Acute pyelonephritis (APN) is one of the most common causes of serious bacterial infection in infants. Renal scarring is the most prevalent long-term complication.
ObjectivesTo review the incidence of renal scarring within 6 months after an episode of APN in children under 36 months and its relationship with imaging studies, clinical settings, and bacteriology.
MethodA retrospective study of previously healthy patients aged one to 36 months, admitted for a first episode of APN, with a minimum follow-up of 6 months. Demographic and clinical variables were collected along with bacteriology, renal and bladder ultrasound scan, voiding cystourethrography, DMSA-scintigraphy, and re-infection events.
ResultsA total of 125 patients were included in the study, of which 60% were male, the large majority (92%) febrile, and due to Escherichia coli (74.6%). There was a history of prenatal ultrasound scan changes in 15.4%. Ultrasound scan found dilation of the urinary tract in 22.1%. Voiding cystourethrography was performed on 70 patients: 54.3% no abnormalities, 12.8% vesicoureteral reflux (VUR) grade i-iii, and 32.9% iv-v grade VUR. Six patients had iv-v grade VUR with a normal ultrasound scan. Adherence to DMSA-scintigraphy at 6 months was only 61% of that indicated. Renal scarring was found in 44.3% of those in which it was performed (60 cases).
ConclusionsAlmost half (44%) DMSA-scintigraphy in children aged one to 36 months hospitalised for APN show renal scarring at 6 months, which was found to be associated with the re-infection events and the iv-v grade VUR. There was no relationship between scarring and the bacteriology or the elevations of inflammatory biochemical markers.
Una de las causas más frecuentes de infección bacteriana grave en lactantes es la pielonefritis aguda (PNFA), cuya secuela más prevalente a largo plazo es la instauración de cicatrices renales.
ObjetivosRevisar la incidencia de cicatrices renales a los 6 meses de un episodio de PNFA en niños menores de 36 meses y su relación con la clínica, las pruebas de imagen y la bacteriología.
MétodoEstudio retrospectivo de pacientes de uno a 36 meses previamente sanos ingresados por un primer episodio de PNFA, con un seguimiento mínimo de 6 meses. Se recogieron las variables demográficas junto con bacteriología, ecografía, cistourografía miccional seriada, recidivas y gammagrafía-DMSA.
ResultadosSe incluyeron 125 pacientes, 60% varones, la mayoría febriles al ingreso (92%), debido a E. coli (74,6%). Existía antecedente de alteración ecográfica prenatal solo en el 15,4%. La ecografía detectó dilatación de la vía urinaria en el 22,1%. En 70 pacientes se indicó cistourografía miccional seriada: 54,3% sin anomalías, 12,8% con reflujo vesicoureteral (RVU) grado i-iii y 32,9% con RVU iv-v. Seis pacientes presentaban RVU iv-v con ecografías normales. La adherencia a la gammagrafía DMSA a los 6 meses fue solo del 61% de los indicados. De los efectuados (60 casos), en un 44,3% se hallaron cicatrices renales, relacionadas significativamente con la recurrencia y el RVU iv-v, pero no con la bacteriología ni con la elevación de reactantes.
ConclusionesEl 44% de las gammagrafías-DMSA de pacientes de uno a 36 meses hospitalizados por PNFA desarrolla cicatrices renales a los 6 meses. Estas se relacionaron con las recurrencias y el RVU grave, pero no con la bacteriología y los reactantes inflamatorios.
The approach to the diagnosis and management of urinary tract infection (UTI) in children is complex, especially in young infants that may have especially severe forms of disease, with a high percentage of patients developing sequelae in the form of renal scarring that have variable impact in the long-term. The indications for imaging tests have been changing in recent years with the publication of different clinical guidelines.1–4 The main changes have been based on systematic literature reviews, taking into account the association of microbiological, ultrasound and cystography findings with long-term sequelae and UTI recurrence. Several practical approaches that have been proposed recently illustrate the difficulty in reaching a consensus about decision making in the management of UTIs during acute infection and after treatment to assess the impact on renal function. These approaches also identify the presence of underlying disease and prevent potential recurrences.2–5 There are few studies on this subject,6,7 especially in our region.8 In this study, we reviewed the outcomes of children aged less than 36 months admitted for severe UTI, analysing the presence of renal scarring in relation to clinical manifestations, medical history and imaging test results.
