To offer analgesia and sedation should be a priority in paediatric emergency departments. The aim of this study was to determine the effectiveness and safety of the sedation-analgesia procedure, as well as the satisfaction of the doctors, patients and parents.
MethodsA multicentre, observational, and prospective analytical study was conducted on the sedation-analgesia procedure performed on children younger than 18 years old in 18 paediatric emergency departments in Spain from February 2015 until January 2016.
ResultsA total of 658 procedures were recorded. The effectiveness was good in 483 cases (76.1%; 95% CI: 72.7–79.4%), partial in 138 (21.7%; 95% CI: 18.5–24.9%), and poor in 14 (2.2%; 95% CI: 1.1–3.4). The effectiveness was better when the doctor in charge was an emergency paediatrician (OR: 3.14; 95% CI: 1.10–8.95), and when a deeper level of sedation was achieved (OR: 2.37; 95% CI: 1.68–3.35). Fifty two children (8.4%) developed adverse drug reactions, more usually gastrointestinal, neurological or respiratory ones (89.9% were resolved in <2h). One patient was intubated. The older child and a deeper level of sedation were found to be independent risk factors for adverse reactions (OR: 1.18; 95% CI: 1.09–1.28 and OR: 1.86; 95% CI: 1.22–2.83, respectively). Thirteen children (5%) developed late adverse drug reactions, more commonly, dizziness and nauseas. A combination of midazolam/ketamine had been used in all the cases (RR: 24.46; 95% CI: 11.78–50.76). The perceived satisfaction level (0–10) was obtained from 604 doctors (mean: 8.54; SD: 1.95), 526 parents (mean: 8.86; SD: 1.49), and 402 children (mean: 8.78; SD: 1.70).
ConclusionsThe sedation-analgesia procedure performed in paediatric emergency departments by trained paediatricians seems to be useful, effective and safe, as well as satisfactory for all participants.
La sedoanalgesia debe ser una prioridad de los servicios de urgencias pediátricas. Analizamos la eficacia y seguridad de los procedimientos de sedoanalgesia así como la satisfacción del personal, pacientes y padres.
MétodosEstudio multicéntrico, prospectivo, observacional y analítico de los procedimientos de sedoanalgesia realizados a niños hasta los 18 años en 18 servicios de urgencias entre febrero de 2015 y enero de 2016.
ResultadosSe registraron 658 procedimientos (edad media: 6,8; DE: 4 años). La eficacia fue buena en 483 niños (76,1%; IC 95%: 72,7-79,4%), parcial en 138 (21,7%; IC95%: 18,5-24,9%) y mala en 14 (2,2%; IC 95%: 1,1-3,4). Se asoció con eficacias mejores la realización por el pediatra de urgencias (OR: 3,14; IC95%: 1,10-8,95) y un mayor nivel de sedación alcanzado (OR: 2,37; IC 95%: 1,68-3,35). Presentaron eventos adversos precoces 52 (8,4%) niños, siendo los más frecuentes: digestivos, neurológicos y respiratorios (el 89,9% remitieron en <2h). Un paciente requirió intubación. La mayor edad y la mayor profundidad de sedación fueron factores de riesgo independientes para presentar eventos adversos (OR: 1,18; IC 95%: 1,09-1,28 y OR: 1,86; IC 95%: 1,22-2,83, respectivamente). Trece niños (5%) presentaron eventos adversos tardíos, siendo el mareo y las náuseas/vómitos los más frecuentes; en todos ellos se usó la combinación midazolam/ketamina (RR: 24,46; IC 95%: 11,78-50,76). Registramos la satisfacción percibida (puntuación de 0-10) de 604 profesionales (media: 8,54, DE: 1,95), de 526 padres (media: 8,86; DE: 1,49) y de 402 niños (media: 8,78; DE: 1,70).
ConclusionesLos procedimientos de sedoanalgesia realizados por profesionales entrenados en los servicios de urgencias pediátricas españoles resultan útiles, eficaces y seguros, además de satisfactorios para todos los participantes.
Health care professionals in paediatric emergency departments (PEDs) have the duty to treat pain related to either disease and to the pain caused by invasive procedures, safely and efficiently, independently of the age and maturity of the child and the severity of disease, for physiological, moral, humane and ethical reasons.1
Adequate relief of pain and anxiety in diagnostic and therapeutic procedures is a quality indicator of the care given in PEDs.2
Sedation and analgesia procedures (SAPs) in PEDS are frequently performed by physicians who are not anaesthesiologists and are considered safe and effective.2,3 However, it is important to remember that sedatives and analgesics can cause adverse events.3,4 For this reason, scientific societies such as the American Academy of Pediatrics (AAP) and the American Society of Anesthesiologists (ASA) have issued guidelines and recommendations on SAPs. These societies consider that these procedures are safe as long as they are performed by physicians that are familiar with the use of these drugs and adequately trained in the identification of complications and basic life support skills.2,3
The success of SAPs can be assessed by considering their efficacy (completing a procedure without the patient having a bad experience or unpleasant memories from it), safety (adverse events) and the level of satisfaction expressed by the patients, the families and the health care providers that delivered sedation/analgesia.
