Paediatric multi-system inflammatory syndrome temporally related to SARS CoV-2 (PIMS-TS) is a disease described in relation to active or recent infection by SARS-CoV-2. Although the aetiology and pathogenesis of PIMS-TS are still unclear, it is believed that it could involve a process of immune dysregulation triggered by SARS-CoV-2. It affects a small proportion of children that acquire the infection, although the case definition also comprehends young adults aged less than 21 years.1
We describe a clinical case that stood out due to the associated presence of cervical manifestations and retropharyngeal oedema, mimicking an abscess. Given the complexity and potential severity of the disease, active watchfulness and early detection are essential to start treatment as soon as possible.
The patient was a healthy male adolescent aged 17 years that presented in the adult emergency department with fever of 5 days’ duration peaking at 39 °C, nonspecific cervical pain, progressive malaise and cutaneous lesions.
The physical examination revealed dry and cracked lips, absence of tonsillar exudate, pain on palpation in the inferior posterior cervical region, with no evidence of lymph node involvement or stiffness in the neck. This was associated with a macular rash in the trunk and extremities that faded with application of pressure. The vital signs on arrival were: temperature, 39 °C; oxygen saturation (SatO2), 97%; heart rate (HR), 126 bpm, blood pressure (BP), 121/68 mmHg.
The salient laboratory findings were: lymphopenia (lymphocytes, 270 cells/mm3), mild thrombopenia (platelets, 93 000/mm3), coagulation changes (prothrombin time, 51%; INR 1,57; fibrinogen, 682 mg/L, activated partial prothrombin time [aPTT], 30 s), changes in renal function (creatinine, 1.34 mg/dL), hyponatraemia (sodium, 125 mEq/L); creatinine kinase, 309 U/L; acute phase reactant elevation (C-reactive protein [CPR], 348.4 mg/L and procalcitonin [PCT], 30.99 ng/mL). The SARS-CoV-2 polymerase chain reaction (PCR) test was positive (3.17 log copies/mL), and the chest radiograph did not evince any abnormalities.
Since sepsis was suspected at the outset, the patient received empiric antibiotherapy with intravenous vancomycin and ceftriaxone and intravenous fluids. Later, due to the presence of fever and neck pain, consultations were made with the neurology department, which recommended performance of a cranial computed tomography (CT) scan and lumbar puncture, and the cardiology department, which assessed the patient with an echocardiogram. These tests did not find any abnormalities, prompting a consultation with the internal medicine department, which recommended performance of a cervical CT scan.
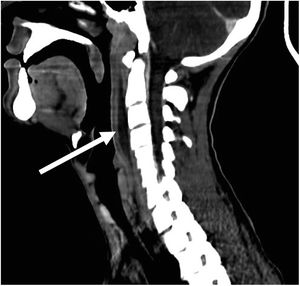
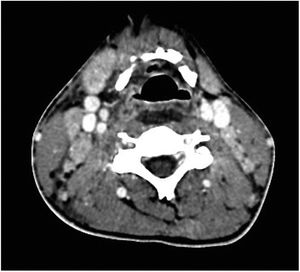
The cervical CT scan revealed a rim-enhancing fluid collection measuring 7.5 × 3.3 × 0.9 cm, in the retropharyngeal space, extending from C2 to C6 (Fig. 1), and bilateral reactive enlargement of multiple lymph nodes in the sides of the neck (Fig. 2). The detection of a potential retropharyngeal abscess led to consultation with the otorhinolaryngology department, which resulted in the broadening of the antibiotherapy spectrum with the addition of meropenem and clindamycin, as well as surgical management. The patient underwent a posterior pharyngotomy, with performance of punctures at different levels of the posterior wall, in which no samples were obtained for culture.
The patient was admitted to the intensive care unit (ICU) in the immediate postoperative period, where he became haemodynamically unstable and exhibited sudden and progressive respiratory impairment in the first 24 h, with an increase in oxygen requirements, tachypnoea and increased work of breathing, prompting intubation and initiation of mechanical ventilation. The chest radiograph showed infiltrates compatible with acute pulmonary oedema and there was a marked impairment of cardiac function, with a left ventricular ejection fraction (LVEF) of 20%.
This picture, combined with the history of infection by SARS-CoV-2 confirmed by a positive PCR test (6.72 log copies/mL) 3 weeks prior, met the full criteria for diagnosis of PIMS-TS.2 The patient started treatment with a steroid (methylprednisolone, 1 g for 5 days, with progressive tapering until heart function normalised), administration of intravenous immunoglobulin (1 g/kg/dose) for 2 days, and anticoagulant therapy. This achieved gradual improvement of symptoms and laboratory parameters, allowing discontinuation of inotropic and respiratory support in the days that followed. At discharge, cardiac function was normal.
Although the literature on the subject is scarce, similar cases have been described in the past. In every instance, patients presented with cervical symptoms and imaging features indicative of retropharyngeal oedema, and required treatment with steroids and intravenous immunoglobulin.3,4 Thus, it is important to keep in mind that in some cases PIMS-TS may manifest with retropharyngeal oedema, which may be confused with an abscess. Keeping a high level of suspicion and early detection of the syndrome are essential, given the associated morbidity and mortality and it needing treatment that is different from the one required for the infection.
The pathophysiology of PIMS-TS remains unknown, although its development could be explained by the increased vascular permeability that characterises the syndrome, which is also a feature of Kawasaki disease.5,6 In the case series published by Au et al.,6 the authors emphasised the importance of an adequate differential diagnosis, including Kawasaki disease, even atypical forms, given the favourable outcomes with immunoglobulin therapy, as it can prevent unnecessary surgical interventions.
Lastly, we must insist on the importance of keeping a high level of suspicion for PIMS-TS, given its potential severity. This syndrome must always be included in the differential diagnosis of young patients presenting with fever and a history of SARS-CoV-2 infection.
FundingThis research did not receive any external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.