The most widely used tool for assessing breastfeeding self-efficacy is the Breastfeeding Self-Efficacy Scale-Short Form (BSES-SF). This study assesses the relationship between the BSES-SF score and the risk of breastfeeding (BF) cessation and determines the cut-off point in the scale score that optimizes detection of this risk in primary health care pediatric consultations.
MethodsSecondary data analysis of the LAyDI study. Cohort study carried out through a research network of primary care pediatricians (PAPenRed). A newborn was recruited every month for one year by 210 pediatricians. The cohort was followed for 24 months. Mothers responded to the BSES-SF at the first visit. General pregnancy and delivery data were collected and assessed to determine whether breastfeeding was exclusive or supplemented during the first 6 months.
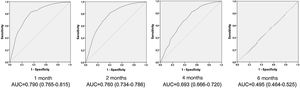
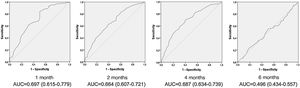
ResultsN = 1845. The Area Under the ROC Curve for the exclusive BF was 0.790 (0.765-0.815) the first month and 0.760 (0.734-0.786) the second month. For 4 and 6 months, as well as for any age in mothers who give supplemented BF, the Area Under the Curve was less than 0.75 and its predictive capacity was not considered to be good. For a sensitivity of 80% in detecting mothers at risk of BF cessation with the BSES-SF, the cut-off score was 58.
ConclusionsMothers with a BSES-SF score below 58 points in primary health care, are at risk of early withdrawal of exclusive BF within two months.
El instrumento utilizado habitualmente para valorar la autoeficacia de la lactancia materna es la Breastfeeding Self-Efficacy Scale-Short Form (BSES-SF). Este estudio valora la relación entre la puntuación de la BSES-SF y el riesgo de abandono de la lactancia. También se determina el punto de corte en la puntuación de la escala que optimiza la detección de este riesgo desde Atención Primaria.
MétodosAnálisis secundario de datos del estudio LAyDI. Estudio de cohorte única realizado a través de la red de investigación de pediatras de Atención Primaria (PAPenRed). Cada pediatra reclutó un recién nacido cada mes durante un año. Se siguió la cohorte 24 meses. Las madres respondieron la BSES-SF en la primera visita. Se recogieron datos generales de embarazo y parto y se valoró la lactancia materna (suplementada o exclusiva) hasta los 6 meses.
Resultadosn = 1845. El Área Bajo la Curva ROC para la LM exclusiva fue al primer mes de 0,79 (0,77–0,82) y al segundo mes de 0,760 (0,734-0,786). Para los 4 y 6 meses, así como para cualquier edad en madres que dan LM suplementada, el Área Bajo la curva fue menor de 0,75 y su capacidad predictiva no se consideró adecuada. Para una sensibilidad del 80% en la detección de madres en riesgo de abandono de la lactancia la puntuación de corte fue 58.
ConclusionesLas madres que en Atención Primaria presenten una puntuación en la BSES-SF por debajo de 58 puntos tienen riesgo de abandono de la lactancia materna exclusiva antes de los dos meses.