ObjectiveOur main goal was to analyse the efficacy and safety of SAPs. Our secondary objective was to assess the satisfaction of health care staff, patients and parents and to identify the factors associated with adverse events.
Materials and methodsWe conducted a multicentre prospective observational and inferential study of SAPs performed in Spanish PEDs.
The study was approved by the competent ethics and research boards of each participating centre, in adherence with the Declaration of Helsinki. All participating centres requested a study classification according to the scheme of the Agencia Española de Medicamentos y Productos Sanitarios (Spanish Agency of Medicines and Medical Devices) of EPA-SP (post-authorisation observational prospective follow-up study).
We obtained the informed consent of the parents and/or legal guardians of all patients that participated in the study.
Study sample and settingWe conducted the study in 18 PEDs between February 1, 2015 and January 31, 2016. Participating hospitals belonged to the Working Group on Analgesia and Sedation of the Sociedad Española de Urgencias de Pediatría (Spanish Society of Paediatric Emergency Medicine).
We selected children that underwent some type of SAP with a dissociative anaesthetic, sedative and/or analgesic. We excluded patients that had only received a topical or local anaesthetic.
The inclusion criteria were age 18 years and informed consent for participation by the parents or legal guardians or, if the patient was mature enough, the patient.
All the selected patients met the inclusion criteria, and none were excluded from the study.
Data collectionA data collection notebook was filled out for each patient. Each hospital assigned a code to each of those notebooks using an alphanumeric sequence to safeguard patient confidentiality.
Every month, the researcher in each hospital submitted the collected data electronically to the principal investigator.
We collected epidemiological variables, patient-related variables (ASA physical classification, fasting, physical examination), technical variables (reason for sedation/analgesia, type of procedure, monitoring, pharmacological strategy, provider in charge, informed consent and parental presence), efficacy and safety of the procedure (early and late adverse events) and participant level of satisfaction.
DefinitionsType of analgesia or sedation procedure: (1) simple analgesia (administration of analgesics with the aim of preventing pain from a painful stimulus); (2) sedation (administration of sedatives/hypnotics with the aim of decreasing the level of consciousness and activity of the patient to a variable degree); (3) sedation and analgesia (administration of sedatives combined with analgesics or dissociative agents to induce a state that allows the patient to endure unpleasant procedures). This includes sedation/analgesia for mildly painful through very painful procedures.4
Pharmacological strategy: use of 1 drug or a combination of 2 or more drugs.
Depth of sedation: depth of sedation categorised as defined by the ASA into minimal sedation, moderate sedation, deep sedation and general anaesthesia.3
Outcome measuresWe defined the effectiveness of sedation as the creation of conditions necessary to safely facilitate the completion of a procedure.5 We considered effectiveness high if the procedure could be completed without resistance from the patient or the patient developing unpleasant memories, moderate if there was a certain level of unexpected pain or anxiety but the procedure was completed, and low if the procedure had to be abandoned or the patient reported having a bad experience.
We defined safe procedure as one where the number and severity of adverse events was minimised. Early adverse events were those that developed in the first 2h since performance of the SAP5 and late adverse events those that developed in the following 24h. To find the incidence of the latter, we made a phone call in the subsequent 48h to the parents/legal guardians of the patient.
We defined adverse events based on the classification of Pediatric Emergency Research Canada (PERC) and the Pediatric Emergency Care Applied Research Network (PECARN) consensus.5
We assessed the satisfaction of the participating health care professionals, parents/legal guardians and children on a Likert scale from 0 to 10 points, where 0 points stood for “totally dissatisfied” and 10 points for “totally satisfied”.
Statistical analysisWe analysed the collected data with the software SPSS version 21.0.
We have expressed categorical variables as absolute frequencies and percentages.
We have expressed quantitative variables with a symmetrical distribution as mean and standard deviation, and those with an asymmetrical distribution as median and interquartile range (IQR). We developed univariate and multivariate logistic regression models to analyse the association between risk factors, effectiveness and safety. To measure the strength of the association, we calculated the odds ratio (OR) or the relative risk (RR) with their corresponding 95% confidence intervals (CIs). We compared early and late adverse events by means of the chi square or the Fisher exact test. We compared satisfaction scores by means of the Student t test or ANOVA.
We defined statistical significance as a P-value of less than .05.
ResultsWe detected 658 SAPs performed in 18 Spanish PEDs. The median age of the patients was 6 years (IQR, 3–10 years).
Table 1 presents the characteristics of the sample.
