpus callosum,3 cortical and vermian atrophy1; 21% genitourinary (4/19): hydronephrosis, cryptorchidism, hypospadias and horseshoe kidney; one child had an epigastric hernia and one congenital ptosis.
On the other hand, minor malformations were detected in 53% of these children, most frequently pigmented lesions (PLs) (33%; 77/231). Of these children, 83% had café-au-lait spots (CALS) and 17% diffuse hyperpigmentation and/or hypopigmented macules. Multiple CALS (MCALS, 2 or more) were present in 10.4%, and 22.4% had vascular anomalies (VAs): capillary malformation (20.6%), infantile haemangioma (4.7%) and 1 case of venous malformation in the right hand. The rest of the detected anomalies were: umbilical hernia (6%), genitourinary anomalies (phimosis, hydrocoele, pyelectasis) (4.3%), supernumerary nipple (3.4%), strabismus (3%) and nasolacrimal duct obstruction (1.7%).
There was 1 case of multiple congenital anomalies with psychomotor retardation of unknown aetiology.
Congenital malformations in the naturally conceived groupA seemingly isolated major CM was identified in 7.2% of NC children, and cardiac malformations were also the most frequent type in this group (60%; 9/15): pulmonary valve stenosis,3 ASD1 and VSD,6 tetralogy of Fallot1; followed by genitourinary malformations (33%; 5/15): hypospadias,4 renal agenesis.3 There was one case of coronal craniosynostosis that required surgery and 1 case of congenital cystic adenomatoid malformation.
Minor malformations were found in 52.6%, most frequently PLs (42.20%), as was also the case in the ART group. Sixty-seven percent of PLs were CALS. One percent of anomalies were MCALS3; 15% vascular (15%, 31): capillary malformation (12.6%) and infantile haemangioma (3.4%; 7), with no other type of VA found. The remaining minor malformations were umbilical hernia (5.8%; 12), supernumerary nipple (4.3%; 9), genitourinary anomalies (phimosis,5 hydrocoele,3 duplex collecting system3) (3.8%; 8): and strabismus (2.8%).
Comparison of case and control cohortsWe did not find differences in the overall incidence of major or minor CMs between groups (Table 2). When it came to minor anomalies, we did find a higher frequency of capillary malformation and PLs in the ART group at age 3 years. These differences remained in the logistic regression analysis adjusted for various potential confounders such as multiple pregnancy, preterm birth, maternal age, sex, exposure to tobacco during gestation, history of preeclampsia and preconception folic acid supplementation: PLs, OR = 1.92 (95% CI, 1.23–3.08; P = .004), capillary malformation, OR = 1.72 (95% CI, 1.00–2.97; P = .050).
Comparison of major and minor congenital malformations in cases and controls.
| Cases | Controls | P (χ2) | |
|---|---|---|---|
| Major CMs | 7.8% | 7.2% | .829 |
| Minor CMs | 53% | 52% | .902 |
| VAs | 22% | 15% | .057 |
| Capillary malformations | 20% | 12.6% | .031 |
| Haemangioma | 4.76% | 3.4% | .474 |
| PLs | 33.3% | 20% | .003 |
CM, congenital malformation; PL, pigmented lesion; VA, vascular anomaly.
The logistic regression analysis did not detect an association between major CMs and membership in the ART or NC group, but it did find an association between major CMs and male sex (relative risk reduction [RRR], 2.86; 95% CI, 1.27–6.46; P = .011) and twin gestation (RRR, 2.31; 95% CI, 1.00–5.35; P = .050) independently of maternal age, preterm birth, exposure to tobacco, preconception folic acid supplementation and the history of preeclampsia.
We also found a recurrent craniofacial pattern in 68% of the ART group that had not been described previously, characterised by a prominent forehead, midface hypoplasia, epicanthus, full cheeks and a thin upper lip (Fig. 3).
The facial recognition software (http://suite.face2gene.com) used to analyse controls, patients with FAS and children born after ART allowed the distinction of the 3 different patterns (Fig. 4).
All binary comparisons gave rise to a receiver operating characteristic (ROC) curve with very large areas under the curve and p-values of less than 0.001 (Fig. 5).
We performed a univariate analysis of the factors potentially associated with this craniofacial pattern, which found a statistically significant association with the presence of neurodevelopmental disorders (P = .016), maternal age less than 35 years (P = .033) and male sex (P = .025).
Study of ART-related factors potentially associated with the presence of CMs in the case groupWe found major CMs in 7.8% of children born after ART. The univariate analysis only found an association with the cause of infertility. We only found 1 case of major CM in the female infertility group (3.3%) compared to an incidence of 40% in the unexplained infertility (UI) group. The logistic regression analysis found that UI was a significant risk factor for major CMs (OR, 11.9; 95% CI, 2.06–69.64; P = .006).
We did not find any factors associated with minor CMs overall, and when it came to the most frequent types, there was only an association between PGD and PLs. Eighty percent (4/5) of children born after PGD had PLs (P = .037). Minor CMs were not associated with a history of preeclampsia, gestational diabetes or tobacco exposure during gestation. The small sample size did not allow performance of logistic regression analysis.