Patients and methodsWe conducted a retrospective study by reviewing the medical records of patients aged less than 36 months admitted to a tertiary care hospital that met the criteria for a first episode of upper urinary tract infection: probable acute pyelonephritis (APN) defined as leukocyturia and evidence of urinary pathogen growth in urine collected by catheter following previously established criteria,4,9 in the presence of fever and/or decline of general health status and/or elevated levels of acute phase reactants4 (C reactive protein [CRP]>20mg/L and/or procalcitonin [PCT]>0.5ng/mL), with a minimum duration of followup of at least 6 months. The study comprehended the period between January 2010 and December 2014. The standardized antibiotherapy approach consisted of treating infants aged less than 3 months with ampicillin and gentamicin, and older children with gentamicin alone until antimicrobial susceptibility test results became available. The exclusion criteria were: UTI occurring in the context of surgery, nosocomial infection, previous or current urinary catheterization, and UTI secondary to a confirmed obstructive uropathy or limited to the lower urinary tract. We also excluded newborns aged less than 4 weeks, as UTI in these cases could be considered a manifestation of a potential generalized neonatal infection.
We collected data for the following variables in each patient: age; sex; duration of symptoms in days at time of admission; fever at admission; nephrourologic abnormalities in prenatal ultrasound (dilation anywhere in the urinary tract or structural malformations); acute phase reactant levels (CRP measured by turbidimetric immunoassay; PCT measured by enzyme-linked fluorescent immunoassay, creatinine at time of admission by means of the modified Jaffé kinetic method [bichromatic spectrophotometry, 510 and 600nm]); abnormal findings in basic urinalysis; pathogen isolated in culture of urine specimen obtained by catheter; results of blood culture, urinary tract ultrasound and serial voiding cystourethrography (VCUG) performed early during admission; recurrent UTI episodes in the months following admission; and dimercaptosuccinic acid (DMSA) scintigraphy at least 6 months after the resolution of the first episode of APN.
We categorized a few quantitative variables for the purpose of analysis. We divided age into three categories: less than 3 months, 3–6 months, and greater than 6 months. We categorized PCT levels into less than 0.5ng/mL, 0.5–1ng/mL, and greater than 1ng/mL. We categorized C reactive protein by quartiles. Urologic ultrasound comprised three categories: urinary tract dilation, lobar nephronia/renal abscesses, and complex malformations. The results of VCUG were divided into three categories: normal, reflux grade I–III, and reflux grade IV–V. Bacteriological results were divided into two categories: Escherichia coli (E. coli) and pathogen other than E. coli. Duration of symptoms was divided into less than one day and more than one day.
Following the general guidelines that applied during the period under study,1,3–5 VCUG was indicated in patients with clinical sepsis, isolated pathogen other than E. coli, sonographic abnormalities or siblings with urinary tract abnormalities. DMSA scintigraphy was indicated in infants aged less than 6 months and all patients with abnormal ultrasound findings, pathogen other than E. coli, septic appearance, persistent fever more than 48h after initiating antibiotherapy, micturition abnormalities, dehydration or elevated creatinine at least 6 months after infection. Imaging studies were considered abnormal when cortical tracer uptake was reduced. The results were divided in two categories: normal and abnormal.
We present quantitative data as mean and standard deviation, and qualitative data as frequency percentages. We analyzed the association between qualitative variables and the presence of lesions in DMSA scintigraphy by means of the χ2-test. Variables for which the association corresponded to a p-value of less than .20 were included in a binomial logistic regression analysis with the purpose of identifying independent risk factors for the presence of abnormalities in DMSA scintigraphy. We conducted the statistical analysis with the PSPP statistical software (GNU© General Public License by the Free Software Foundation).
ResultsThe study included a total of 125 healthy patients. Table 1 presents patient data for quantitative variables. Sixty percent of the patients were male; 52.8% were aged less than 3 months, 72.0% less than 6 months and 87% less than 12 months. Eight percent of cases had onset without fever. In 46.7%, symptom duration at admission was less than one day. As for diagnostic tests, the reagent strip test was positive (defined as a result corresponding to two or more crosses) for leukocyte esterase in 84% of cases, and for nitrites in 45%.