Characteristics of the patients and of the sedation and analgesia procedures.
| n (%) | |
|---|---|
| Physical examination: documented in 652 patients (99%) | |
| Normal | 610 (93.6) |
| Potential risk of complications | 3 (0.5) |
| ASA physical status: documented in 593 patients (90%) | |
| I | 529 (80.4) |
| II | 56 (8.5) |
| III | 6 (0.9) |
| IV | 2 (0.3) |
| Fasting: documented in 538 patients (81%) | |
| <1h | 30 (4.6) |
| 1–2h | 208 (31.6) |
| 2–3h | 16 (2.4) |
| 3–4h | 81 (12.3) |
| 4–6h | 94 (14.3) |
| >6h | 109 (16.6) |
| Reason for sedation/analgesia | |
| Trauma-related procedures | 236 (35.9) |
| Surgical procedures | 187 (28.4) |
| Medical procedures | 124 (18.8) |
| Nursing procedures | 86 (13.1) |
| Imaging test | 14 (2.1) |
| Other | 11 (1.6) |
| Type of procedure | |
| Simple analgesia | 57 (8.7) |
| Anxiolysis/sedation | 44 (6.7) |
| SA for mildly painful procedure | 275 (41.8) |
| SA for very painful procedure | 282 (42.9) |
| Monitoring | |
| No monitoring | 178 (27.1) |
| Pulse oximetry | 460 (69.9) |
| Intermittent HR/BP monitoring | 127 (19.3) |
| Cardiac monitoring | 94 (14.3) |
| Antidote preparation | 58 (8.8) |
| Supplemental oxygen from beginning | 35 (5.3) |
| Capnography | 21 (3.9) |
| Provider performing sedation/analgesia | |
| Emergency paediatrician | 423 (64.3) |
| Non-emergency paediatrician | 44 (6.7) |
| 3rd–4thyear resident physician | 133 (20.2) |
| 1st–2ndyear resident physician | 38 (5.8) |
| Other | 20 (3.0) |
| Pharmacological strategy | |
| 1 Drug | 392 (59.6) |
| Nitrous oxide 50% | 225 (57.4) |
| Ketamine | 20 (5.1) |
| Midazolam | 61 (15.6) |
| Fentanyl | 54 (13.8) |
| Morphine | 24 (6.1) |
| Propofol | 1 (0.3) |
| Other | 7 (1.8) |
| Drug combination | 266 (40.4) |
| Midazolam+ketamine | 162 (60.9) |
| Fentanyl+nitrous oxide | 47 (17.7) |
| Midazolam+fentanyl | 32 (12.0) |
| Morphine+nitrous oxide | 7 (2.6) |
| Ketamine+fentanyl | 3 (1.1) |
| Other | 6 (2.3) |
| Combination of 3 or more drugs | 9 (3.4) |
| Informed consent request | |
| Verbal | 205 (31.2) |
| Written | 444 (67.5) |
| Not requested | 9 (1.4) |
| Parental presence during procedure | |
| No | 306 (46.5) |
| Yes | 352 (53.5) |
ASA, American Society of Anesthesiologists; BP, blood pressure; HR, heart rate; SA, sedation/analgesia.
Results expressed as absolute frequencies and percentages.
The decision to combine 2 or more drugs seemed to be associated with the type of procedure (simple analgesia, 5.3%; sedation, 19.2%; sedation/analgesia for mildly painful procedures, 29.5%; sedation/analgesia for very painful procedures, 62.1%; P<.001), the ASA physical status (I, 43.1%; II, 30.4%; III, 33.3%; IV, 0%; P=.038) and the facility (P=.022), but not with the type of provider that carried out the procedure (emergency paediatrician, 41.4%; other paediatrician, 40.9%; 3rd–4th year medical intern-resident [MIR], 41.4%; 1st–2nd year MIR, 34.2%; other, 25%; P=.243). However, in the multivariate analysis, the only variable that was significantly associated with the choice of pharmacological strategy was the type of procedure (P<.001), while the facility was not associated with the choice (P=.972).
The effectiveness was assessed for 635 SAPs, and was high in 483 patients (76.1%; 95% CI, 72.7%–79.4%), moderate in 138 (21.7%; 95% CI, 18.5%–24.9%) and low in 14 (2.2%; 95% CI, 1.1%–3.4%).
Table 2 shows the effectiveness outcomes based on patient characteristics and the sedation/analgesia procedures used.
