Proctalgia consists of pain in the anal region of varied aetiology. The most frequent causes are anal fissure, pudendal neuralgia, levator ani syndrome, coccygodynia, proctalgia fugax, hypertrophy of the internal anal sphincter, visceral hypersensitivity, anxiety and anorectal dyssynergia.1,2 In children, the pain is intermittent and transient and usually responds to customary management, such as sitz baths or topical remedies, although in some cases it requires more specific and invasive treatments.3–6
We present the case of a boy aged 8 years with no relevant history who visited the paediatric gastroenterology outpatient clinic for evaluation of anal pain of several weeks’ duration.
The patient reported episodes of intense anal pain (rated 10 on a 10-point scale) that occurred intermittently (sometimes daily for a whole week), prolonged (lasting several hours) and utterly disabling, with a significant deleterious impact on his quality of life. They were not associated with any trigger and occurred even with the patient at rest. For 5 years, the pain episodes persisted despite multiple treatments, such as warm sitz baths, inhaled salbutamol, topical nitroglycerine, topical diltiazem, topical steroids, oral lorazepam, oral and intravenous metamizole, oral mebendazole, oral cyproheptadine, oral oxcarbazepine oral, psychotherapy and pelvic floor rehabilitation (electrical stimulation of posterior tibial nerve, biofeedback and radiofrequency stimulation of the anal canal). Pudendal nerve block, with CT-guided injection of medication, achieved temporary improvement, but the pain eventually recurred. The parents refused injection of botulinum toxin.
The general results of the laboratory and imaging tests were absence of inflammation based on serum levels of inflammatory markers, and absence of abnormal features in the rectosigmoidoscopy, anal ultrasound and magnetic resonance imaging. The anorectal manometry evinced considerable elevation of anal pressure with a normal recto-anal inhibitory reflex.
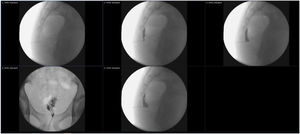
Given the persistence of the problem and its impact on everyday quality of life, combined with the lack of response to multiple treatments, the patient was referred to the pain unit of the department of anaesthesia, where he underwent bilateral pulse radiofrequency of the ganglion impar (ganglion of Walther) at age 14 years (Fig. 1). The treatment was delivered in 2 sessions, one guided by ultrasound and the other one by fluoroscopy, with the following settings: 42 °C, 6 min, 0.5 V + injection of 0.5% bupivacaine and triamcinolone. Following the sessions, the patient experienced transient pain, with no subsequent side effects, and the proctalgia improved gradually until its full resolution. Currently, at 2 years post treatment, the patient remains completely asymptomatic and has not experienced any recurrences. If the pain were to recur, he would be treated with additional pulsed radiofrequency sessions.
In conclusion, anal pain can be long-lasting and disabling in some children, seriously affecting quality of life. In cases refractory to conventional treatment, pulsed radiofrequency of the ganglion impar should be considered, as it is safe and effective.
Previous meeting: This case was presented as a poster communication at the XXVIII Congress of the Sociedad Española de Gastroenterología, Hepatología y Nutrición Pediátrica, June 2022.