The Autistic Spectrum Disorders (ASD) are characterised by general deficits in social communication, stereotypes, and restricted interests. The ASD have a high prevalence of additional psychiatric disorders that make their daily functioning worse, and reduces their quality of life, as well as that of their families.
Material and methodsIn an effort to identify the environmental characteristics that may explain this high comorbidity, this study has focused on the symptoms of stress and psychological unease of the parents as possible risk factors. A cross-section study was carried out on the relationship between the stress and psychological unease of the parents of pre-school children (2–6 years) with ASD and its relationship with co-existing psychological conditions in children with ASD.
Results and ConclusionsHigh levels of stress and psychological unease in the parents are already associated, since early childhood, with a co-existing psychological condition in that population, specifically with emotional and behavioural problems (P.05). However, further longitudinal studies are needed for a better understanding of the causal relationship between these variables and their possible bidirectional relationship.
Los Trastornos del Espectro Autista (TEA) se caracterizan por deficiencias generalizadas en la comunicación social, estereotipias e intereses restringidos. Los TEA presentan una alta prevalencia de trastornos psiquiátricos adicionales que empeoran su funcionamiento diario y reducen la calidad de vida de ellos y sus familias.
Material y MétodoEn el esfuerzo de identificar características ambientales que expliquen esta alta comorbilidad, esta investigación se ha centrado en la sintomatología de estrés y malestar psicológico de los padres como posibles factores de riesgo. Se realizó un estudio transversal de asociación entre estrés y malestar psicológico de padres de niños preescolares con TEA (2–6 años) y su relación con psicopatología coexistente en niños con TEA.
Resultados y ConclusionesAltos niveles de estrés y malestar psicológico en los padres están asociados ya desde la primera infancia con psicopatología coexistente en dicha población, específicamente con problemas emocionales y conductuales (p < .05). Sin embargo, se necesitan futuros estudios longitudinales para entender mejor la relación causal entre estas variables y su posible relación bidireccional.
Autism spectrum disorder (ASD) is a lifelong severe developmental disorder affecting 1% of the population.1 It is characterized by general impairment in social interactions and communication, stereotyped behaviours and restricted interests. Besides the characteristic features of autism, 70–90% of children with ASD have additional psychiatric comorbidities leading to impaired functioning in everyday activities and a reduced quality of life of patients and their families.2 These comorbidities commonly affect mood (such as anxiety or depression) or behaviour (conduct disorder, oppositional behaviour or hyperactivity). Previous studies show that emotional and behavioural problems are associated more strongly with family functioning3 and parental wellbeing4 than with the symptoms characteristic of ASD.
The most frequent psychiatric comorbidities are anxiety disorders, attention-deficit hyperactivity disorder (ADHD) and oppositional-defiant disorder (ODD).2,5 The prevalence of these disorders in individuals with ASD is 5–10 times greater compared to the general population of children with normal development.
This increase in the prevalence of psychiatric disorders associated with ASD is only partially understood. It is likely that there is an overlap in genetic risk factors between ASD and neurodevelopmental comorbidities, such as ADHD.6 However, this explanation does not seem to apply to comorbid anxiety disorders.7
Research in the general population has rigorously established associations between mental health disorders in children and psychological distress in parents. Studies in the general population have proven that parenting stress8 and mental health problems in parents9 are significantly associated with childhood psychiatric disorders after adjusting for other family-related, child-related and environmental factors. Longitudinal studies have evinced a reciprocal predictive association between emotional and behavioural problems in children and parental mental health, such as presence of depression,10 and certain stressors experienced by parents.11 Although it is possible that a shared genetic component may account for the correlation between psychiatric problems in children and in their parents, genetically sensitive studies have evinced that the environment plays a significant role in intergenerational patterns of anxiety,12 depression13 and behavioural problems.14
However, there are fewer data on the paediatric population with ASD in regard to the role of the family, parenting factors and their association with psychiatric comorbidities. Some authors have found that parental stress,15,16 a controlling parenting style and a chaotic home environment are associated with a higher prevalence of behavioural problems,17 while affection18 and clear boundaries16 from parents are associated with a lower prevalence of behavioural problems in children with ASD. In any case, most of these studies have a cross-sectional design and have not clearly established the direction of the effect.