The prevalence of breastfeeding (BF) in Spain has been increasing progressively in recent years. The frequency of exclusive BF at 6 months of life has increased from 28.5% in 2011 to 39% in 2017.1 However, we are still far from fulfilling the recommendation of the World Health Organization to maintain exclusive BF through age 6 months.2
Multiple factors have been found to be associated with early discontinuation of BF, including maternal age, educational attainment or psychosocial status.3 Although these are not modifiable factors, it is important to be aware of them in order to identify mothers at risk of discontinuing BF. On the other hand, there are modifiable factors on which it is possible to act to attempt to minimise this risk.4
One of the modifiable risk factors for early BF discontinuation is the lack of support to mothers from health care professionals.3,5 Providers in maternity wards play an important role in the successful establishment of BF, and primary care providers in its successful maintenance over time.6,7 To achieve this goal, it is essential that validated tools be available to objectively assess BF. At present, there are several scales that assess BF technique through the direct observation of a feed by a health care professional.8,9 The use of scales facilitates the standardization of assessment criteria and objective identification of aspects in need of improvement.6 We recommend observation of at least one full feed in the maternity ward and another one when the infant enters the primary care system.6
There is another important factor at play in the maintenance and exclusivity of BF: self-efficacy. The level of this trait in mothers is also a good predictor of early BF discontinuation.10,11 Self-efficacy refers to how competent and confident women feel about their ability to breastfeed. The main aspects that contribute to this factor are previous personal experience BF, past vicarious experience of BF in others, the physical and psychological condition of the mother and verbal persuasion by others.12 Previous studies have demonstrated that self-efficacy is a modifiable factor and that interventions that improve self-efficacy achieve an increase in BF duration and exclusive BF.4,13,14 Thus, instruments for assessment of self-efficacy can be useful and help identify mothers at risk of premature discontinuation of BF.13
The scale used most frequently for this purpose is the Breastfeeding Self-Efficacy scale-short form (BSES-SF), developed in Canada in 2003.12 The BSES-SF has been translated to different languages and adapted to different cultures and exhibited an adequate validity and reliability.15–21 There is also a validated version of the scale in Spanish.22 In addition, the BSES-SF has been found to be a good predictor of early BF discontinuation, with lower scores in the scale associated with an increased risk of discontinuation.18,19,23,24
This motivated us to assess the potential usefulness of the BSES-SF as a predictor of BF practices at the primary care level. The BSES-SF is a simple and feasible scale that could be very helpful to health care professionals. In addition, we sought to establish the optimal cut-off point to identify mothers at risk of BF discontinuation.
MethodsThe data used in this study were obtained in the context of the study Lactancia y Desarrollo Infantil (Breastfeeding and Infant Development, LAyDI), so the results presented here are from a secondary analysis of the data obtained in said project.
Design and settingThe LAyDI is a single cohort study with the primary objective of establishing whether there is an association between the feeding modality in infancy and future developmental outcomes. This study was conducted through the Primary Care Paediatrics Research Network (Spanish abbreviation, PAPenRed) of the Asociación Española de Pediatría de Atención Primaria. PAPenRed is composed of 320 paediatricians of the Spanish public health system with a distribution that matches the population distribution by autonomous community, leading us to assume that the results of the study are representative of the entire Spanish territory.
Study periodData collection started on April 1, 2017 and ended on March 31, 2020.
Sample selection and data collectionThroughout the period under study, collaborating paediatricians each recruited up to 12 newborn infants. Since we intended to analyse morbidity data, in order to eliminate seasonal bias we decided that, for a full year, paediatricians would recruit the first infant born each month that met all the eligibility criteria. We followed up the resulting cohort through age 2 years.
Data were collected in the first primary care visit (within 15 days post birth) and at 1, 2, 4, 6, 12, 18 and 24 months post birth. In our study, we used the data collected through age 6 months. The BSES-SF was completed by mothers in the initial appointment. During this appointment, the paediatricians also collected information regarding the pregnancy and delivery in addition to information on the neonate and the parents. In subsequent visits, paediatricians collected information on the feeding modality of the infant. In each visit, data were collected in a form developed for the purpose. Once data collection was completed, each paediatrician submitted a report. The sources of information used to fill out these forms were the mothers themselves, labour and delivery discharge summaries, official child health notebooks, patient health records and emergency department reports.
The inclusion criteria were: infant born at term (>37 weeks gestational age) brought for the initial paediatric primary care visit before 15 days post birth and written informed consent signed by the mother.
The exclusion criteria were low birth weight (less than 2400 g in boys and 2100 g in girls), multiple birth, length of stay in maternity ward or neonatal unit greater than 5 days, presence of malformations or severe disease, history of moderate to severe disease in the mother during pregnancy or the postpartum period, language barrier, refusal of family to participate and families whose usual geographical mobility patterns precluded follow-up.
SampleIn 2015, a total of 426 303 children were born in Spain. Given a 2.5% margin of error for a 95% level of confidence for the entire paediatric population residing in Spain, we estimated that we needed a minimum sample size of 1500 to represent the entire paediatric population of Spain.
