Trauma care in Spain is not provided in specific centres, which means that health professionals have limited contact to trauma patients. After the setting up of a training programme in paediatric trauma, the aim of this study was to evaluate the quality of the initial care provided to these patients before they were admitted to the paediatric intensive care unit (PICU) of a third level hospital (trauma centre), as an indirect measurement of the increase in the number of health professionals trained in trauma.
Materials and methodsTwo cohorts of PICU admissions were reviewed, the first one during the four years immediately before the training courses started (Group 1, period 2001–2004), and the second one during the 4 years (Group 2, period 2012–2015) after nearly 500 professionals were trained. A record was made of the injury mechanism, attending professional, Glasgow coma score (GCS), and paediatric trauma score (PTS). Initial care quality was assessed using five indicators: use of cervical collar, vascular access, orotracheal intubation if GCS≤8, gastric decompression if PTS≤8, and number of actions carried out from the initial four recommended (neck control, provide oxygen, get vascular access, provide IV fluids). Compliance was compared between the 2 periods. A p<0.05 was considered statistically significant.
ResultsA total of 218 patient records were analysed, 105 in Group 1, and 113 in Group 2. The groups showed differences both in injury mechanism and in initial care team. A shift in injury mechanism pattern was observed, with a decrease in car accidents (28% vs 6%; p<0.0001). Patients attended to in low complexity hospitals increased from 29.4% to 51.9% (p=0.008), and their severity decreased when assessed using the GCS≤8 (29.8% vs 13.5%; p=0.004), or PTS≤8 (48.5% vs 29.7%; p=0.005). As regards quality indicators, only the use of neck collar improved its compliance (17.3–32.7%; p=0.01). Patients who received no action in the initial care remained unchanged (19% vs 11%%; p=0.15).
ConclusionsAlthough there are limited improvements, the setting up of a training programme has not translated into better initial care for trauma patients in our area of influence. Trauma training should be complemented with other support measures in order to achieve a systematic application of the trauma care principles.
En nuestro país la asistencia al trauma no se presta en centros específicos, lo que expone a los profesionales sanitarios a un contacto esporádico con este tipo de pacientes. El objetivo de este estudio es evaluar la calidad de la asistencia inicial prestada a los pacientes antes de su ingreso en la Unidad de Cuidados Intensivos Pediátricos (UCIP) de un centro de tercer nivel tras el inicio de un programa formativo en trauma pediátrico, como medida indirecta del aumento de profesionales con formación específica.
Material y métodosSe seleccionaron 2 cohortes de pacientes correspondientes a los ingresos en UCIP por trauma durante los 4 años previos al inicio de los cursos de formación (grupo 1, periodo 2001–2004) y durante los 4 últimos años (grupo 2, periodo 2012–2015), tras haber formado a cerca de 500 profesionales. Se registró el mecanismo lesional, equipo que presta la asistencia inicial, puntuación en el score de Glasgow (GCS) en la atención inicial, y puntuación en el índice de trauma pediátrico (ITP) en la atención inicial. La calidad de la asistencia se evaluó mediante 5 indicadores: uso de collarín cervical, obtención de una vía venosa, intubación orotraqueal si GCS≤8, sondaje gástrico si ITP≤8, y número de actuaciones realizadas entre las primeras 4 medidas recomendadas (control cervical, administración de oxígeno, canalización de vía periférica y administración de fluidos). Se comparó el porcentaje de cumplimiento de los indicadores en ambos periodos. Una p<0,05 fue considerada estadísticamente significativa.
ResultadosSe analizó a 218 pacientes; 105 en el grupo 1 y 113 en el grupo 2. Los grupos mostraron diferencias tanto en el mecanismo lesional como en el equipo que presta la asistencia inicial. En los últimos años se aprecia una disminución de los accidentes de tráfico (28% vs. 6%; p: 0,0001), así como un aumento de los casos atendidos en centros de baja complejidad (29,4% vs. 51,9%; p: 0,008). También disminuyeron los pacientes en coma (29,8% vs. 13,5%; p: 0,004) o con trauma grave (48,5% vs. 29,7%; p: 0,005). De los indicadores analizados solo se observó mejoría en el uso de collarín cervical (17,3% vs. 32,7%; p: 0,01), sin modificarse el porcentaje de pacientes en los que no se realiza ninguna acción en la asistencia inicial (19% vs. 11%; p: 0,15).
