To analyse the relationship between previous severity of illness, lactic acid, creatinine and inotropic index with mortality of in-hospital cardiac arrest (CA) in children, and the value of a prognostic index designed for adults.
MethodsThe study included a total of 44 children aged from 1 month to 18 years who suffered a cardiac arrest while in hospital. The relationship between previous severity of illness scores (PRIMS and PELOD), lactic acid, creatinine, treatment with vasoactive drugs, inotropic index with return of spontaneous circulation and survival at hospital discharge was analysed.
ResultsThe large majority (90.3%) of patients had a return of spontaneous circulation, and 59% survived at hospital discharge. More than two-thirds (68.2%) were treated with inotropic drugs at the time of the CA. The patients who died had higher lactic acid before the CA (3.4mmol/L) than survivors (1.4mmol/L), p=.04. There were no significant differences in PRIMS, PELOD, creatinine, inotropic drugs, and inotropic index before CA between patients who died and survivors.
ConclusionA high lactic acid previous to cardiac arrest could be a prognostic factor of in-hospital cardiac arrest in children.
Analizar si el estado de gravedad previo, el láctico, la creatinina y el índice inotrópico se relacionan con la mortalidad de la parada cardiaca (PC) intrahospitalaria en niños y si un índice de predicción pronóstica diseñado para adultos tiene utilidad en pediatría.
MétodosSe estudió a 44 niños de edades entre un mes y 18 años de edad que presentaron una PC en el hospital durante un período de 2 años. Se analizaron la relación entre las puntuaciones de gravedad PRIMS y PELOD, el láctico, la creatinina, el tratamiento previo con fármacos vasoactivos, el índice inotrópico con la recuperación de la circulación espontánea (RCE) y la supervivencia.
ResultadosUn 90,3% de los pacientes recuperaron la circulación espontánea y un 59% sobrevivió al alta del hospital. Un 68,2% de los pacientes recibían inotrópicos previos a la PCR. Los pacientes fallecidos presentaban valores de lactato previos a la parada más elevados (3,4mmol/L) que los supervivientes (1,4mmol/L), p=0,04. No existieron diferencias en las puntuaciones de PRISM, PELOD, los valores de creatinina, el tratamiento con inotrópicos, con adrenalina, el número de inotrópicos, o el índice inotrópico antes de la PCR entre fallecidos y supervivientes.
ConclusiónLa elevación de ácido láctico previa a la parada cardiaca puede ser un indicador de mal pronóstico en la PC en los niños.
Between 50 and 70% of in-hospital cardiac arrests (CA) take place in a paediatric intensive care unit (PICU).1–4
Various authors have analysed the characteristics of CAs and the factors associated with in-hospital CA prognosis in children,1–9 but no studies have assessed whether severity of illness prior to CA is associated with return of spontaneous circulation (ROSC) and survival.
A scoring system for predicting the prognosis of out-of-hospital CA in adults has been developed and reported,10 and its application to in-hospital CA has also been evaluated.11
The aim of this study was to analyse whether previous severity of illness, measured by paediatric severity scores, prognostic scores for adult CA, other markers such as lactic acid and creatinine, and the treatments given to patients such as mechanical ventilation and inotropic drugs, are associated with in-hospital CA mortality in children.
Patients and methodsWe conducted an observational prospective study that included paediatric patients aged one month to 18 years who had in-PICU CA between December 2007 and December 2009. We collected the data following the Utstein style guidelines.12,13 We excluded infants under one month of age and patients who only had respiratory arrest.
We included the following variables: age, sex, weight, cause and type of CA, assisted respiration, administration and dosage of inotropic drugs, inotropic index, blood pressure, heart rate, lactate, creatinine, paediatric prognostic scores, Paediatric Risk of Mortality (PRISM)14 and Paediatric Logistic Organ Dysfunction (PELOD)15 prior to CA, and CA prognostic score.10 We recorded the values closest to CA, always within the previous 24h.