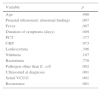
Main descriptive statistical results for the data collected at the time of hospital admission for the first episode of upper urinary tract infection.
| N | Minimum | Maximum | Mean | Standard deviation | |
|---|---|---|---|---|---|
| Age (months) | 125 | 1 | 36 | 5.59 | 7.68 |
| Fever (°C) | 120 | 36.00 | 41.00 | 38.87 | 0.84 |
| Duration of symptoms | 117 | 0 | 14 | 1.53 | 2.42 |
| C reactive protein (mg/L) | 121 | 20 | 358 | 98.85 | 82.35 |
| Procalcitonin (ng/mL) | 86 | 0.5 | 79 | 6.54 | 12.82 |
| Plasma creatinine (mg/dL) | 87 | 0.10 | 1.70 | 0.42 | 0.22 |
The pathogen isolated in 125 of the urine cultures was E. coli (74.6%), followed by Klebsiella pneumoniae (8.9%), Enterococcus faecalis (7.3%), Pseudomonas aeruginosa (3.2%), Proteus mirabilis (1.6%), Enterobacter cloacae (1.6%) and other. Of the total blood cultures performed (108), 7.4% were positive.
Ultrasound detected nephronia, renal abscess or complex malformations in 16.7% and some type of urinary tract dilation in 21.9%. A VCUG was ordered in 70 patients; 54.3% had normal results, 12.8% had reflux grade I–III, and 32.9% reflux grade IV–V. Six patients had grade IV–V vesicoureteral reflux (VUR) with normal ultrasound results, and four of these patients developed renal scarring. Investigation with a DMSA scan was indicated in 80% of cases of APN, but was only performed in 61% of these cases due to parental non-adherence. Out of the sixty cases in which it was finally performed, some degree of renal scarring was found in 44%. In our case series, 13.4% of the patients had a history of abnormal findings in the urinary tract on prenatal ultrasound. We found a recurrence rate in the first six months of follow-up of 15.2%.
Table 2 shows the comparative analysis of abnormalities in the DSMA scintigraphy examination at six months. We found a statistically significant association with the presence of abnormalities in prenatal ultrasound, involvement of a pathogen other than E. coli, and recurrent UTI. We did not find an association between the presence of renal lesions and patient age or elevation of acute phase reactants.
Statistical significance of comparison by χ2 test of abnormal dimercaptosuccinic acid scintigraphy findings and other variables under study.
| Variable | p |
|---|---|
| Age | .490 |
| Prenatal ultrasound: abnormal findings | .007 |
| Fever | .007 |
| Duration of symptoms (days) | .089 |
| PCT | .377 |
| CRP | .973 |
| Leukocyturia | .396 |
| Nitrituria | .107 |
| Bacteriuria | .770 |
| Pathogen other than E. coli | .002 |
| Ultrasound at diagnosis | .001 |
| Serial VCUG | .001 |
| Recurrence | .001 |
CRP, C reactive protein; PCT, procalcitonin; VCUG: voiding cystourethrography.
The logistic regression analysis identified the presence of reflux of grade IV–V in VCUG and UTI recurrence as risk factors, while the peak temperature of fever was identified as a weak protective factor (Table 3).
Variables that were statistically significant in the logistic regression analysis, odds ratio and 95% confidence interval.
| Significance: p | OR | 95% CI | |
|---|---|---|---|
| Fever | .005 | 0.967 | 0.945–0.990 |
| VCUG: VUR grade IV–V | .006 | 6.419 | 1.688–24.413 |
| Recurrence | .017 | 7.592 | 1.433–40.213 |
CI, confidence interval; OR: odds ratio; VCUG: voiding cystourethrography; VUR, vesicoureteral reflux.
The potential for developing sequelae in the form of renal scarring is the leading factor in current guidelines for deciding the diagnostic tests to be performed in cases of severe UTI, which are more frequent during childhood. Few studies make reference to the potential long-term sequelae or the probability of recurrence of these diseases in our region. Thus, we thought it would be interesting to determine the potential correlation of development of renal scarring with updated local microbiology and ultrasound and scintigraphy findings in order to establish an appropriate protocol for treatment and for determining the need for diagnostic and follow-up tests, for the purpose of optimizing long-term outcomes in adulthood while avoiding performance of unnecessary tests.