ConclusionesAunque con mejoras aisladas, el desarrollo de un programa formativo específico no se ha traducido en una mejora global de la calidad asistencial en este tipo de pacientes. La formación en trauma debe complementarse con medidas de refuerzo para conseguir una aplicación sistemática del algoritmo de actuación.
Injury is the leading cause of death for children over a year of age in developed countries. More than 8.7 million children are treated in emergency departments for injury each year, with more than 7000 deaths a year, and improving injury care is a public health priority.1 Spain does not have a national injury register, although there is one at the European level (The European Injury Database).2 In the absence of official data, save for the death records offered by the Instituto Nacional de Estadística (National Institute of Statistics), 2 studies conducted in different paediatric hospitals have offered an equally worrisome approximation, estimating that for every death there are 160 hospital admissions and 2600 visits to emergency departments.3–5
Spain does not have specific referral centres for paediatric trauma care, so these patients are usually managed at the scene of the accident by the advance life support (ALS) ambulance teams, or at the nearest hospital or primary care centre, which exposes health professionals in these facilities to patients with life-threatening conditions with whom they rarely come into contact. Adding to this low incidence, the care provided in the first few minutes has an impact on the final outcome in what has come to be known as the “golden hour”, so that appropriate medical intervention is of vital importance. The Advanced Trauma Life Support (ATLS) protocol is the gold standard for the management of trauma patients since it was first adopted in the 1980s by the American College of Surgeons as a training programme for trauma care.6 This protocol offers an intervention algorithm that is similar to that of paediatric CPR (ABCDE for trauma) and standardises the actions to be taken in the first moments of care.
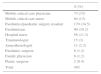
The paediatric version of this course was introduced in Spain in 1987 by the Sociedad Española de Cirugía Pediátrica (Spanish Society of Paediatric Surgery) in the form of the AITP course (atención inicial al trauma pediátrico, or initial care for paediatric trauma), which reproduces the standardised training of the ATLS, adapting it to the paediatric population.7 The course consists of a distance portion and a face-to-face portion in which students engage in various skill stations in a simulation environment and take a final test with actors in character. This course has been taught in our hospital since 2004, and more than 500 professionals have been trained to date, physicians as well as nurses, employed in both hospital and out-of-hospital settings (Table 1). The aim of this study was to assess the quality of the initial care provided to patients brought to a tertiary care level hospital as an indirect measure of the increase in the number of professionals trained in trauma care.
Distribution of students by specialty (March 2004–March 2016).
| N (%) | |
|---|---|
| Mobile critical care physician | 73 (15) |
| Mobile critical care nurse | 64 (13) |
| Paediatrics/paediatric surgery resident | 170 (34.5) |
| Paediatrician | 90 (18.2) |
| Hospital nurse | 56 (11.3) |
| Traumatologist | 15 (3) |
| Anaesthesiologist | 11 (2.2) |
| Paediatric surgeon | 6 (1.2) |
| Family physician | 6 (1.2) |
| Plastic surgeon | 2 (0.4) |
| Total | 493 |
We conducted a retrospective study of patients admitted to the paediatric intensive care unit (PICU) with traumatic injuries. We selected 2 historic cohorts that corresponded to a first period comprehending the 4 years preceding the implementation of the training courses (2001–2004, group 1) and a second period that included the last 4 years of activity (2012–2015, group 2). The AITP course is open to all health professionals and is offered twice a year in classes of 25 students each (originally 20). It includes a distance education portion in which students are given a manual with the theoretical contents, and a face-to-face portion delivered over two days. The face-to-face portion includes a brief review of the theory as well as training at the different skill stations, which cover the full range of interventions and decisions involved in the care of these patients: basic and advanced airway management, peripheral catheter placement, treatment of immediately life-threatening injuries in anaesthetised experimental animals (tension pneumothorax, massive haemothorax, cardiac tamponade), cervical collar placement and immobilisation of patient for transport, extrication, interpretation of radiologic tests and patient classification and triage. In addition to individual training, performance as part of a team is evaluated by practicing scenarios of accidents with multiple victims. The course ends with a theoretical exam and a practical exam with actors (children in character) in which the student has to demonstrate the acquired skills by managing a variety of clinical scenarios.