We calculated the inotropic index by modifying the formula proposed by Gaies et al.,16 substituting isoprotenerol for vasopressin, which is not commercialised in Spain. Inotropic score (μg/kg/min): dopamine+dobutamine+(adrenaline×100)+(noradrenaline×100)+(isoproterenol×100)+(milrinone×15). The CA prognostic score includes the following variables (initial ECG rhythm, time elapsed to CPR initiation, CPR duration, and pre-arrest creatinine level).10
We defined CA as an abrupt, unexpected and potentially reversible interruption of spontaneuous circulation and respiration requiring cardiac massage and ventilation. We defined ROSC as the return and maintenance of a palpable central pulse for at least 20min. We looked at survival to discharge from hospital.
We performed the statistical analysis with the SPSS software version 18 (SPSS Inc., Chicago, Illinois). The data are expressed as medians and interquartile ranges, P25–P75 [IQR]). We analysed the relationship of each of the parameters with ROSC and survival. We used the chi-squared test to compare percentages, and the Mann–Whitney non-parametric test to compare qualitative variables. We performed univariate logistic regression to analyse the relationship of each of the risk factors with mortality, and analysed the ROC curve to study the predictive ability of lactic acid in relation to mortality. We set the significance value at p<0.05.
ResultsFrom December 2007 to December 2009, we studied 44 patients (15 female and 29 male) admitted to the PICU after a CA. The median age was 15 months (IQR 4–66 months) and the median weight 10kg (IQR 4–18kg).
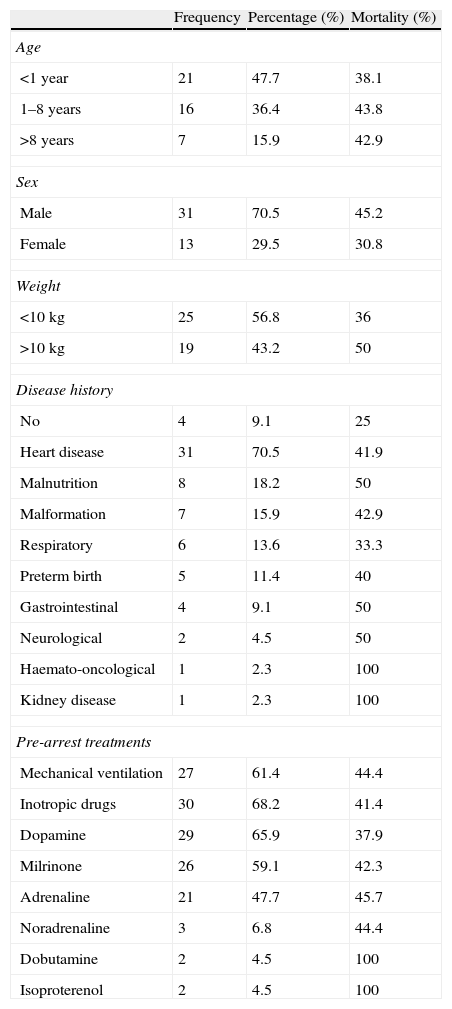
Table 1 summarises the characteristics of the patients and the treatments they were receiving prior to CA. Heart disease was the most frequent cause of CA. In-PICU CA occurred in 70.4% of the patients: 61.4% were receiving mechanical ventilation and 68.2% were receiving inotropic drugs at the time of CA. The median lactate level was 1.7 (IQR 1.1–4.5) and the median creatinine level was 0.40mg/dL (0.2–0.7). The mortality risk according to the PRISM score was 7.6%, and 1.3% according to the PELOD score.
Patient characteristics and pre-arrest treatment. Association with mortality.
