Hyper-attendance is a significant problem in paediatric primary care clinics. The aim of our study was to analyse the level of attendance in these clinics and its relationship with certain psychosocial aspects of the families attending them.
Patients and methodsObservational descriptive study was conducted using questionnaires collected during a period of 6months, as well as recording the frequency of attendance in the previous 6months. A total of 346 questionnaires of children between 6months and 13years of age belonging to 2 urban primary care clinics in Madrid were completed. The raw data was analysed, and comparisons between groups and multivariate analysis were performed.
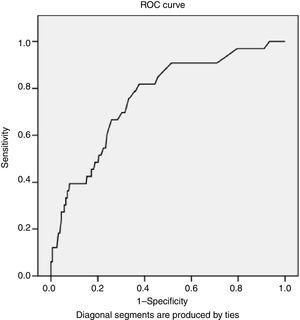
ResultsThe mean number of consultations in the last 6months, of the total included in the study, was 3.06 in the primary care centre, and 0.77 in the emergency services. It was considered over-frequent for those who had attended the primary care health centre 6 or more times in this period (>P90), of which there were 33 children (9.53%). In the multivariate analysis, the variables related to being frequent users of primary care clinics were: the presence of high level of anxiety in the parents (OR=5.50; 95%CI: 2.49–12.17, P<.0001), and the age of the children (OR=0.73; 95%CI: 0.58–0.91, P=.005). The model presented an area under the curve of 0.761 (95%CI: 0.678–0.945, P<.0001).
ConclusionsThe frequency of visits in paediatric primary care clinics is directly related to the high level of anxiety of the parents, and inversely to the age of the children. It would be advisable to detect and, if possible, intervene in cases of high parental anxiety in order to try to reduce the over-frequency in the paediatric primary health care.
La hiperfrecuentación es un problema relevante en las consultas pediátricas de atención primaria, por lo que el objetivo de nuestro estudio ha sido analizar el nivel de frecuentación en dichas consultas y su relación con determinados aspectos psicosociales de las familias asignadas a las mismas.
Pacientes y métodosEstudio descriptivo observacional realizado mediante cuestionarios recogidos durante un periodo de 6meses y registrando la frecuentación de los 6meses previos. Se han completado 346 encuestas de niños entre 6meses y 13años de edad pertenecientes a dos consultas urbanas de atención primaria de Madrid. Se analizaron datos crudos, comparaciones entre grupos y análisis multivariante.
ResultadosEl promedio de consultas en los últimos 6meses, del total de incluidos en el estudio, fue de 3,06 en el centro de salud y de 0,77 consultas en urgencias. Se consideró hiperfrecuentadores a los que habían acudido 6 o más veces al centro de salud en este periodo (>p90), que fueron 33 niños (9,53%). En el análisis multivariante, las variables relacionadas con ser hiperfrecuentador en las consultas del centro de salud fueron la presencia de elevado nivel de ansiedad en los padres (OR=5,50; IC95%: 2,49-12,17; p<0,0001) y la edad de los niños (OR=0,73; IC95%: 0,58-0,91; p=0,005). El modelo presentó un área bajo la curva de 0,761 (IC95%: 0,678-0,945; p<0,0001).
ConclusionesLa frecuentación en las consultas pediátricas de atención primaria está directamente relacionada con el nivel elevado de ansiedad de los padres e inversamente con la edad de los niños. Sería recomendable detectar y a ser posible intervenir en los casos de elevada ansiedad parental para así intentar reducir la hiperfrecuentación asistencial.
In Spain, universal coverage for paediatric health care is guaranteed by law. The Public Health System has the duty to deliver quality care regardless of the administrative situation of a child.1–5
The Public Health System is funded through taxation, and it is the citizens, through their tax contributions, that maintain the system. Receiving care on demand as often as the patient wants by presenting the health care card obtained after registering in the census has an economic cost that health care users are often unaware of.