In addition to demographic characteristics, the variables under study included the mechanism of injury, the team that provided initial care, the Glasgow Coma Score (GCS) at the time of initial care and the paediatric trauma score (PTS).
To assess the quality of initial trauma care, we evaluated 4 clinical indicators that are commonly used in studies of this type8,9 and that reflect the adherence to interventions considered indispensable in trauma care: use of a cervical collar, establishment of vascular access, orotracheal intubation in patients with a GCS of 8 or less, and placement of a gastric tube in patients with severe trauma (PTS≤8). We also included a fifth indicator that counted the number of interventions performed out of the first 4 recommended interventions: cervical immobilisation, oxygen administration, peripheral catheter placement and administration of intravenous fluids.
We collected the data from emergency department discharge summaries for patients managed in hospitals, or from the patient care reports that must be completed by ALS ambulance teams documenting the performed interventions.
To analyse the data, we compared categorical variables by means of the chi-square test or the Fisher exact test. We compared continuous variables using the Student t test or the Mann–Whitney U test based on whether the variable followed a normal distribution. We set the level of significance at the conventional p-value of less than 0.05 to define statistical significance.
ResultsThe study sample consisted of 218 patients: 105 patients in group 1 (2001–2004 period) and 113 in group 2 (2012–2015 period). The number of admissions to the PICU due to severe trauma remained stable through both periods, with a mean of 26 admissions a year and a range of 20–32 admissions.
The comparison of both groups revealed a similar distribution by sex and age, with the characteristic predominance of the male sex in trauma patients (Table 2). The groups were not comparable in terms of the mechanisms of injury, trauma care team or proportion of severely injured patients. In recent years, there has been a decrease in the number of patients injured in road accidents while riding a vehicle and an increase in unintentional falls and bicycle accidents, as well as a decrease in the number of cases managed by mobile ALS teams and an increase in the cases treated in lower-level health care facilities. We also found a decreased frequency of patients in a coma (GCS≤8) or with severe trauma (PTS≤8), which was probably related to the decreased incidence of high-energy injuries.
Characteristics of the study sample.
| Group 1 N=105 n (%) | Group 2 N=113 n (%) | p | |
|---|---|---|---|
| Sex | |||
| Male | 68 (64.8) | 75 (66.4) | 0.80 |
| Female | 37 (35.2) | 38 (33.6) | |
| Mechanism of injury | |||
| Unintentional fall | 19 (18) | 44 (39) | 0.0001 |
| Fall from height | 22 (21) | 11 (10) | |
| Motor vehicle (rider) | 30 (28.6) | 7 (6.4) | |
| Motor vehicle (pedestrian) | 19 (18) | 17 (15.5) | |
| Bicycle | 8 (7.6) | 13 (11.8) | |
| Crushing | 4 (3.8) | 8 (7.3) | |
| Direct hit | 2 (1.9) | 6 (5.5) | |
| Other | 1 (1) | 4 (3.6) | |
| Care team | |||
| Trauma centre. Emergency department | 14 (13.7) | 8 (7.4) | 0.008 |
| Trauma centre. PICU | 3 (2.9) | 0 | |
| Other hospital | 30 (29.4) | 56 (51.9) | |
| Primary Care Centre | 5 (4.9) | 2 (1.9) | |
| Intensive Care ambulance | 49 (48) | 39 (36) | |
| Basic Life Support (BLS). Ambulance without medical staff (nurse or physician) | 1 (1) | 3 (2.8) | |
| Severity | |||
| Patients with GCS≤8 | 31 (29.8) | 15 (13.5) | 0.004 |
| Patients with PTS<8 | 50 (48.5) | 33 (29.7) | 0.005 |
| Mean (SD) | |||
|---|---|---|---|
| Age (years) | 7.2 (4.3) | 6.6 (4.3) | 0.3 |
| Glasgow Coma Score | 11.5 (4.2) | 13.08 (3.4) | 0.006 |
| Paediatric Trauma Score | 7.9 (3.1) | 9.3 (3.1) | 0.002 |
When it came to the quality of care, while the percentage of adherence to the quality indicators increased in nearly all (Table 3), the difference was only statistically significant in the use of measures for cervical spine control (p=0.01), with a near-significant p-value for the establishment of peripheral vascular access (p=0.054). The indicator with the least improvement was the use of gastric tubes for decompression (p=0.14), although its proportion had doubled in group 2 (from 12% to 24%).