Study variablesThe LAyDI study collected data on a large number of variables. The variables that we used for our study were the following:
Primary outcomes:
- •
Exclusive BF: defined as the infant being exclusively breastfed in the past 7 days.
- •
Mixed feeding: defined as the infant having been breastfed in the past seven days, but also fed any amount of artificial formula, other water-based fluids or any other form of nutrition other than BF.
- •
Score in the BSES-SF: unidimensional scale consisting of 14 items that present statements about BF to be rated by the mothers on a Likert scale ranging from “not at all confident” (1 point) to “always confident” (5 points). Thus, the total score can range from a minimum of 14 points to a maximum of 70.
Other variables analysed in the study:
- •
Maternal characteristics: age, educational attainment, immigration status, employment status, marital status.
- •
Pregnancy and delivery: primiparity, weeks of gestation, hospital where infant was born, type of delivery.
- •
Infant characteristics: Apgar score, sex, birth weight, age at first visit.
The PAPenRED project obtained overall approval from the Scientific Research Ethics Committee of Aragon (File 19/2013; C.P.-C.I. PI13/00154). The LAyDI study was approved by the Research Ethics Committee of the Principality of Asturias (project no. 213/16). It also received a positive review from the Central Research Commission of the Department of Health of Madrid. All the collected data were anonymised and confidentiality safeguarded in adherence with Regulation (EU) 2016/679. Mothers received adequate information about the study, and those who expressed an interest in participating were asked to sign an informed consent form.
Statistical analysisWe performed a descriptive analysis of the cohort under study. We calculated the total score in the BSES-SF and the differences in the scores obtained by mothers that offered exclusive BF versus those offering mixed feeding by means of the t test. We considered p-values of 0.05 and less statistically significant.
We used the BSES-SF scores obtained in the initial visit to generate receiver operating characteristic (ROC) curves for each age group (1, 2, 4 and 6 months) for both the exclusive BF and the mixed feeding groups. For each curve, we calculated the area under the curve (AUC) with the corresponding 95% confidence interval (CI). We considered that the predictive power of a ROC curve was poor if the AUC was less than 0.59, fair if the AUC was between 0.6 and 0.74, good if the AUC was between 0.75 and 0.89 and very good if the AUC was greater than 0.9.
If the AUC showed a good or very good predictive power, we also calculated the sensitivity and specificity for those curves starting from scores of 30 points in the BSES-SF. We established a minimum sensitivity threshold of 80% for the calculation of the optimal cut-off point.
We performed the statistical analysis of the data with the software Statistical Package for the Social Sciences (SPSS) version 22.0.
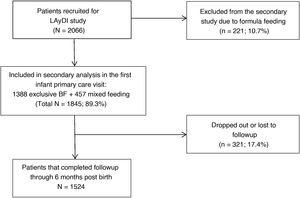
ResultsA total of 210 paediatricians of the network participated in the LAyDI study. Fig. 1 presents a flowchart of the sample under study. We found the following rates of BF in the initial primary care visit: exclusive BF, 67.2% (65.1%–69.2%), mixed feeding, 22.1% (20.4%–24.0%) and formula feeding 10.7% (9.4%–12.1%). The mean age of the infants in the initial visit was 10.8 days (standard deviation [SD], 4.0). Table 1 summarises the main characteristics of the participants at the beginning of the study.
Main characteristics of the sample by feeding modality.