There had been abnormal ultrasound findings in 38.6% of cases. Most frequent among them were nephronia and dilation of the urinary tract, which was consistent with the previous literature.10–15 The findings of DMSA scintigraphy were abnormal in 44% of the patients. Therefore, we estimated the overall percentage of patients with some type of long-term renal damage at 22%, somewhat higher than the figure reported in a previous systematic review,15 although the latter included patients up to age 19 years with any type of UTI, febrile and afebrile, of whom 57% had a history of previous abnormal findings on DMSA scintigraphy. When no other indication criteria are applied, the percentage of cases of febrile UTI in which there is evidence of renal damage in acute phase DMSA scintigraphy is as high as 73%.12 Case series that focus on children aged less than 36 months,14 as our study did, have found a lower percentage of renal damage on DMSA scintigraphy of around 12%, but these series involved ambulatory patients and approaches in which the sole indication for DMSA scintigraphy is the presence of abnormal findings in ultrasound. In our opinion, this results in a clear selection bias, and we believe that other criteria such as those applied in our study should be indications for DMSA scintigraphy.4 We also attribute the incidence of scarring that we found to the sample selected for our study, with a predominance of young infants with probable APN that presented with fever and a marked elevation of acute phase reactants. Although PCT has been described as a marker of renal damage with development of scarring in the long term,16 we did not find this association in our series. In this regard, there is no wide consensus regarding the routine measurement of acute phase reactants for assessment of acute disease.10 In research on infants with febrile UTI, DMSA scintigraphy showed renal lesions at 3 months in 51% of the patients, while VUR was found in 25%.11 It is possible that some of the lesions detected by DMSA scintigraphy will have no long-term impact, as suggested by some authors,11 but the circumstances under which this test can be forgone have yet to be established.
In our case series, the association between abnormal findings in VCUG and high-grade (IV–V) reflux and DMSA scan abnormalities remained significant in the multivariate analysis, suggesting that reflux is a predisposing factor for APN but that the latter, in itself, can account for renal scarring regardless of its cause. The authors of the systematic review referred above noted that the presumed association of VCUG and DMSA gammagraphy could be due to confounding factors,15 as nearly all studies find that high-grade reflux is found in only approximately 2.5% of cases of APN, and yet the mean percentage of cases with sequelae detected by DMSA gammagraphy is 25%. In our series, the association emerged as an independent factor in the logistic regression analysis (OR, 6.419). For decades, the presence of VUR has been the focus of interest in the follow-up of UTI, although it is evident that the presence of VUR is neither necessary nor sufficient to develop renal scarring.14
The absence of an association between the development of scarring and isolation of a bacterium other than E. coli in the multivariate analysis is consistent with the recommendations of the most recent clinical practice guidelines for the management of UTI in children, according to which the results of microbial testing are no longer a criteria for the indication of VCUG.1,2,4,5 Perhaps the criterion of the involved bacterium for the indication of DMSA scintigraphy should also be reconsidered.
There has been previous discussion that the association between the abnormalities found in prenatal ultrasound and DMSA scintigraphy may result from a cause of cortical dysplasia that predated UTI and manifests with renal damage detectable in DMSA scintigraphy that may progress to renal failure regardless of the subsequent treatment of the associated VUR, which is usually of a high grade.17,18 A larger sample of cases may be able to evince the association that is suggested by the χ2-test.
As reported in other series, we found a statistically significant association between recurrence of APN and renal damage, and recurrence was identified as a risk factor (OR, 7.52). We do not know the role that the genetic susceptibility to UTI previously described in the literature19 may have played in our series. In this regard, the best preventive measure is early detection of reinfection and its prompt treatment, as has been proposed,1,4,5 while the need for antibiotic prophylaxis in reflux cases is increasingly disputed.5,20
Lastly, we would like to mention the protective effect (albeit a weak one) of fever in relation to the development of scarring, as a mechanism that is a nonspecific response to infection. We have not found any studies that analyzed or referred to this aspect.
Some of the limitations of the study were the lack of long-term follow-up of the impact of the detected renal scarring, as well as the lack of data on recurrence beyond the first six months from the first episode of APN. The sample consisted of severe cases with a predominance of infants younger than 6 months of age with a marked elevation of acute phase reactants, and thus our conclusions apply to this specific subset of patients with APN, on whom, as we mentioned before, few data are available.
ConclusionsThe presence of renal scarring at 6 months reached 44% with the selection criteria for DMSA scintigraphy applied in our study of patients hospitalised with severe disease. In our study, recurrence and high-grade VUR were risk factors for abnormal DMSA scintigraphy findings. Raised body temperature in the fever variable appeared as a weak protective factor. We did not find an association with the isolation of pathogens other than E. coli. We think it is justified to propose eliminating the isolation of a pathogen other than E. coli as an indication for ordering a DMSA scan.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Rodríguez-Azor B, Ramos-Fernández JM, Sánchiz-Cárdenas S, Cordón-Martínez A, Carazo-Gallego B, Moreno-Pérez D, et al. Cicatrices renales en menores de 36 meses ingresados por pielonefritis aguda. An Pediatr (Barc). 2017;86:76–80.