Parents of children with ASD score high in parental stress scales, even compared to parents of children with other developmental disorders or intellectual or physical disabilities19; an increase in scores that measure other mental health problems has also been observed in the mothers of these children before and after childbirth.20 Research in the general population has shown that parental stress and mental health problems are distinct but associated phenomena, as each of these factors increases the risk of the other.21 For example, since children with ASD are at greater risk of having poor mental health, their ability to meet parental expectations may be compromised. Likewise, intense challenges in parenting can lead to the development of mental health problems in parents.
Transactional models of child development22,23 suggest that parent-child interactions are reciprocal. From a transactional perspective, the presence of ASD symptoms and behavioural problems in children increases parental stress, leading to changes in parental behaviour which in turn reinforce those symptoms and behavioural problems in the child.24
A recent meta-analysis by Yorke et al.25 found a significant strong association between additional emotional and behavioural problems in children with ASD and mental health problems and distress in parents that persisted after controlling for potential confounders.
Our hypothesis is that the association between anxiety and psychological distress is parents may be associated even from early childhood (2–6 years) with emotional and behavioural problems in children with ASD, even after adjusting for variations of ASD in children (in severity of autism, executive functioning and adaptive ability) and sociodemographic characteristics such as parental educational attainment and the age and sex of the child.
Material and methodsStudy sample and data collectionThe study was approved by the Ethics Committee of the Hospital Regional de Málaga on February 23, 2017.
The invitation to participate in the study was made in person to all eligible families through the Child and Adolescent Mental Health Unit of the Hospital Materno Infantil de Málaga in the framework of the Autism Spectrum Disorder Integrated Care Programme of the Regional Government of Andalusia, which serves children with an early diagnosis of ASD aged 2–6 years. To be included, children had to have a clinical diagnosis of ASD based on the criteria of the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) between February 2017 and February 2019, so we obtained a sample of convenience.
The recruitment period lasted 2 years. Of the 149 children referred during this period for suspected ASD, 101 had the diagnosis confirmed through the gold standard of testing, the Autism Diagnostic Observation Schedule-Second Edition (ADOS-2), administered by accredited personnel, and were invited to participate in the study.
The exclusion criteria were absence of confirmation of the ASD diagnosis with the gold standard (ADOS-2), diagnosis of global developmental delay, age less than 2 years or more than 6 years, and lack of completion of the main anxiety and psychological distress scales by the parents (N = 70).
MaterialWe used the Autism Parenting Stress Index (APSI)26 to assess which specific aspects of the child’s health and social functioning caused the highest level of worry and stress in the family. This questionnaire measures aspects specific to families of children with an ASD diagnosis, including worries about communication, social development and future independent living skills, with 13 items grouped into 3 categories: core social disability, difficult-to-manage behaviour, and physical issues. The index has a high internal consistency with an Cronbach α of 0.82.26
We used the Kessler Psychological Distress Scale (K-10)27 as a brief self-report measure of psychological distress in parents/caregivers. This questionnaire consists of 10 items used to produce a global distress score based on the report of symptoms of anxiety and depression experienced in the past 4 weeks. Its internal consistency corresponds to an α of 0.93.28
The Strengths & Difficulties Questionnaire29 (SDQ) parent report was used to assess the severity of emotional and behavioural problems. We used the emotional symptoms and conduct problems subscales of this instrument. The SDQ is used to detect probable mental health disorders and behavioural problems in children aged 2–16 years. It consists of 25 items organised in 5 subscales of 5 items each. Four subscales measure problematic behaviours. These subscales assess emotional symptoms, conduct problems, hyperactivity and peer relationship problems. The fifth subscale assesses positive prosocial behaviours. The 4 subscales that measure problematic behaviours add together to generate a total difficulties score. The internal consistency for the Spanish version of the SDQ parent report corresponds to a Cronbach α of 0.77.30