| MF | EBF | |
|---|---|---|
| n = 457 | n = 1388 | |
| [0.1−3]Maternal characteristics | ||
| [0.1−3]Age, n (%) | ||
| <20 years | 2 (0.4%) | 17 (1.2%) |
| 20−24 years | 25 (5.5%) | 59 (4.3%) |
| 25−29 years | 63 (13.8%) | 176 (12.6%) |
| 30−34 years | 159 (34.8%) | 536 (38.6%) |
| 35−39 years | 157 (34.4%) | 473 (34.2%) |
| 40−44 years | 46 (10.0%) | 120 (8.6%) |
| > 44 years | 5 (1.1%) | 7 (0.5%) |
| [0.1−3]Educational attainment, n (%) | ||
| No education | 2 (0.5%) | 5 (0.4%) |
| Elementary | 48(10.5%) | 104 (7.5%) |
| Secondary | 199 (43.6%) | 536 (38.6%) |
| University | 208 (45.5%) | 743 (53.5%) |
| Immigrant, n (%) | 119 (26.0%) | 299 (21.5%) |
| Employed, n (%) | 381 (83.4%) | 1158 (83.4%) |
| Single, n (%) | 5 (1.1%) | 19 (1.3%) |
| [0.1−3] | ||
| [0.1−3]Pregnancy and delivery | ||
| First pregnancy, n (%) | 172 (37.6%) | 722 (52.1%) |
| Weeks of gestational age (median) | 40 | 40 |
| Delivery in public hospital, n (%) | 385 (84.2%) | 1188 (85.6%) |
| Type of delivery, n (%) | ||
| Vaginal | 346 (75.7%) | 1169 (84.2%) |
| Elective caesarean | 48 (10.5%) | 83 (6.0%) |
| Emergency caesarean | 63 (13.8%) | 136 (9.8%) |
| [0.1−3] | ||
| [0.1−3]Infant characteristics | ||
| 1-minute Apgar (Median) | 9 | 9 |
| 5- minute Apgar (Median) | 10 | 10 |
| Female sex, n (%) | 224 (49.1%) | 692 (49.9%) |
| Birth weight in g | 3279 ± 417 | 3324 ± 389 |
| Mean (standard deviation) | ||
| Days of age at initial visit | 10.7 ± 3.5 | 10.5 ± 3.7 |
| Mean (standard deviation) | ||
EBF, exclusive breastfeeding; supplemental feeding: MF, mixed feeding.
The mean BSES-SF score in the total sample was 59.76 points (SD, 9.95). The mean score in each of the groups was 62.54 points (SD, 7.91) in the exclusive BF group compared to 51.79 points (SD, 10.88) in the mixed feeding group. This corresponds to a difference between the 2 groups of 10.42 points (P < .001).
Fig. 2 shows the ROC curves obtained from the BSES-SF scores of mothers that exclusively breastfed their infants. We ought to note that only the curves corresponding to the visits at 1 and 2 months had an AUC above the threshold established to define good predictive power (0.75).
Fig. 3 presents the ROC curves of mixed feeding group. In this instance, there were no AUCs greater than 0.75 in any infant age group.
Since the only curves with AUCs above the threshold for good predictive power were those in the exclusive BF group at 1 and 2 months, these were the age groups for which we calculated the sensitivity and specificity of BSES-SF scores ranging from 30 to 70 points. The results are presented in Table 2. As can be seen in the table, a sensitivity of 80% was achieved with a score of 59 points at 1 month and 58 points at 2 months.
Sensitivity and specificity of different cut-off values for the BSES-SF score in mothers that breastfeed exclusively.
| Cut-off | EBF first month | EBF second month | ||
|---|---|---|---|---|
| Sen | Spe | Sen | Spe | |
| 30 | 99.0 | 4.0 | 98.9 | 3.6 |
| 31 | 98.9 | 4.4 | 98.9 | 4.1 |
| 32 | 98.9 | 5.3 | 98.8 | 4.7 |
| 33 | 98.9 | 5.7 | 98.8 | 5.1 |
| 34 | 98.8 | 6.5 | 98.7 | 5.7 |
| 35 | 98.8 | 7.4 | 98.7 | 6.5 |
| 36 | 98.8 | 8.6 | 98.7 | 7.9 |
| 37 | 98.8 | 9.2 | 98.7 | 8.3 |
| 38 | 98.8 | 10.9 | 98.7 | 9.9 |
| 39 | 98.8 | 11.1 | 98.7 | 10.3 |
| 40 | 98.8 | 13.0 | 98.7 | 12.2 |
| 41 | 98.7 | 14.3 | 98.6 | 13.4 |
| 42 | 98.7 | 15.1 | 98.4 | 13.8 |
| 43 | 98.1 | 17.4 | 97.9 | 16.4 |
| 44 | 97.8 | 18.9 | 97.6 | 17.6 |