| Frequency | Percentage (%) | Mortality (%) | |
| Age | |||
| <1year | 21 | 47.7 | 38.1 |
| 1–8years | 16 | 36.4 | 43.8 |
| >8years | 7 | 15.9 | 42.9 |
| Sex | |||
| Male | 31 | 70.5 | 45.2 |
| Female | 13 | 29.5 | 30.8 |
| Weight | |||
| <10kg | 25 | 56.8 | 36 |
| >10kg | 19 | 43.2 | 50 |
| Disease history | |||
| No | 4 | 9.1 | 25 |
| Heart disease | 31 | 70.5 | 41.9 |
| Malnutrition | 8 | 18.2 | 50 |
| Malformation | 7 | 15.9 | 42.9 |
| Respiratory | 6 | 13.6 | 33.3 |
| Preterm birth | 5 | 11.4 | 40 |
| Gastrointestinal | 4 | 9.1 | 50 |
| Neurological | 2 | 4.5 | 50 |
| Haemato-oncological | 1 | 2.3 | 100 |
| Kidney disease | 1 | 2.3 | 100 |
| Pre-arrest treatments | |||
| Mechanical ventilation | 27 | 61.4 | 44.4 |
| Inotropic drugs | 30 | 68.2 | 41.4 |
| Dopamine | 29 | 65.9 | 37.9 |
| Milrinone | 26 | 59.1 | 42.3 |
| Adrenaline | 21 | 47.7 | 45.7 |
| Noradrenaline | 3 | 6.8 | 44.4 |
| Dobutamine | 2 | 4.5 | 100 |
| Isoproterenol | 2 | 4.5 | 100 |
Spontaneous circulation returned in 40 (90%) patients and 26 (59.1%) survived to hospital discharge. We could not perform a statistical analysis to study the relationship with ROSC because only 4 patients failed to recover spontaneous circulation.
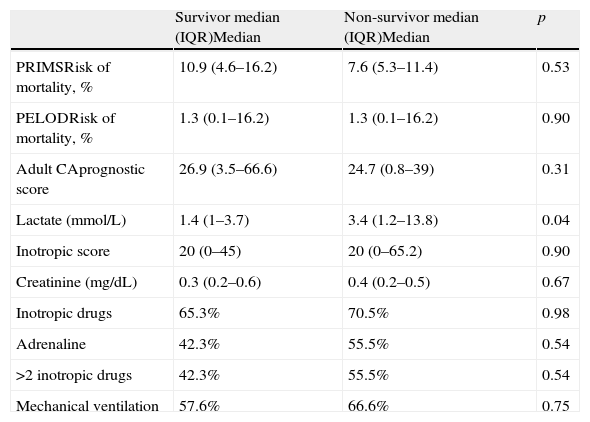
Table 2 compares the parameters of the deceased patients and the survivors in relation to pre-arrest severity of illness and treatments. There were no differences in the PRISM and PELOD paediatric severity of illness scores, in the adult CA prognostic score, nor in the creatinine levels of survivors vs. non-survivors. There was no difference in mortality associated with treatment with inotropic drugs (58.6% of patients who received inotropic drugs survived, as did 64.3% of patients who did not). Patients who were given adrenaline had a lower survival rate (52.4%) than patients who did not receive it (65.2%), although the difference was not statistically significant. There were no statistically significant differences in association with the number of inotropic drugs given to the patients, although none of those who were given 4 or more inotropic drugs survived CA.
Comparison of survivors and non-survivors in relation to severity of illness and pre-arrest treatment.
| Survivor median (IQR)Median | Non-survivor median (IQR)Median | p | |
| PRIMSRisk of mortality, % | 10.9 (4.6–16.2) | 7.6 (5.3–11.4) | 0.53 |
| PELODRisk of mortality, % | 1.3 (0.1–16.2) | 1.3 (0.1–16.2) | 0.90 |
| Adult CAprognostic score | 26.9 (3.5–66.6) | 24.7 (0.8–39) | 0.31 |
| Lactate (mmol/L) | 1.4 (1–3.7) | 3.4 (1.2–13.8) | 0.04 |
| Inotropic score | 20 (0–45) | 20 (0–65.2) | 0.90 |
| Creatinine (mg/dL) | 0.3 (0.2–0.6) | 0.4 (0.2–0.5) | 0.67 |
| Inotropic drugs | 65.3% | 70.5% | 0.98 |
| Adrenaline | 42.3% | 55.5% | 0.54 |
| >2 inotropic drugs | 42.3% | 55.5% | 0.54 |
| Mechanical ventilation | 57.6% | 66.6% | 0.75 |
CA: cardiac arrest; PELOD: multi-organ failure score; PRIMS: risk of mortality prognostic score; CPR: cardiopulmonary resuscitation; IQR: interquartile range.