Effectiveness of sedation/analgesia by patient characteristics and type of procedure.
| High | Moderate | Low | Not assessed | Total | |||||
|---|---|---|---|---|---|---|---|---|---|
| Anxiety | n | % | n | % | n | % | n | % | n |
| Gronninger 1 | 118 | 77.1 | 28 | 18.3 | 2 | 1.3 | 5 | 3.3 | 153 |
| Gronninger 2 | 125 | 73.5 | 38 | 22.4 | 3 | 1.8 | 4 | 2.4 | 170 |
| Gronninger 3 | 85 | 64.9 | 37 | 28.2 | 3 | 2.3 | 6 | 4.6 | 131 |
| Gronninger 4 | 95 | 78.5 | 17 | 14.0 | 3 | 2.3 | 6 | 5.0 | 121 |
| Gronninger 5 | 24 | 72.7 | 6 | 18.2 | 1 | 3.0 | 2 | 6.1 | 33 |
| Not assessed | 36 | 72.0 | 12 | 24.0 | 2 | 4.0 | 0 | 0.0 | 50 |
| Pharmacological strategy | n | % | n | % | n | % | n | % | n |
| 2 or more drugs | 207 | 77.8 | 42 | 15.8 | 6 | 2.3 | 11 | 4.1 | 266 |
| 1 drug | 276 | 70.4 | 96 | 24.5 | 8 | 2.0 | 12 | 3.1 | 392 |
| Provider | n | % | n | % | n | % | n | % | n |
| Emergency paediatrician | 340 | 80.4 | 67 | 15.8 | 8 | 1.9 | 8 | 1.9 | 423 |
| Other paediatrician | 30 | 68.2 | 13 | 29.5 | 1 | 2.3 | 0 | 0 | 44 |
| MIR 3–4 | 78 | 58.6 | 39 | 29.3 | 5 | 3.8 | 11 | 8.3 | 133 |
| MIR 1–2 | 26 | 68.4 | 11 | 28.9 | 0 | 0 | 1 | 2.6 | 38 |
| Other | 9 | 45 | 8 | 40 | 0 | 0 | 3 | 15 | 20 |
| ASA physical status | n | % | n | % | n | % | n | % | n |
| I | 392 | 74.1 | 104 | 19.7 | 14 | 2.6 | 19 | 3.6 | 529 |
| II | 47 | 83.9 | 7 | 12.5 | 0 | 0 | 2 | 3.6 | 56 |
| III | 2 | 33.3 | 3 | 50 | 0 | 0 | 1 | 16.7 | 6 |
| IV | 2 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| V | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Not assessed | 40 | 61.5 | 24 | 36.9 | 0 | 0 | 1 | 1.5 | 65 |
| Type of procedure | n | % | n | % | n | % | n | % | n |
| Simple analgesia | 39 | 68.4 | 18 | 31.6 | 0 | 0 | 0 | 0 | 57 |
| Sedation | 29 | 65.9 | 12 | 27.3 | 1 | 2.3 | 2 | 4.5 | 44 |
| SA, mildly painful procedure | 208 | 75.6 | 50 | 18.2 | 8 | 2.9 | 9 | 3.3 | 275 |
| SA, very painful procedure | 207 | 73.4 | 58 | 20.6 | 5 | 1.8 | 12 | 4.3 | 282 |
| Depth of sedation | n | % | n | % | n | % | n | % | n |
| Minimal sedation | 257 | 67.8 | 104 | 27.4 | 10 | 2.6 | 8 | 2.1 | 379 |
| Moderate sedation | 125 | 83.3 | 19 | 12.7 | 2 | 1.3 | 4 | 2.7 | 150 |
| Deep sedation | 81 | 91 | 6 | 6.7 | 1 | 1.1 | 1 | 1.1 | 89 |
| General anaesthesia | 5 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 5 |
| Not documented | 15 | 42.9 | 9 | 25.7 | 1 | 2.9 | 10 | 28.6 | 35 |
ASA, American Society of Anesthesiologists; MIR, medical intern-resident; SA, sedation/analgesia.
Results expressed as absolute frequencies and percentages.
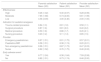
The drugs used most frequently by specialist physicians differed from the drugs used by medical residents, although in the multivariate analysis, only the higher depth of sedation achieved and the presumably greater experience of the provider that delivered the intervention were independently associated with greater effectiveness (Table 3). When it came to the provider performing the intervention, we only found a statistically significant difference in emergency paediatricians, with an OR of 3.14 (95% CI, 1.10–8.95).
Association of different factors with the effectiveness of the sedation/analgesia procedure in the univariate and multivariate analyses.