The quality of paediatric health care6 improves significantly by enhancing primary care (PC) services, increasing the number of paediatricians, expanding service hours from 8 am to 9 pm and including patients through age 14 years. These measures clearly improve accessibility and have been very well received by the population, as when it comes to children, there is generally a rushed, heedless and indulgent attitude towards the use of health care services.7 On the other hand, health care providers have described the emergence of a phenomenon known as high-frequency utilisation,8 a concept that is difficult to define because there is no clearly established threshold based on the number of visits a patient would have to make in a given time period.9 Providers that deliver PC, hospital emergency care and after-hours outpatient urgent care frequently experience stress because the frequent visits of some patients do not seem to be warranted by the clinical situation; furthermore, and considering that this excess entails the unnecessary use of resources, it stands to reason that all the involved agents should act and share the responsibility of regulating the disorganised flows of patients.10
The aim of our study was to analyse the frequency of utilisation of paediatric PC services and the factors that could be associated with specific psychosocial aspects in the families included in the caseloads of participating clinics.
Patients and methodsWe conducted an observational descriptive study by analysing the data collected through the administration of a questionnaire to the parents of 346 children aged 6 months to 14 years that visited 2 paediatric clinics in 2 urban PC centres in the Community of Madrid. We had previously validated the questionnaire in a pilot study (reliability assessed by Cronbach α [0.768; P<.0001] and validity by confirmatory factor analysis and the item-test correlation coefficient). The total number of children in this age group with health care cards assigned to the caseloads of these two clinics was approximately 2800, and we requested the participation in the survey between March and August of 2017 of a randomly selected sample of the children in this group that visited the clinic with or without having previously scheduled an appointment.
We collected data for the following variables: age and sex of the patients, age and country of origin of parents, family structure (whether parents lived together or apart), parental educational attainment, household income, patient enrolment in child care facility or school, number of visits to the primary care centre, hospital emergency departments or after-hours urgent care clinics in the past 6 months; the parents were also assessed with the Goldberg Anxiety and Depression Scale (GADS), a tool used for screening anxiety and depression. The overall scale has a sensitivity of 83% and a specificity of 82%, it is administered by an interviewer, and the cut-off points are 4 points or higher for the anxiety subscale and 2 points or higher for the depression subscale. The scale was designed to detect probable cases rather than for diagnosis.11 We found the data regarding the number of visits by reviewing the patients’ electronic health records.
We established 3 categories for assessment of household income: (1) monthly income of less than 1000 euro; (2) monthly income between 1000 and 2000 euro, and (3) monthly income greater than 2000 euro. We also established 3 categories for assessment of parental educational attainment: (1) no education or elementary education (primary education); (2) secondary education (middle school, high school, vocational education), and (3) higher education (short- or long-course university degree).
The endpoints in our study were the number of visits made to the 2 primary care centres, hospital emergency departments and after-hours urgent clinics as well as the overall number of visits.
We performed the statistical analysis of the data with the SPSS® software version 15.0. We have summarised quantitative data as mean and standard deviation (SD) and the qualitative data as absolute frequencies and percentages, and calculated 95% confidence intervals (CIs). We used the Mann–Whitney U test to compare quantitative variables after verifying that they did not follow a normal distribution (Kolmogorov–Smirnov test). We compared qualitative variables by means of the chi square test. Statistical significance was defined as a P-value of less than 0.05. We performed logistic regression analysis starting with a model that included all candidate variables and removing them one by one until only those that were statistically significant remained.
ResultsWe collected data for 346 children with a mean age of 3.61 years (range, 6 months to 13 years; SD, 2.69), of who 174 (50.2%) were male. The mean maternal age was 34.82 years (SD, 5.88) and the mean paternal age 37.95 years (SD, 6.75). The mean number of children in the household was 1.66 (SD, 0.76), and in 217 cases (62.7%) the patient was the first child. In 37 cases (10.7%), the patient lived in a single-parent household, and in 187 families (54.04%) at least one of the parents had immigrant status. Of all respondents, 127 reported having support from their families (36.7%). When it came to income, 65 households (18.8%) were in the low-income group, 131 (37.9%) in the middle-income group and 150 (43.4%) in the high-income group.
As for educational attainment, 21 respondents (6.1%) had an elementary education, 108 (31.2%) a secondary education and 217 (62.7%) a higher education.
