Propionic acidaemia (OMIM 606054) is an autosomal recessive organic acid metabolism disorder that involves a defective form of propionyl-CoA carboxylase (PCC). The disease usually manifests with acute and potentially fatal episodes of metabolic decompensation and delays in cognitive development. Its association with cardiomyopathy, usually dilated, is well known, and usually manifests during the episodes of metabolic decompensation. More recently, propionic acidaemia has been associated with long QT syndrome1,2 (the normal range in children older than 1 year is defined by a heart-rate corrected QT interval [QTc]<440ms),3 which can predispose the patient to the development of ventricular arrhythmias and sudden death. Its exact aetiology is not known and its treatment is similar to that of long QT without associated propionic acidaemia.
We present the case of one girl with propionic acidaemia in whom the electrocardiogram (ECG) revealed prolongation of the QTc.
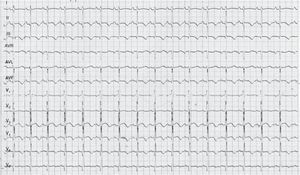
The patient was a girl aged 10 years diagnosed in the neonatal period as having propionic acidaemia and followed up by the congenital errors of metabolism unit. The patient was undergoing treatment with l-carnitine and a protein-restricted diet. She was referred to the paediatric cardiology unit for assessment. The patient had no cardiovascular symptoms. There was no family history of sudden death or heart disease. The findings of the physical examination and echocardiogram were normal. The ECG revealed a sinus rhythm with normal voltages, but with a QTc interval of 500ms (calculated by Bazett's formula) and repolarization abnormalities with negative T waves in the inferior (II, III and aVF) and left precordial leads (V4–V6) (Fig. 1). Both parents were evaluated, and the ECG did not reveal any abnormal findings in either. The patient wore a Holter monitor for 24h, which recorded a maximum QTc of 500ms, with no evidence of arrhythmias. Laboratory tests were performed, including measurement of electrolyte, glucose, ammonia, plasma amino acids and acylcarnitine levels, the results of which were normal. Treatment of long QT syndrome was initiated with oral propanolol. Subsequent evaluations showed that the patient remained free of cardiovascular symptoms and tolerated therapy with propanolol, while prolongation of the QTc persisted in the ECG (QTc, 440–480ms).
Propionic acidaemia is caused by the deficient activity of PCC, a biotin-dependent mitochondrial enzyme needed for the conversion of propionyl-CoA to d-methylmalonyl-CoA. PCC is a heteropolymer composed of two types of subunits, α and β, that are encoded by the PCCA gene (13q32) and PCCB gene (3q21-q22), respectively. Mutations in these genes cause the disease. The genetic defect leads to the intramitochondrial accumulation of propionyl-CoA that is metabolised by secondary pathways to other metabolites. Its prevalence is of one case per 100,000 live births worldwide. It can present in the following forms: severe neonatal onset, intermittent late onset or a chronic progressive form.
Cardiac involvement is relatively frequent, and cardiomyopathy develops in one-fourth to one-third of patients with propionic acidaemia, which does not respond to supplementation with carnitine.4 On the other hand, a recent prospective longitudinal study of 10 patients with propionic acidaemia5 found that 70% of them had a prolonged QT interval (QTc>440ms), and that the interval was longer than 460ms in 60%. The lengthening of the QT interval was unrelated to the metabolic status of the patients. It was observed both in school-aged children and adolescents, but not in infants. The same study reported that the most frequent ECG changes besides QT prolongation were repolarization abnormalities with T-wave inversion in leads V4–V6, abnormalities that we also found in the ECGs of our patient.
Although the exact underlying mechanism of the association between these two entities remains unknown, some authors have proposed that changes in heart conduction could be due to carnitine deficiency.6
From the perspective of clinical practice, this case suggests that patients with propionic acidaemia may be at greater risk of experiencing prolongation of the QT interval, so we recommend a yearly cardiovascular evaluation including a 12-lead ECG and a 24-h Holter recording in addition to the echocardiogram. If the presence of long QT syndrome were confirmed, initiation of beta-blocker therapy would be indicated to prevent ventricular arrhythmias, syncope or sudden death. It is also important that the parents and the patient are informed of the risk of using various medicines that may lengthen the QT interval and thus promote the development of ventricular arrhythmias.
Please cite this article as: Moure AF, Jiménez MC, García-Rovés RÁ, Villanueva NG, López CM. Acidemia propiónica y síndrome QT largo: una asociación potencialmente grave. An Pediatr (Barc). 2015;83:281–282.