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| P | OR | (95% CI) | P | OR | (95% CI) | |
| Age | .072 | 1.04 | (1.00–1.09) | |||
| Anticipatory anxiety | .985 | 1.00 | (0.85–1.17) | |||
| Pharmacological strategy (2 or more drugs) | .014 | 1.63 | (1.10–2.40) | .119 | 0.67 | (0.41–1.11) |
| Type of provider | <.001 | 1.42 | (1.22–1.66) | <.001 | 1.35 | (1.15–1.58) |
| Emergency paediatrician | .006 | 4.03 | (1.51–10.79) | .032 | 3.14 | (1.10–8.95) |
| ASA physical status | .481 | 1.22 | (0.70–2.14) | |||
| Type of procedure | .104 | 1.13 | (0.98–1.31) | |||
| Depth of sedation | <.001 | 2.43 | (1.74–3.41) | <.001 | 2.37 | (1.68–3.35) |
| Midazolam | .750 | 0.94 | (0.65–1.37) | |||
| Ketamine | <.001 | 3.90 | (2.30–6.60) | .203 | 1.66 | (0.76–3.60) |
| Fentanyl | .062 | 0.66 | (0.43–1.02) | |||
| Morphine | .304 | 0.69 | (0.34–1.40) | |||
| Nitrous oxide | .813 | 1.05 | (0.72–1.51) | |||
ASA, American Society of Anesthesiologists.
We measured the strength of the association by means of the odds ratio (OR) with the corresponding 95% confidence interval (CI). We present statistically significant results in boldface.
A total of 52 children experienced early adverse events, the most frequent of which were neurological, respiratory and gastrointestinal (vomiting and nausea). Most of these adverse reactions (89.8%) resolved within 2h (Table 4).
Early and late adverse events associated with sedation and analgesia.
| n (%) | |
|---|---|
| Early (assessed in 658 children) | 52 (7.9) |
| Neurologic/change in behaviour | 21 (40.4) |
| Dizziness/vertigo | 12 (57.1) |
| Agitation | 4 (19.0) |
| Excitatory movements (myoclonus, muscle rigidity) | 2 (9.5) |
| Paradoxical response | 2 (9.5) |
| Unpleasant reaction during recovery | 1 (4.8) |
| Respiratory | 16 (30.8) |
| Hypoxia | 7 (43.8) |
| Central apnoea | 4 (25.0) |
| Total or partial obstructive apnoea | 3 (18.8) |
| Other | 2 (12.5) |
| Gastrointestinal | 15 (28.8) |
| Nausea | 6 (40.0) |
| Vomiting | 9 (60.0) |
| Permanent sequelae (neurologic impairment/death) | 0 (0) |
| Late (assessed in 258 children) | 13 (5.0) |
| Dizziness/vertigo | 3 (23.0) |
| Somnolence | 2 (15.4) |
| Nausea/vomiting | 2 (15.4) |
| Hallucinations | 1 (7.7) |
| Other (dry mouth, difficult urination, asthenia) | 5 (38.5) |
Results expressed as absolute frequencies and percentages.
We identified age as an independent risk factor for the development of early adverse events, with the number of adverse events increasing with increasing age (median, 9 [IQR, 6–11.75] vs median, 6 [IQR, 3–10]), which was also the case with the depth of sedation (proportion of patients with adverse events: minimal sedation, 5%; moderate sedation, 9.3%; deep sedation, 18%; general anaesthesia, 40%). We found a decreasing trend in the incidence of adverse events associated with the use of nitrous oxide that was nearly statistically significant (Table 5).
Association of different factors with the development of early adverse events in the univariate and multivariate analyses.
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| P | OR | (95% CI) | P | OR | (95% CI) | |
| Day of the week | .738 | 0.95 | (0.72–1.26) | |||
| Time | .952 | 1.01 | (0.80–1.26) | |||
| Hours of fasting | .031 | 1.22 | (1.02–1.46) | .252 | 1.12 | (0.92–1.37) |
| Sex | .229 | 0.69 | (0.37–1.27) | |||
| Age | .003 | 1.11 | (1.04–1.19) | <.001 | 1.18 | (1.09–1.28) |
| Provider | .882 | 0.98 | (0.77–1.26) | |||
| Type of procedure | .525 | 1.09 | (0.84–1.41) | |||
| Pharmacological strategy (2 or more drugs) | .002 | 2.54 | (1.42–4.55) | .578 | 1.32 | (0.50–3.45) |
| Depth of sedation | <.001 | 2.09 | (1.50–2.91) | .004 | 1.86 | (1.22–2.83) |
| ASA physical status | .043 | 0.63 | (0.40–0.99) | .127 | 0.71 | (0.46–1.10) |
| Midazolam | .004 | 2.35 | (1.32–4.18) | .683 | 0.84 | (0.37–1.94) |
| Ketamine | <.001 | 3.25 | (1.83–5.78) | .842 | 0.89 | (0.27–2.91) |
| Fentanyl | .951 | 1.02 | (0.51–2.05) | |||
| Morphine | .512 | 0.62 | (0.14–2.63) | |||
| Nitroso | .002 | 0.36 | (0.18–0.69) | .062 | 0.45 | (0.19–1.04) |
ASA, American Society of Anesthesiologists.
We measured the strength of the association by means of the odds ratio (OR) with the corresponding 95% confidence interval (CI). We present statistically significant results in boldface.
Respiratory adverse events consisted of decreases in oxygen saturation, and there were no cases of aspiration of gastric contents. The measures used to manage these events included head repositioning (10 children), bag-valve-mask ventilation (2 children) and tracheal intubation (1 child).