Children of immigrant parents were younger at the time of visiting the health care centre compared to children of Spanish nationals, with a mean age of 3.17 years (SD, 2.21) versus 3.98 years (SD, 2.99) (P=.032). We did not find any other significant differences between these two groups in any of the other outcomes.
The mean GADS scores were 1.43 in the anxiety subscale (SD, 2.72) and 0.55 in the depression subscale (SD, 1.75). There were 57 respondents (16.47%) with a score of 4 or higher in the anxiety subscale, and 29 respondents (8.38%) with a score of 2 or more in the depression subscale.
Table 1 presents the epidemiologic data for the sample under study.
Epidemiological characteristics of the sample.
| Patient age in years, mean (SD) | 3.61 (2.69) |
| Maternal age in years, mean (SD) | 34.82 (5.88) |
| Paternal age in years, mean (SD) | 37.95 (6.75) |
| Number of children, mean (SD) | 1.66 (0.76) |
| Single-parent household, n (%) | 37 (10.7) |
| Immigrant family, n (%) | 187 (54.04) |
| Income level, n (%) | |
| Low | 65 (18.8) |
| Middle | 131 (37.9) |
| High | 150 (43.4) |
| Educational attainment, n (%) | |
| Elementary | 21 (6.1) |
| Secondary | 108 (31.2) |
| Higher | 217 (62.7) |
| Goldberg anxiety depression scale score | |
| Anxiety subscale, mean (SD) | 1.43 (2.72) |
| Depression subscale, mean (SD) | 0.55 (1.75) |
| Score of 4 or more in the anxiety subscale of the GADS, n (%) | 57 (16.47) |
| Score of 2 or more in the depression subscale of the GADS, n (%) | 29 (8.28) |
| Visits made to primary care centre in the past 6 months, mean (SD) | 3.06 (2.57) |
| Urgent visits made in the past 6 months, mean (SD) | 0.77 (0.56) |
| High-frequency utilisers of primary care services, n (%) | 33 (9.53) |
| High-frequency utilisers of primary care + urgent/emergency care, n (%) | 55 (15.98) |
| Age of children born to immigrants at time of visit, mean (SD) | 3.98 (2.99) |
| Age of children born to native Spaniards at time of consultation, mean (SD) | 3.17 (2.21) |
SD, standard deviation.
The mean number of visits made in the past 6 months for the total sample was 3.06 (SD, 2.56), with a maximum of 20 visits.
Table 2 presents the Spearman correlation coefficients for the association of the number of visits to the PC centre, emergency/urgent care services and overall visits with the anxiety and depression subscale scores in the total sample under study. We did not find an association between the anxiety score and age (r=0.013; P=.803).
We defined high-frequency utilisers as patients whose number of visits exceeded the 90th percentile of the sample (P90), either to the PC centre (P90=5.7) or overall (PC centre+emergency/urgent care, P90=5.95). Analysing children aged less than 3 years separately, the P90 was 6 for visits to the PC centre and 6.03 for overall visits, so we ultimately defined high-frequency utilisers as those who made 6 or more visits in the period under study. We found a total of 33 high-frequency utilisers if we restricted the definition to PC services (9.53%), and 55 (15.89%) if we included visits to emergency or urgent care services.
The respondents that made 6 or more visits to the PC centre and 6 or more overall visits had a score of 4 or more in the GADS subscale in 20.58% of cases, while they amounted to 6.57% of respondents with a score of less than 4 in the GADS (P<.0001).
We performed a multivariate analysis (binary logistic regression; Table 3) to identify variables associated with making 6 or more health care visits in 6 months, and in the final model, the variables that remained significant were age, as a protective factor, and a score of 4 or higher in the GADS, as a risk factor. We plotted a receiver operating characteristic (ROC) curve with the results of the model (Fig. 1), and found an area under the curve (AUC) of 0.761 (95% CI, 0.678–0.945; P<.0001).