Initial care quality indicators.
| Variable | Period 1 | Period 2 | p |
|---|---|---|---|
| n (%) | |||
| Peripheral catheter placement | 78 (75) | 94 (85.5) | 0.054 |
| Use of cervical collar | 18 (17.3) | 35 (32.7) | 0.01 |
| Orotracheal intubation (OTI) if GCS≤8 | 17 (54.8) | 12 (80) | 0.09 |
| Gastric intubation in case of severe trauma (PTS≤8) | 6 (12) | 8 (24.2) | 0.14 |
| Number of initial interventions from the following | |||
| Cervical spine control | |||
| Oxygen administration | |||
| Peripheral vascular catheter placement | |||
| Administration of IV fluids | |||
| 0 | 20 (19.8) | 11 (11.3) | 0.15 |
| 1 | 9 (8.9) | 13 (13.4) | |
| 2 | 34 (33.7) | 32 (33) | |
| 3 | 27 (26.7) | 21 (21.7) | |
| 4 | 11 (10.9) | 20 (20.6) | |
We also found no statistically significant differences in the “number of initial interventions” indicator, with a similar proportion of patients in who no intervention was performed during initial care (19% in group 1, 11% in group 2). This variable exhibited a statistically significant negative correlation with both the GCS (r=−0.40; p=0.0001) and the PTS (r=−0.357; p=0.0001), so that the more the number of interventions decreased, the better the mental status of the patient or the lesser the apparent severity. We only calculated this indicator in patients for who enough information was available on the 4 interventions under study, and therefore it was the indicator that was most affected by missing data. In group 1, we calculated it based on 101 cases (96% of the sample), whereas in group 2 we calculated it based on 97 cases (85% of the sample). An additional analysis that presupposed that the appropriate interventions had been performed in cases with missing data (worst case analysis) gave similar results, with maintenance of the inverse correlation of the GCS and the PTS with the number of performed interventions (r=−0.41; p=0.01 for GCS; r=−0.34; p=0.01 for PTS).
Most patients in who the initial care interventions were not performed presented with traumatic brain injury (TBI) associated with skull fracture and complicated by bleeding (subdural or epidural haematoma, intracerebral or subarachnoid haemorrhage).
DiscussionIt is well known that simulation-based training programmes are a very useful tool for the development of skills and habits that would be difficult to achieve in health problems with a low prevalence and a high mortality,10 as is the case of traumatic injury. Our data revealed that in recent years, most of these patients were managed in hospitals with a low level of care, possibly as a result of the decrease in traffic accidents, which means that any professional serving the paediatric population could face such a case. There are few data on the impact of training courses in clinical practice. Evaluations conducted in simulation environments9,11 tend to show an improvement of parameters in post-training evaluations compared to pre-training, but it would not be realistic to expect the same degree of improvement in a real-world environment. Two previous studies have investigated the correlation between training and real practice in Spain, one in the paediatric population conducted in the Hospital Gregorio Marañón,7 and another in adults conducted in several hospitals in Catalonia (TRAUMACAT project).8 The study on the paediatric population focused exclusively in the care provided by mobile ALS teams, and found improvement in every indicator, which probably reflected the greater specialisation of these teams in the care of these patients. The study on the adult population assessed performance in emergency department bays, although 75% of the sample had been transported and therefore received initial care from ALS ambulance teams, and the study was limited to victims of high-energy accidents.
When it comes to the indicators used for quality assessment, several authors have remarked on the difficulty of establishing global standards for data auditing.12 Mortality is not considered an appropriate indicator, as many injuries carry a low risk of death yet a high risk of disability, leading to the proposal of other indicators, such as the presence of shock, sepsis, ventilator-associated pneumonia or undue delays in care,13 although these indicators also assess the quality of in-hospital and not only of out-of-hospital care. The indicators we used for out-of-hospital care in our study were based on the interventions proposed by the AITP management algorithm, although other protocols may be implemented based on the age of the patient or different training programmes. Thus, the protocol established by the Cincinnati Children's Hospital, designed for groups (teams), takes into account variables such as the time elapsed to initiation of electrocardiographic monitoring, and the ATLS, geared towards the adult population, assesses the presence of a heart rate of less than 100bpm as an indicator of haemodynamic stability prior to transfer to radiology, a situation that cannot be extrapolated to the paediatric population.