The Adaptive Behaviour Assessment System-II (ABAS-II)31 is an instrument used to assess adaptive skills from birth to age 6 years. Its purpose is to assess the daily adaptive skills necessary for functioning effectively in the usual environments to determine whether the individual is able to perform activities independently in everyday life without help from others. The ABAS-II comprises 3 adaptive domain scores (conceptual, social and practical) that give rise to an overall adaptive functioning score, or general adaptive composite (GAC), which we used to measure adaptive functioning. The reported internal consistency of this score ranges from 0.97 to 0.99.32
The Behavior Rating Inventory of Executive Function-Preschool version (BRIEF- P)33 is a version of the BRIEF® adapted to children aged 2–6 years. It is used to assess observable behavioural manifestations of executive functioning in everyday living. The questionnaire can be completed by parents and teachers, who report how frequently certain behaviours of the child are problematic. The internal consistency of the parent rating form is 0.83.34
We assessed the presence and severity of autistic symptoms by means of the Autism Diagnostic Observation Schedule, second edition (ADOS-2).35 The ADOS-2 is a standardised semi-structured assessment of communication skills, social interaction and play or imaginative use of materials in individuals with suspected ASD. It comprises 5 modules (T, 1, 2, 3 and 4) that apply depending on the chronological age and language ability of the individual. The ADOS-2 can be applied in a broad age range in individuals with very different levels of development and verbal communication skills. It is considered the gold standard for diagnosis of ASD.36
Statistical analysisWe fitted linear regression models in which the dependent variables were behavioural problems (SDQ, conduct problems) and emotional problems (SDQ, emotional symptoms) and the independent variables were parental anxiety (APSI) and parental distress (K-10). To check the assumptions of the linear regression models, we used the Ramsay regression specification error test (RESET), the Breusch-Pagan test to assess heteroskedasticity and the Shapiro-Wilk test to assess the normality of the residuals. In multivariate models, we assessed colinearity by means of the variance inflation factor (VIF) and investigated age, sex, parental educational attainment, severity of autism (ADOS) and adaptive skills (ABAS) as potential confounders. Initially, the GAC was included as another covariate, but given the high colinearity and variance inflation (VIF > 2) we decided to exclude it from the final multivariate models. We handled missing data in some of the covariates by means of multivariate imputation by chained equations (mice package for R). Since we could not check the assumptions of the linear regression models at once, we verified them separately in each of the 5 imputed data sets. When the independent variable was parental psychological distress and the dependent variable was behavioural problems in the children, the homogeneity of variance assumption was not met, so we fitted a robust regression model instead (with the robustbase package and the lmrob function in R). We set a level of confidence of 95%. All the analyses were performed with the software R version 3.5.1.
ResultsOf the 101 families we invited to participate in the study, 84 agreed, and 70 completed all the assessments and were included in the analysis.
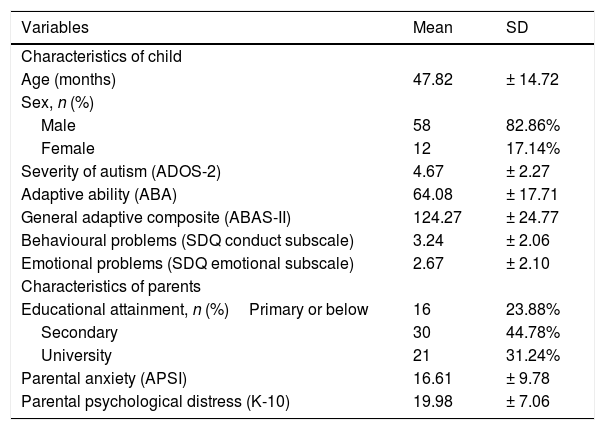
Table 1 describes the sociodemographic characteristics of the sample and the variables under study. Of all children in the sample, 82.86% were male (4:1 ratio), and the mean age was 3 years and 11 months. Only 31.4% of the parents had university degrees.
Descriptive variables.
| Variables | Mean | SD |
|---|---|---|
| Characteristics of child | ||
| Age (months) | 47.82 | ± 14.72 |
| Sex, n (%) | ||
| Male | 58 | 82.86% |
| Female | 12 | 17.14% |
| Severity of autism (ADOS-2) | 4.67 | ± 2.27 |
| Adaptive ability (ABA) | 64.08 | ± 17.71 |
| General adaptive composite (ABAS-II) | 124.27 | ± 24.77 |
| Behavioural problems (SDQ conduct subscale) | 3.24 | ± 2.06 |
| Emotional problems (SDQ emotional subscale) | 2.67 | ± 2.10 |
| Characteristics of parents | ||
| Educational attainment, n (%)Primary or below | 16 | 23.88% |
| Secondary | 30 | 44.78% |
| University | 21 | 31.24% |
| Parental anxiety (APSI) | 16.61 | ± 9.78 |
| Parental psychological distress (K-10) | 19.98 | ± 7.06 |
ABAS-II, Adaptive Behaviour Assessment System; ADOS-2, Autism Diagnostic Observation Schedule; APSI, Autism Parenting Stress Index; K-10, Kessler Psychological Distress Scale; SDQ, Strengths & Difficulties Questionnaire, parent version.
