A female term neonate was admitted 2 days post birth with unconjugated hyperbilirubinemia (peak total bilirubin, 25.06 mg/dL; direct bilirubin, 1.49 mg/dL) that was found to be recurrent. She was treated with 5 phototherapy sessions and 2 blood transfusions, and remained haemodynamically stable.
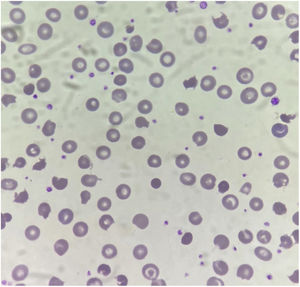
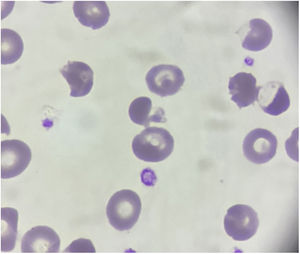
The complete blood count revealed a white blood cell count of 16,200 cells/μL, a haemoglobin concentration of 6.7 g/dL, a mean corpuscular volume of 103.6 fL, a reticulocyte count 7.5%, platelet count 605,000/μL and LDH 371 U/L. Leishman staining of the peripheral blood smear (PBS) revealed spiculated, irregularly contracted cells, pyknocytes, blister cells, polychromasia, target cells and rare spherocytes (Figs. 1 and 2).
On physical examination the patient was icteric, but with no other alterations, mainly hepatosplenomegaly.
The differential diagnosis of neonatal haemolytic anaemia included testing for membranopathies, enzyme deficiencies, thalassaemias, infections, autoantigen incompatibility and an abdominal ultrasound scan, the results of which were normal.1 The direct Coombs test and irregular antibody screening were negative, with no evidence of blood type incompatibility. Haematological tests in the mother were negative.
These findings confirmed the diagnosis of infantile pyknocytosis. The haemolysis resolved on day 20 and the patient was discharged from hospital.
She underwent evaluations at 1 and 2 months post discharge, which evinced absence of jaundice, good weight gain and neurodevelopment, progressive improvement of anaemia and normal PBS morphology with no pyknocytes. She remains on otorhinolaryngological follow-up, without hearing changes.
Infantile pyknocytosis is a benign transient rare condition responsible for 10% of cases of neonatal haemolytic anaemia of unknown aetiology. The diagnosis is made through the identification of pyknocytes in the PBS. It usually resolves spontaneously within 4–6 months and does not recur.2,3
The differential diagnosis of haemolytic jaundice in newborns should include infantile pyknocytosis, especially in cases without splenomegaly or without a history of infection and after ruling out the common known causes, for which performance of a PBS is essential in all newborns with haemolytic anaemia to allow timely and appropriate diagnosis and treatment.
We thank the family of the newborn and all the members of the health care team for their help and support.