We observed an increased risk of vomiting in children who had fasted longer than 3h compared to a shorter time (RR, 1.63; 95% CI, 1.27–2.08). There were no cases of vomiting in children who had fasted for less than 2h.
We received reports of 13 late adverse events (5.0%; 95% CI, 2.4%–5.7%), the most frequent of which were dizziness, nausea/vomiting and somnolence (Table 4). All these patients had received a combination of midazolam/ketamine, which corresponded to a probability of 24.46% of adverse events using this combination (95% CI, 11.78%–50.76%).
We analysed whether children that developed late adverse events also experienced early ones, and found no association between the two (P=.345).
A total of 185 children (28.1%) required hospital admission, in 1.7% of these cases, it was due to the adverse event secondary to the SAP.
The satisfaction of the professionals that performed the SAPs was assessed in 604 cases (91.7%), and the mean score was 8.54 (SD, 1.95); parental satisfaction was assessed in 526 (80%), with a mean score of 8.86 (SD, 1.49) and patient satisfaction in 402 (61%), with a mean score of 8.78 (SD, 1.70).
We analysed the association between the level of satisfaction and effectiveness, and found higher satisfaction scores in providers, parents/guardians and patients when effectiveness was high compared to when effectiveness was moderate or low (P<.001). Furthermore, we found statistically significant differences in satisfaction based on the indication for sedation and analgesia (P<.001), with parents giving better ratings to sedation and analgesia for nursing procedures (mean: 9.23; SD: 1.2) and children worse ratings to trauma-related procedures (mean: 8.61; SD: 1.63).
We did not find significant differences based on the presence or absence of adverse events or the type of professional that carried out the SAP (Table 6).
Satisfaction scores in parents, children and health care providers.
| Parental satisfaction Mean (SD) | Patient satisfaction Mean (SD) | Provider satisfaction Mean (SD) | |
|---|---|---|---|
| Effectiveness | |||
| High | 9.26 (1.02) | 9.30 (0.97) | 9.28 (0.99) |
| Moderate | 7.65 (1.68) | 6.74 (2.06) | 6.61 (1.99) |
| Low | 4.56 (3.09) | 4.00 (3.46) | 2.00 (1.00) |
| Indication for sedation/analgesia | |||
| Trauma-related procedure | 8.84 (1.3) | 8.61 (1.6) | 8.58 (1.1) |
| Surgical procedure | 8.87 (1.6) | 8.81 (2.0) | 8.40 (2.2) |
| Medical procedure | 8.50 (1.8) | 8.86 (1.7) | 8.45 (2.1) |
| Nursing procedure | 9.23 (1.2) | 9.11 (1.3) | 8.85 (1.5) |
| Provider | |||
| Emergency paediatrician | 8.97 (1.51) | 8.91 (1.75) | 8.57 (2.01) |
| Paediatrics MIR | 8.58 (1.51) | 8.38 (1.74) | 8.20 (2.01) |
| Non-emergency paediatrician | 8.96 (1.51) | 8.87 (1.73) | 8.47 (2.03) |
| Nurse | 8.82 (1.52) | 8.76 (1.75) | 8.46 (2.02) |
| Early adverse event | |||
| Yes | 8.77 (1.24) | 8.38 (1.84) | 7.59 (2.58) |
| No | 8.82 (1.51) | 8.73 (1.74) | 8.46 (2.00) |
MIR, medical intern-resident.
Results expressed as mean and standard deviation (SD).
The effectiveness of SAPs depends on the adequate use of analgesics and/or sedatives.6 In our study, the effectiveness of SAP was high in two thirds of the patients, and low in only a very few cases.
Some studies have found an association between age and a decreased efficacy, as fear of adverse events may lead to underdosing in younger patients.7 In our study, we did not find differences in effectiveness based on age.
Emergency paediatricians achieved a higher effectiveness compared to resident physicians or other providers. This may be due to the emergency paediatricians having more experience on this area. Among other requirements, current guidelines recommend that non-anaesthesiologists performing SAPs receive specific training on and be well acquainted with the pharmacology of sedatives and analgesics.3,8,9
We found that some SAPs were performed by first- and second-year medical residents who used drugs, alone or in combination, that could produce serious adverse events. This practice contravenes international guidelines, which recommend that any provider performing SAPs must be knowledgeable of the drugs and have the skills to rescue patients whose level of sedation becomes deeper than initially intended and to identify and manage complications.3,8 For this reason, certain providers should not be performing SAPs without the supervision of professionals with specialised training.