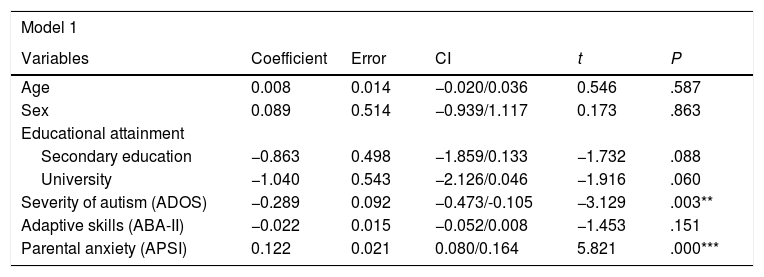
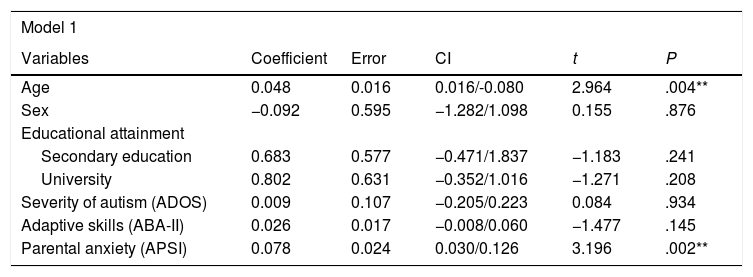
The multivariate regression analyses found a significant association between parental psychological distress and stress and emotional and behavioural problems in children with ASD after controlling for the aforementioned confounders (Tables 2 and 3). In model 1, the independent variable was the stress perceived by parents, and in model 2 it was psychological distress (symptoms of anxiety and depression).
Multivariate regression models, behavioural problems as dependent variable.
| Model 1 | |||||
|---|---|---|---|---|---|
| Variables | Coefficient | Error | CI | t | P |
| Age | 0.008 | 0.014 | −0.020/0.036 | 0.546 | .587 |
| Sex | 0.089 | 0.514 | −0.939/1.117 | 0.173 | .863 |
| Educational attainment | |||||
| Secondary education | −0.863 | 0.498 | −1.859/0.133 | −1.732 | .088 |
| University | −1.040 | 0.543 | −2.126/0.046 | −1.916 | .060 |
| Severity of autism (ADOS) | −0.289 | 0.092 | −0.473/-0.105 | −3.129 | .003** |
| Adaptive skills (ABA-II) | −0.022 | 0.015 | −0.052/0.008 | −1.453 | .151 |
| Parental anxiety (APSI) | 0.122 | 0.021 | 0.080/0.164 | 5.821 | .000*** |
| Model 2 | |||||
|---|---|---|---|---|---|
| Educational attainment | Coefficient | Error | CI | t | P |
| Secondary education | −0.021 | 0.013 | −0.047/0.005 | −1.622 | .110 |
| University | 0.770 | 0.463 | −0.156/1.696 | 1.663 | .101 |
| Severity of autism (ADOS) | |||||
| Educational attainment | −0.448 | 0.691 | −1.830/0.934 | −0.648 | .591 |
| Secondary education | −1.199 | 0.576 | −2.351/-0.047 | −2.184 | .032* |
| University | −0.301 | 0.123 | −0.547/-0.055 | −2.443 | .017* |
| Adaptive skills (ABAS) | −0.012 | 0.013 | −0.038/0.014 | −0.937 | .352 |
| Parental psychological distress (K-10) | 0.173 | 0.032 | 0.109/0.237 | 5.357 | .000*** |
CI, confidence interval. *P < .05; **P < .01; ***P < .001.
Model 1: adjusted R2 = 0.414.
Model 2: adjusted R2 = 0.369.