Researching health care overuse is challenging. This is a multifactorial problem12 that involves, on the one hand, institutional aspects of health care organisation, on the other, aspects related to health care providers13 (who in some cases, depending on whether they work at the PC or emergency care level, may contribute to the increased demand for their services), and, last of all, aspects concerning the patients themselves.14 In the paediatric population, the demand for care originates from the parents or caregivers of the child, and their perception of the child's health and the health education they have received determine whether they repeatedly seek services at the emergency care level. There is no consensus as to what constitutes a high-frequency utiliser, and we found different definitions in the literature. Thus, one could define high-frequency utilisers as patients that exceed the mean number of visits for their age group by at least 2 SDs, or whose number of visits is above the 90th percentile or at least twice the mean, or who arbitrarily seek care in PC clinics or emergency departments at least 10 times a year.15–17
The Health at a Glance 2017 report18 presents the most recent data on the health status of populations with the indicators of the Organisation for Economic Co-operation and Development (OECD), and shows that the number of visits per capita in Spain is above the mean of the rest of the countries.
Paediatricians have long been expressing concern about working conditions that jeopardise the quality of the care they provide to children, which is the priority objective of their daily activity, with quality of care referring to providing accessible services of the highest professional quality and with thoughtful use of available resources to achieve user satisfaction and loyalty.
There are few studies on the frequency of primary care utilisation,19 and their conclusions are controversial and have spurred debate regarding different levels of care, especially on the subject of urgent care delivery.20–22
The most important aspect in the profile of high-frequency utilisers of paediatric services is age less than 2 years.23 In this regard, our findings are consistent with the study of Oterino de la Fuente and Peiró Moreno24: children aged less than 2 years made the most visits to the paediatrician, which can be explained by the higher incidence of infection in this age group and the well-known risk factor that is attendance to child care centres.25 Furthermore, parents in this age group are often inexperienced – indeed, in our study 62.7% of the children were the first-born – and therefore more likely to worry significantly about illness in the child. In our study, the data confirmed the correlation between greater age and lower frequency of utilisation.
The family is considered a system that promotes health and improves quality of life, but this is actually contingent on certain aspects of family structure,26 so that anxiety, depression and/or the personality of parents are other factors that numerous publications have associated with healthcare overuse.27–32 Our study found an association between high-frequency utilisation and parental anxiety level, although we did not find an association with depression.
A novelty in our study was the use of the GADS, which is easy to use in PC and in a few minutes can offer a general idea of the level of anxiety and/or depression experienced by the parent or caregiver of the child, which allows intervention by health professionals to try to keep the emotional state of parents from distorting their perception of the child's health. Combining the anxiety score and the age of the child, we obtained a ROC curve with an AUC of 0.761 for prediction of 6 or more visits to the primary care centre in the period under study.
Other social factors that may have an impact on health care utilisation are socioeconomic status and the support and cohesion of family members; the immigrant population was heavily represented in our study, and we did not find this group to use health services more frequently than the native Spanish population, which was consistent with the results of Macipe Costa et al.33 We even found that the mean age at the time of utilisation was slightly greater in children of immigrant parents compared to those of Spanish parents.
Among the limitations of our study, we ought to highlight its small sample size, so we believe that it would be of interest to conduct further research on the subject in larger samples; furthermore, considering the complexity of the problem, we expect that the mere detection of abnormally high anxiety levels in parents will not prevent their continued overuse of services unless they are informed about this matter and/or undergo or are advised to pursue specialised assessment.
To conclude, we ought to emphasise that improving the problem of health care overuse requires the coordinated implementation of different measures at every level of care,34 to which end the recommendations for the management of urgent and non-deferrable conditions of the Technical Advisory Group on Primary Care Paediatrics of the Autonomous Community of Valencia35 are significantly useful. This group considers that population-based health education measures and coordination between PC and specialty care are necessary, as is the involvement of the competent administrations, although there are also authors that consider such interventions ineffective.36
Excessive workloads and the associated stress do not contribute to a decent professional and occupational situation for paediatricians37 nor, needless to say, to the quality of the care delivered to children, as demonstrated by the study conducted by Fernández San Martín et al.38 about the job satisfaction of health care professionals in the Community of Madrid.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Martín Martín R, Sánchez Bayle M, Teruel de Francisco C. Aspectos psicosociales relacionados con la hiperfrecuentación en las consultas pediátricas de atención primaria. An Pediatr (Barc). 2019;90:26–31.