In our series, gastric tube placement in severely injured patients was the indicator in which there was the least improvement, possibly because it is perceived as an aggressive intervention in paediatric patients, especially in the absence of changes in the level of consciousness, a circumstance that has already been identified in similar studies.14 As for the “number of interventions performed,” the fact that it is negatively correlated to signs of neurologic involvement is important, as it denotes an erroneous perception of risk in these patients. The implementation of the trauma algorithm should not be based on the Glasgow Coma Score, but on the medical history of the patient. It is important to remember that while a low GCS is a risk factor for the presence of intra-abdominal injury, a high score does not rule it out, or that paediatric patients can continue to be haemodynamically stable for hours despite rupture of a solid organ. No intervention or a single intervention was performed in 30% of patients in group 1 and 25% of patients in group 2 during initial care. A more detailed analysis of the diagnoses of these patients at the time of admission to the PICU revealed a predominance of TBI associated with skull fracture and complicated by haemorrhage (subdural or epidural haematoma, subarachnoid haemorrhage), but there were also patients with solid organ rupture or multiple fractures, including pelvic fracture. Therefore, the best possible care is to adhere to the trauma care protocol until performance of diagnostic tests is completed and the patient can be classified appropriately.
The availability of a simulation training programme in a given region does not imply that the quality of pre-hospital care is any better compared to other areas,15 and furthermore, a direct association between the care provided by professionals trained in trauma management and improved outcomes has not been established to date,16 mainly due to a lack of rigorous studies. Nevertheless, training by means of simulation has been proven to increase individual confidence and skills in the management of complex medical situations. Although it has been estimated that students of these courses retain their knowledge for a period of 6 years,17 it is probably unrealistic to depend solely on such courses to achieve an overall improvement in outcomes. Complementary strategies, such as the one developed in the TRAUMACAT programme, which combines educational talks with the distribution of informational posters in the emergency care area, or the use of a checklist in the care of trauma patients,18 may contribute to reduce the number of tasks that are not performed during initial care.
Last of all, we ought to note some of the limitations of the study associated with its retrospective design. First of all, we were unable to establish a direct association between training courses and the analysed data, as it was not possible to determine whether the health professional (or professionals) that delivered care had been trained in trauma management, and only 50% of our students were employed in the catchment area of the hospital. Considering that our hospital is the only hospital in the province with a trauma centre, it is reasonable to assume that the data we collected was appropriate for the assessment of the level of training in our region.
Secondly, there was a patient selection bias, as we only analysed data for patients admitted to the PICU, excluding the rest of hospitalised patients that stayed in the ward. The sample we used has characteristics that are common in trauma care studies, and the inclusion of patients admitted to hospital but that did not need admission to PICU would have been a source of bias of a different kind, as we would have only analysed patients admitted to our hospital, excluding those admitted to lower-level facilities, which would diminish the external validity of the results.
Lastly, we should highlight that the two groups were not comparable, so the univariate analysis may have been affected by intervening variables, as well as by the small sample size for some of the study variables when we restricted the analysis to subgroups of patients with a GCS or PTS of 8 or less. We cannot exclude the possibility that the size of the compared groups was responsible for results not being statistically significant despite the absolute increase in the percentage of adherence to 4 out of the 5 analysed indicators.
In conclusion, our results show an increased proportion of trauma cases managed in non-specialty hospitals along with a decrease in trauma severity. The implementation of AITP training courses has not translated to an overall improvement in quality indicators for the care of patients managed at a tertiary care hospital, with the exception of specific interventions, such as the use of a cervical collar. Training courses should be combined with other resources, such as the dissemination of outcomes, the use of checklists or other reinforcing measures to achieve the systematic implementation of currently recommended protocols.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank the AITP-Valencia group.
Please cite this article as: Ibáñez Pradas V, Pérez Montejano R. Calidad asistencial en la atención inicial al trauma pediátrico. An Pediatr (Barc). 2017;87:337–342.
Previous presentation: This study was presented at the Jornada Conmemorativa of the XXV Curso de AITP-Valencia: Avanzando en la formación del politrauma pediátrico. March 3, 2016; Valencia, Spain.