Multivariate regression models, emotional problems as dependent variable.
| Model 1 | |||||
|---|---|---|---|---|---|
| Variables | Coefficient | Error | CI | t | P |
| Age | 0.048 | 0.016 | 0.016/-0.080 | 2.964 | .004** |
| Sex | −0.092 | 0.595 | −1.282/1.098 | 0.155 | .876 |
| Educational attainment | |||||
| Secondary education | 0.683 | 0.577 | −0.471/1.837 | −1.183 | .241 |
| University | 0.802 | 0.631 | −0.352/1.016 | −1.271 | .208 |
| Severity of autism (ADOS) | 0.009 | 0.107 | −0.205/0.223 | 0.084 | .934 |
| Adaptive skills (ABA-II) | 0.026 | 0.017 | −0.008/0.060 | −1.477 | .145 |
| Parental anxiety (APSI) | 0.078 | 0.024 | 0.030/0.126 | 3.196 | .002** |
| Model 2 | |||||
|---|---|---|---|---|---|
| Variables | Coefficient | Error | CI | t | P |
| Age | 0.034 | 0.018 | −0.002/0.070 | 1.886 | .064 |
| Sex | 0.289 | 0.638 | −0.987/1.565 | 0.452 | .652 |
| Educational attainment | |||||
| Secondary education | −0.335 | 0.607 | −1.611/0.879 | −0.552 | .582 |
| University | 0.943 | 0.662 | −0.381/2.267 | −1.424 | .159 |
| Severity of autism (ADOS) | 0.028 | 0.111 | −0.194/0.250 | 0.249 | .804 |
| Adaptive skills (ABA-II) | −0.025 | 0.019 | −0.060/0.013 | −1.282 | .204 |
| Parental psychological distress (K-10) | 0.078 | 0.038 | 0.002/0.154 | 2.056 | .044* |
CI, confidence interval. *P < .05; **P < .01; ***P < .001.
Model 1: adjusted R2 = 0.246.
Model 2: adjusted R2 = 0.173.
Table 2 focuses on the behavioural problems, and shows that model 1, in which perceived parental stress (APSI) was the independent variable, detected a significant association. In this model, the only significant covariate was the severity of core autism symptoms measured by means of the ADOS-2 (P < .001), or, in other words, the model detected a significant association between the severity of autism and behavioural problems in children with ASD. Model 2, in which the independent variable was parental psychological distress, detected a significant association with the behavioural problems dependent variable (P < .001). We also found a significant association between the severity of autism and parental educational attainment.
Table 3 presents the results of the model in which the dependent variable was the presence of emotional problems in children with ASD during early childhood. Model 1 found a significant association with the stress perceived by parents (P < .01). It also evinced a significant positive association with age, that is, as age increased, so did the emotional problems in these children. Based on model 2, there is also a significant association between psychological distress in parents and emotional problems in the children (P < .05) after controlling for the rest of the covariates that were not significant in explaining the variance in the model.
DiscussionThe results of the study supported the initial hypothesis that there is an association between parental stress and distress and emotional and behavioural problems in children with ASD from early childhood, even after controlling for variations shared by childrens´ severity of autism and adaptive functioning, and sociodemographic characteristics such as parental educational attainment and age and sex of the child.
Our findings are consistent with those of Goodman et al.37 and the latest meta-analysis by Yorke et al.,25 which found evidence that high levels of parental psychological distress are associated with both emotional problems (internalizing disorders) and behavioural problems (externalizing disorders). In addition, there is evidence that externalizing disorders in children have a stronger impact on parental stress during early childhood, while internalizing disorders tend to have a stronger impact on parental stress during late childhood and early adolescence.25 This is consistent with our findings, as we found a positive association between the age of the child and the presence of emotional problems from early childhood, in addition to a stronger association with behavioural problems.
Our study also took into account differences in cognitive and adaptive skills between children with ASD, which have been frequently reported to be associated with various behavioural and emotional disorders.38 That is, the association with perceived stress and symptoms of anxiety or depression (psychological distress) in parents continues to be significant independently after controlling for both adaptive functioning and the severity of autistic symptoms. However, we did not find a significant association between adaptive skills and emotional and behavioural problems in the regression models.