Some procedures are potentially more painful than others, but we did not find any differences in effectiveness based on the reason for using sedation/analgesia. A possible explanation is that the choice of a specific pharmacological strategy depends on multiple factors, and not only on the indication for sedation/analgesia, such as age, the intrinsic characteristics of the patient, the expected level of pain, the type of SAP, the duration of the diagnostic or therapeutic procedure to be performed and the expertise of the provider performing the SAP.10
The selected pharmacological strategy did not vary based on the type of provider delivering sedation/analgesia nor the age of the patient; we only found differences based on the type of SAP, which may suggest the presence of protocols that establish to a varying degree which drugs are used depending on the type of SAP.
Although we found no differences in effectiveness based on the chosen pharmacological strategy, the univariate analysis suggested that effectiveness improved with the use of ketamine. Ketamine is widely used in PEDs because it provides sedation and analgesia effectively and safely without compromising the protective reflexes of the airways.11–13
In our study, we found a proportion of early adverse events of 7.9%. The incidence in other studies has ranged from the 2.3% reported by Pena and Krauss14 to the 17% reported by Roback et al.,7 Pitetti et al.15 or Wenzel and Schweitzer.16 These differences may be due to differences in the definitions of complications. Pena and Krauss14 defined hypoxia as an oxygen saturation of 90% or less, while Pitetti et al.15 used a threshold of 93%. In our study, we defined hypoxia as a decrease in O2 saturation below 94% lasting more than 15seconds and requiring supplemental oxygen.5
Other studies have tried to identify risk factors for adverse events related to SAPs. Coté et al.17 identified a few, such as sedation outside the hospital setting, poor monitoring, lack of an adequate evaluation before sedation, medication errors and absence of an independent observer.
In our study, the only factors associated with the incidence of adverse events were age and depth of sedation, with increasing age and increasing depth of sedation correlating to a greater probability of adverse events. Pitetti et al. also observed this correlation with age (mean age in adverse event group, 7.4 vs 6.6 years in group without adverse events; P=.02).15
There is evidence that the risk of adverse events increases with the use of 2 or more analgesics.15,17,18 Our data suggested a similar trend in the univariate analysis, but the association was not confirmed by the multivariate analysis.
There were few respiratory adverse events in our patients (<3%), most of which corresponded to decreases in oxygen saturation. This incidence was lower than those reported by Pitetti et al. (14%)15 and Wenzel and Schweitzer (4.2%).16
We ought to highlight that most of our patients were monitored by means of pulse oximetry and capnography, a method that allows earlier and more frequent detection of changes in saturation19,20 in a small percentage (3%).
The proportion of vomiting as an adverse reaction was low (2%) and inferior to the proportions reported in other case series.7,15
The published evidence has not established a clear association between a short duration of fasting and the development of vomiting.21–23 In our study, the risk of vomiting was greater when the duration of fasting exceeded 3h. The underlying mechanism of this finding is unknown; a possible explanation is that prolonged fasting leads to hypoglycaemia and subsequently to ketosis, which can cause nausea and vomiting. Some recent guidelines recommend consumption of clear fluids with carbohydrates up to 2h before surgery to prevent dehydration and increases in catabolism.21,22,24
The duration of fasting before a SAP is a controversial subject. Fasting rules are defined in reference to the guidelines of the ASA,2 but in emergency care decisions need to be made on a case-by-case basis, weighing the risks of potential vomiting against the benefits of sedation/analgesia taking into account the desired depth of sedation.2,22 In agreement with other published series, we did not observe any cases of aspiration of gastric contents.7,15,23
At the time of discharge of a child that has undergone a SAP, it is important to give instructions regarding potential late adverse events and to ensure that an adult is supervising the child. In our study, we found adverse events in 5% of patients (vomiting, dizziness and somnolence), all of whom had received a combination of midazolam and ketamine. Other studies have reported greater proportions of late adverse events (10%–22.4%).15,24–27 On the other hand, Wathen et al.25 did not find any differences between the use of ketamine alone and its use in combination with midazolam, while other studies have found an association between a higher incidence of late adverse events and the combined use of ketamine and midazolam26 or of midazolam alone compared to the exclusive use of nitrous oxide27.
The satisfaction of the involved parties (health providers, patients and family members) was another important factor to consider in relation to SAPs. Our scores were highly satisfactory in all groups, improving with increasing effectiveness and varying based on the reason that the SAP was performed.
In most of the studies that we reviewed, parental or patient satisfaction was used as a measure for comparison of 2 pharmacological strategies,28–30 but we found no references in the literature that analysed satisfaction in relation to the indication for sedation or analgesia, the type of SAP or the staff performing the procedure.
There are several limitations to our study. Firstly, all participating PEDs belong to the Working Group on Analgesia and Sedation of the Sociedad Española de Urgencias de Pediatría, which may limit the generalisation of our findings to other centres. However, the participating PEDs represented hospitals of different levels of care and in different geographical regions, which in our opinion makes them a group that is quite representative of Spanish PEDs overall. Second, the frequency distribution of SAPs by type of professional was uneven, as most procedures were performed by emergency paediatricians. Last of all, we were only able to investigate the development of late adverse events through a telephone call in 258 children (39% of the sample), which may have led to underestimation of their incidence.