DiscussionMany studies on the health problems found in individuals born after ART have differentiated between singleton and multiple pregnancies and stratified risk based on maternal age, but to our knowledge, this is the first one to carry out a prospective follow-up in a group of children born after ART and a group of matched controls comparable in terms of the frequency of multiple pregnancy, preterm birth and maternal age, in which we also achieved a high participation rate (approximately 90%). The only relevant factor that we could not avoid to be able to essentially attribute outcomes to the use of ART was subfertility (failure to conceive after 1 year of unprotected regular sexual intercourse), which was only identified in 7.8% of couples with NC children. However, since ART is associated with difficulty conceiving (except, generally, cases of PGD), and this is the only option available for many couples to be able to conceive, we think that for the purpose of counselling, it would be more appropriate to consider the risks associated with subfertility and with ART as a whole.
Chief among the findings of the study is that, despite the higher incidence of major CMs in the ART group (7.8%), the comparison with the control group did not evince significant differences, contrary to the conclusions of the most recent meta-analysis on the subject.10 The high incidence of CMs in both groups was probably due to the characteristics of the populations under study (frequencies of multiple gestations and preterm birth of 24%–25%) and the study design: prospective study with follow-up through age 3 years, which allowed the detection of malformations not diagnosed at birth. This suggests that the criteria used to select the control group should be contemplated as potential key factors associated with the morbidity described in the literature focused on this population, as opposed to ART itself. Couples must receive adequate information, and age should be taken into account in the interpretation of success rates, in addition to its potential effects on health during gestation and the future health of the offspring. Our findings also support the growing practice of single-embryo transfer24 to reduce the frequency of MG and the associated frequency of preterm birth, aspects that couples must also be informed about.
We did find an increased risk of certain minor anomalies, such as PLs, MCALS and capillary malformations in the ART group, an association that had not been described in the previous literature. As we already noted, ART had been identified as a risk factor for infantile haemangioma in the past, but in our study, while we found a greater incidence of this anomaly in the ART group (4.76% vs 3.4%), the difference was not statistically significant after adjusting for sex, preterm birth, multiple gestation and other possible confounders. The identified association between ART and minor cutaneous abnormalities, while not clinically relevant per se, is of great interest, as the presence of PLs, particularly MCALS (found in 10% of cases in our series), has been found to be associated to other developmental disorders, epilepsy25 and some forms of cancer, such as acute lymphoblastic leukaemia, in the previous literature.26 We ought to note, however, that the association with cancer is currently under debate. A recent study conducted in Brazil did not find a higher prevalence of MCALS in patients with solid tumours.27 Thus, further research is required to confirm these associations, and long-term follow-up of this and other cohorts is necessary to establish potential long-term risks.
We also found a recurrent craniofacial pattern that had not been described in the past and associated with abnormal neurodevelopment. If we considered both disorders to be manifestations of deviations from normal development in the early stages of embryogenesis, as proposed by Seggers et al.,28 these findings suggest the possibility of mild changes in embryonic development associated with the use of ART that could give rise to minor anomalies at the facial level and more serious problems in a small percentage of cases. The association with male sex and younger maternal age is also interesting, as it suggests a potential role of the hormonal milieu. Assuming that younger women respond more strongly and have higher levels of estradiol, and given the higher frequency of the identified craniofacial pattern in male offspring, oestrogen levels may play a role in its development.29
It is essential that clinicians, especially those involved in the evaluation of patients with multiple CMs or neurodevelopmental disorders, be aware of this phenotype, as craniofacial features are often the starting point that eventually leads to diagnosis. At times, they may mask or hinder diagnosis or lead to performance of additional diagnostic tests.
ConclusionOur study found a high prevalence of major CMs in both groups, without statistically significant differences between them. The incidence of minor anomalies was similar to the incidence described in individuals born after ART and the subfertile population, and we also did not find significant differences between the ART or NC groups for these anomalies.
This study is the first to describe an increased risk of PLs, MCALS and capillary malformation in individuals born after ART, independently of the order of the pregnancy and sex. We found an association between PLs and PGD, despite the small number of children conceived after PGD. We also unexpectedly identified a recurrent craniofacial pattern in children born after ART that had not been previously described. Further research is required to confirm these associations.
None of the ART-specific factors under study were associated with these anomalies, but we found an association with multiple gestation, which reinforces the important role of this factor in abnormal embryonic development. Couples need to be informed of these outcomes before initiation of treatment, emphasising the need to transfer only one embryo whenever possible.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank all participants, parents as well as children, for making themselves available and their collaboration. The results presented here were obtained in the context of a doctoral dissertation titled “Evaluación de salud y desarrollo de niños hasta los 3 años de edad concebidos por técnicas de reproducción asistida.”
Please cite this article as: Sánchez Soler MJ, López-González V, Ballesta-Martínez MJ, Gálvez-Pradillo J, Nicolás-Arnao M, Gómez-Sánchez E, et al. Riesgo de malformaciones mayores y menores en niños concebidos por técnicas de reproducción asistida (FIV/ICSI): estudio prospectivo de cohorte controlado. An Pediatr (Barc). 2021;95:448–458.