Although there is evidence that symptoms of autism and behavioural problems improve somewhat over time,39 autism is a disorder with no known cure that brings multiple challenges to families in each stage of life. These daily stressful experiences can have a negative impact on the wellbeing of parents, and some studies evince that parents of children with ASD experience high levels of caregiver stress.40 The behavioural problems frequently found in children with ASD are among the most significant sources of stress to their families22 and could explain the observed direct association found in our study, which was also described in the most recent meta-analysis on the subject.25
Also in agreement, the model published by Hastings22 indicates that emotional and behavioural problems in children with ASD increase parental stress, which in turn compromises the ability of the parent to engage in positive parenting behaviours that could support the development of emotional and behavioural skills in the child. Thus, there may be a feedback loop by which each of these variables reinforces the other, so that parental stress/distress would have a negative impact on emotional functioning and behaviour in the children, and these features in the children would exacerbate the stress and distress of parents.
One of the strengths of our study was the careful recruitment of children aged less than 6 years and a high participation rate of more than 80%, as recruitment of very young children often proves challenging. In addition, we evaluated every child with the gold standard of diagnosis, the ADOS-2, in addition to the clinical diagnosis of ASD. Lastly, there are few studies focused on early childhood (<6 years) in the literature. Thus, in the most recent systematic review, published by Yorke et al. in 2018, of the 67 studies included in the review, only 9 focused on young children aged less than 6 years.
In our study, emotional and behavioural problems in children were reported by parents, who also rated their own stress and mental health problems, and therefore the data in different questionnaires completed by the same individual may show an association for reasons other than a true association between the variables of interest; it is possible that parents that experienced greater psychological distress perceived certain behaviours of the child as being more problematic compared to other parents.41 Secondly, our reliance on a single source of information on the emotional and behavioural problem of children (mainly the mothers) may limit the generalizability of the observed association of these problems with parental distress to certain conditions. Thus, while our study contributes data supporting an association between parental stress/distress and emotional and behavioural problems in children with ASD, due to its cross-sectional design, we were unable to establish causality or direction of effect.
Relevance and future lines of researchThis study not only adds to the existing evidence on ASD and its comorbidities, but it is quite relevant at the clinical level. First of all, there is little data on the role of families in the population with ASD. It is clear that the aetiology of autism has a strong genetic component, and this may have contributed to the lack of research on environmental aspects in the home. The negative impact of the now discredited “refrigerator mother” theory of the aetiology of autism may also partly explain the dearth of research on this area.42 However, the influence of families and parents is considered an important element in the development and outcomes of psychiatric disorders in children with normal development.9 Therefore, the aim of our study was to clarify the potential impact of the home environment in the mental health of the population with ASD, focusing on parental stress and psychological distress, and to explore future lines of research.
Another important aspect to explore in future research is whether the association found between parental stress/distress and mental health problems in children with ASD is moderated by other family characteristics, such as structure and cohesion. For instance, Mink and Nihira43 found that in cohesive families, the family tended to influence the child, whereas in control-oriented families, the child tended to influence the family.
It may also be beneficial to explore other concurrent mental health problems in children with ASD, such as hyperactivity, obsessive patterns and emotional dysregulation, and their association with parental stress and distress.
As our findings suggest, one of the possible ways to address behavioural and emotional comorbidities in children with ASD is to treat stress/psychological distress in the parents. In other mental health disorders, psychoeducation and group therapy programmes for parents have been found to offer significant benefits in terms of symptom reduction in children. Examples include programmes aimed at improving the parent-child relationship, such as Incredible Years,44 or programmes with mindfulness and acceptance components within an evidence-based treatment plan for children and adolescents.45
In short, despite the aforementioned limitations, our study contributes evidence on ASD and its comorbidities and on parental psychological distress/stress. Our study also lays the foundation for future studies exploring the association between parental factors and emotional and behavioural problems in children with a diagnosis of ASD. It also suggests that parental stress and distress in parents of children with ASD could be a target of intervention from early childhood in the framework of a comprehensive strategy of interventions and treatments aimed at improving emotional and behavioural outcomes in these children.
Conflicts of interestThe principal investigator declares no conflicts of interest, and thanks the Fundación Alicia Koplowitz for the support given in the form of a returning scientist grant, which allowed the initiation of this project. The author also thanks families for their participation. Without them, advances in science would not be possible.
Please cite this article as: Romero-González M, Marín E, Guzmán-Parra J, et al. Relación entre estrés y malestar psicológico de los padres y problemas emocionales y conductuales en niños preescolares con trastorno del espectro autista. An Pediatr (Barc). 2021;94:99–106.