In conclusion, the use of sedation and analgesia for pain and anxiety relief seems safe and effective, especially when these procedures are performed by trained professionals. Furthermore, its use is associated with a high level of satisfaction in providers as well as patients and their families.
Conflicts of interestThe authors have no conflicts of interest to declare.
Concepción Míguez Navarro (Paediatric Emergency Department, Hospital General Universitario Gregorio Marañón, Madrid).
Niki Oikonomopoulou (Paediatric Emergency Department, Hospital General Universitario Gregorio Marañón, Madrid).
Arístides Rivas García (Paediatric Emergency Department, Hospital General Universitario Gregorio Marañón, Madrid).
Andrea Mora Capín (Paediatric Emergency Department, Hospital General Universitario Gregorio Marañón, Madrid).
Gloria Guerrero Márquez (Paediatric Emergency Department, Hospital General Universitario Gregorio Marañón, Madrid).
Ana Isabel Fernández Lorente (Paediatric Emergency Department, Hospital General de Basurto, Basurto).
Pilar Storch de Gracia Calvo (Paediatric Emergency Department, Hospital Infantil Niño Jesús, Madrid).
Eva Benito Ruiz (Paediatric Emergency Department, Hospital Infantil Miguel Servet, Zaragoza).
Elena Sancho Gracia (Paediatric Emergency Department, Hospital Infantil Miguel Servet, Zaragoza).
Olga Serrano Ayestarán (Paediatric Emergency Department, Hospital de Salamanca, Salamanca).
Cristina Cordero Castro (Paediatric Emergency Department, Hospital Rey Juan Carlos, Mostoles).
Cecilio Palomino Muñoz (Paediatric Emergency Department, Hospital de Getafe, Getafe).
Sofía Mesa García (Paediatric Emergency Department, H. Doce de Octubre, Madrid).
Cristina Muñoz López (Paediatric Emergency Department, Hospital Infanta Leonor, Madrid).
Nuria Clerigué Arrieta (Paediatric Emergency Department, Complejo Hospitalario de Navarra B, Navarre).
Jorge Álvarez García (Paediatric Emergency Department, Complejo Hospitalario de Navarra B, Navarre).
Isabel Cubero (Paediatric Emergency Department, Hospital Clínico San Cecilio, Granada).
José Luis Fernández Arribas (Paediatric Emergency Department, Hospital Río Hortega, Valladolid).
Alberto Barasoain Millán (Paediatric Emergency Department, Fundación Alcorcón, Alcorcon).
Juan Alonso Cozar Olmo (Paediatric Emergency Department, Hospital San Agustín, Linares).
José Luis Cuevas Cervera (Paediatric Emergency Department, Hospital San Agustín, Linares).
Carlos García Vao Bel (Paediatric Emergency Department, Hospital del Tajo, Aranjuez).
M. José Carbonero Celís (Paediatric Emergency Department, Hospital Virgen de la Macarena, Seville).
M. José Carpio Linde (Paediatric Emergency Department, Hospital Virgen de la Macarena, Seville).
M. Teresa Alonso Salas (Paediatric Emergency Department, Hospital Virgen del Rocío, Seville).
Please cite this article as: Míguez Navarro C, Oikonomopoulou N, Rivas García A, Mora Capín A, Guerrero Márquez G, en representación del Grupo de Analgesia y Sedación de la Sociedad Española de Urgencias de Pediatría. Eficacia, seguridad y satisfacción de los procedimientos de sedoanalgesia en las urgencias españolas. An Pediatr (Barc). 2019;90:32–41.
Appendix A lists all the authors of the article.
Previous presentations: the findings of this study were presented under the title Eficacia, seguridad y satisfacción de los procedimientos de sedoanalgesia en los servicios de urgencias pediátricos españoles (Niki Oikonomopoulou, Conepción Míguez, Arístides Rivas [Hospital General Universitario Gregorio Marañón. Madrid], Working Group on Analgesia and Sedation of the Sociedad Española de Urgencias de Pediatría: Ana Isabel Fernández, Pilar Storch, Gloria Guerrero, Eva Benito and Elena Sancho, Olga Serrano, Cristina Cordero, Cecilio Palomino, Sofía Mesa, Cristina Muñoz, Nuria Clerigué and Jorge Álvarez García, Isabel Cubero, José L Fernández, Alberto Barasoain, Juan Alonso Cozar and José Luis Cuevas, Clara García y Carlos García Vao, M. José Carbonero and M. José Carpio Linde, M. Teresa Alonso, Vicente Barea) at the 21 Annual Meeting of the Sociedad Española de Urgencias de Pediatría, April 14–16, 2016; Valencia, Spain.