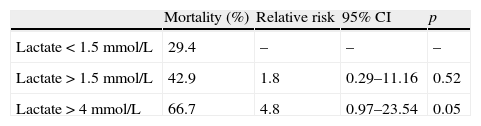
Pre-resuscitation lactate levels in non-survivors were significantly higher than in survivors. Table 3 summarises the relative risk of mortality of pre-arrest lactate values greater than 1.5mmol/L and 4mmol/L. The area under the ROC curve was 0.69 (confidence interval 0.51–0.87), p=0.05. The 4mmol/L cut-off point classified 66.7% of the patients accurately.
Risk of mortality in relation to pre-arrest lactate levels.
| Mortality (%) | Relative risk | 95% CI | p | |
| Lactate<1.5mmol/L | 29.4 | – | – | – |
| Lactate>1.5mmol/L | 42.9 | 1.8 | 0.29–11.16 | 0.52 |
| Lactate>4mmol/L | 66.7 | 4.8 | 0.97–23.54 | 0.05 |
CI: confidence interval.
Lactate>4: sensitivity: 50%, specificity: 80%, positive predictive value: 63.4%, negative predictive value: 69.7%.
Several studies have analysed the relationship between patient characteristics (age, sex) and underlying diseases, the general and neurological performance status, and the causes of CA and CPR characteristics with prognosis after CA in adults and children.1–9 However, few have studied the relationship between the previous health status of the patient and prognosis. Our study is the first to analyse the relationship between severity of illness and prognosis after in-PICU CA.
Prognostic severity scoresThe PRISM and PELOD1–9 scores are validated prognostic indicators for children admitted to intensive care units. However, no previous studies have analysed their prognostic value in children who have CA.
In adults, 2 studies have found that Apache II and III in the first 24h after CA can predict mortality at 30 days.11,17 In our study, neither PRISM nor PELOD measured before CA could predict mortality, although we did not analyse the prognostic value of these scoring systems after CA, as the aim of the study was to analyse prognostic indicators prior to CA.
Cardiac arrest prognostic scoreThe out-of-hospital CA prognostic score integrates some parameters of the previous score (creatinine), the initial ECG rhythm, and CPR characteristics (time to CPR start and CPR duration). A study on adults has shown that this score can also predict prognosis after in-hospital CA in adults.11 In our study, this score showed no prognostic capability. This may be because some of the parameters that are essential in out-of-hospital and in-hospital, out-of-PICU CA, like time elapsed between CA and CPR initiation, have a low discriminatory value in CAs that occur in PICUs, as CPR initiation is almost immediate in these units. On the other hand, this score was developed for adults and, with the exception of CPR duration, which is also the most important prognostic indicator in children, prognostic factors are different in this age group from those found in adults.
LactateLactic acid is one of the markers used most frequently in critical patients to diagnose hypoperfusion and/or tissue hypoxia and to monitor the evolution of treatment, as it has demonstrated prognostic capability and its levels can be measured quickly and easily. However, serum lactate levels can also increase without being a sign of tissue hypoperfusion after adrenaline administration or with the hyperglycaemia that frequently follows CA.18
It is possible that post-arrest lactate level is a prognostic indicator of mortality in patients recovered from CA because it reflects the severity of ischaemia-repercusion injury. Several studies have found that lactate levels in the first 48h after CA are lower in survivors and patients without neurological damage.19–21
Our study is the first to analyse the prognostic value of lactate prior to CA. Our results show that lactic acid was the only pre-arrest severity indicator that could predict prognosis in children who had CA. The predictive capability was 69.5%, despite the relatively small number of patients in the study.
Kidney function (creatinine)Kidney failure is an important mortality factor in critical patients, and it is one of the proven prognostic indicators of mortality in out-of-hospital resuscitation studies in adults. For this reason, serum creatinine was included in the prognostic CPR score for adults.10
De Vos et al. found that, in adults, previous kidney failure is a mortality risk factor in patients who have CA.22 In children, kidney failure prior to CA is a predictive factor for mortality in in-PICU CA2 and in patients who have undergone heart surgery.9 However, our study found no significant difference in pre-arrest creatinine levels between survivors and non-survivors.
This could be due to the fact that creatinine may not be an adequate indicator of kidney function in critically ill children, as increased creatinine levels may occur late or be lower as a result of the malnutrition often occurring in these patients. Furthermore, patients who develop acute kidney failure are treated early with extrarenal purification techniques and may have normal levels of creatinine at the time of CA, as happened in two of our cases. On the other hand, normal creatinine levels vary as a function of age. Therefore, creatinine levels prior to CA should be replaced by classification of kidney function using the AKIN or RIFLE criteria.23
In children who have received CPR for CA, a urine output greater than 1mL/kg/h indicates a favourable prognosis.24 In adults, creatinine levels after CA are prognostic indicators, and improved creatinine values in the first 24h post-arrest (an hourly decrease of 0.2mg/dL in creatinine levels) are a favourable prognostic indicator.25
Administration of vasoactive drugs and inotropic scoring systemsVarious authors have found that patients who were receiving vasoactive treatment at the time of CA have higher mortality.26–28 In a study with adults, Tian et al. 29 found a significant difference in survival between patients who were receiving vasoactive drugs at the time of CPR and those who were not. On the other hand, patients who were given 2 or more vasoactive drugs had a lower survival rate than those who were given only one (6.4% vs. 11.5%, p<0.0001). In children, pre-arrest treatment with vasoactive drugs and adrenaline is a predictor of mortality for in-hospital4,8 and in-PICU1,2 CA.
On the other hand, various studies have used inotropic scores to quantify the degree of haemodynamic support in children after heart surgery, and have found that higher inotropic scores are associated with higher mortality.16,30–32 However, inotropic scores have not been used before to assess CA prognosis in children.
Contrary to what we expected, our study did not find significant differences in survival between patients who received inotropic therapy prior to CA and patients who did not. We also did not find differences in relation to adrenaline or to the number and dosages of inotropic drugs received, which we analysed using the inotropic index.
One of the possible reasons why the results of our study diverge from the rest may have to do with the characteristics of the studied sample. A considerable percentage of the participants included in our study (45.4%) were in postoperative care, for which they received inotropic drugs. This may be partly why inotropic therapy in these patients does not help to differentiate between them when it comes to prognosis. Our results, consistent with those of Parra et al. 7 for children admitted to a paediatric cardiology ICU and those of Ortmann et al. in children with heart disease,9 support this hypothesis. These authors also did not find differences in CPR type and survival between patients who received vasoactive drugs9 or adrenaline7 prior to CA and patients who did not.
However, the inotropic score, which aims to measure the intensity of treatment with inotropes, should have been able to differentiate between patients with greater haemodynamic alteration prior to CA and thus those who are less likely to survive.
Broader multi-centre studies are needed to assess the usefulness of other inotropic scores as prognostic indicators in children with CA and conduct a differentiated analysis of patients in postoperative care for heart surgery.
LimitationsOur study has some limitations. The sample size was relatively small and the study was conducted in a single hospital where a considerable percentage of patients were in postoperative care for heart surgery. We used the PRISM score to evaluate severity of illness, though it has only been validated for assessing the mortality risk in the first 24h after admission to the PICU.
On the other hand, our study did not intend to assess every prognostic factor for in-PICU CA in children, but to analyse the usefulness of a few prognostic scores. For that reason, our analysis did not include other factors that have a significant influence in prognosis, such as age, sex, type of CA, ECG rhythm, or CPR duration and characteristics.
We concluded that children who died after CPR had higher pre-arrest lactate levels than survivors. Since detecting lactic acid levels is easy and quick, lactate could be a good prognostic indicator for CPR in children. Studies are needed to confirm these results and to assess whether there is a lactate cut-off value that could discriminate reliably between patients who will die and patients who will survive.
Creatinine levels, paediatric prognostic scores (PRIMS and PELOD) prior to CPR, the inotropic score and the adult CA prognostic score were not useful in predicting survival of children who receive in-hospital CPR. Thus, prognostic scoring systems specific for in-hospital CA in children need to be developed.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Serrano M, Rodríguez J, Espejo A, del Olmo R, Llanos S, del Castillo J, et al. Relación entre el estado de gravedad previo y el pronóstico de la parada cardiaca intrahospitalaria. An Pediatr (Barc). 2014;81:9–15.