| 45 | 97.5 | 21.6 | 97.3 | 20.5 |
| 46 | 97.2 | 24.2 | 96.9 | 22.7 |
| 47 | 96.7 | 26.7 | 96.5 | 24.9 |
| 48 | 96.3 | 28.6 | 96.1 | 26.6 |
| 49 | 95.4 | 31.9 | 95.1 | 30.2 |
| 50 | 95.0 | 34.0 | 94.6 | 32.0 |
| 51 | 94.2 | 36.6 | 93.9 | 34.7 |
| 52 | 93.1 | 38.9 | 92.6 | 36.7 |
| 53 | 91.9 | 43.1 | 91.4 | 41.2 |
| 54 | 90.1 | 47.5 | 89.5 | 45.2 |
| 55 | 88.5 | 50.4 | 87.9 | 47.7 |
| 56 | 85.7 | 54.4 | 85.4 | 52.1 |
| 57 | 84.1 | 61.3 | 83.4 | 56.2 |
| 58 | 82.7 | 65.1 | 81.9 | 59.4 |
| 59 | 80.1 | 67.4 | 79.2 | 61.5 |
| 60 | 76.1 | 70.2 | 75.6 | 64.5 |
| 61 | 71.8 | 73.7 | 71.4 | 68.2 |
| 62 | 67.6 | 76.5 | 67.6 | 72.2 |
| 63 | 62.0 | 79.2 | 62.4 | 75.3 |
| 64 | 56.5 | 82.4 | 56.7 | 79.5 |
| 65 | 50.9 | 86.3 | 50.4 | 83.2 |
| 66 | 44.0 | 89.1 | 44.0 | 86.2 |
| 67 | 37.1 | 91.4 | 37.2 | 89.0 |
| 68 | 28.5 | 92.9 | 28.2 | 91.3 |
| 69 | 19.8 | 95.2 | 19.9 | 93.9 |
| 70 | 12.6 | 96.8 | 12.7 | 95.7 |
BSES-SF, breastfeeding self-efficacy scale-short form; EBF, exclusive breastfeeding; Sen, sensitivity; Spe, specificity.
The BSES-SF score found in our study (59.76 points) was above the scores reported in other studies conducted in Spain. In the validation study conducted by Oliver-Roig et al., the mean score in the BSES-SF was 51.94 points,22 while Marco-Alegría et al. reported a mean of 50.03 points.25 In these studies, the BSES-SF was administered in the maternity ward before day 5 post birth. This may explain the observed differences, as in the LAyDI study, mothers completed the BSES-SF on day 10 post birth, when they had been breastfeeding longer and presumably felt more competent. Ideally, the initial newborn evaluation in primary care centres should take place 48–72 h after discharge.26 The results of our study suggest that the time elapsed between both care settings (maternity ward and primary care centre) is longer than recommended, which poses a risk to infant health and may contribute to early BF discontinuation.26
Studies conducted in other countries have produced heterogeneous results, with the lowest scores found in Asian countries (where the prevalence of BF is substantially lower): 47.3 points China19 and 42.39 points in Japan.27 In other European countries, scores are similar to those in our study: 54.8 points in Italy,18 57.4 in Sweden15 and 63.6 in Portugal.21 Therefore, the scores obtained in the scale seem to be associated with the prevalence of BF in the region where self-efficacy is being assessed.
The BSES-SF performed adequately for prediction of BF maintenance. Some studies have found that the scale offers a good predictive power through 3 months post birth,17,18,23,27 compared to 1 month in others.19,22 In our study, the BSES-SF exhibited a good predictive power through 2 months post birth in mothers that breastfed exclusively. We did not find any studies that analysed the predictive power of the scale differentiating between mothers that practiced exclusive BF and mothers that practiced mixed feeding. Given the substantial differences we observed in the BSES-SF scores between these 2 groups of mothers, we thought it would be prudent to make a separate analysis for each. Based on the results, the scale does not seem to be a good predictor in the case of mixed feeding.
As for the optimal cut-off point in the BSES-SF, a similar study estimated a cut-off score of 50 points.27 However, this study was conducted in the Asian population, in which BF trends, as we mentioned above, are very different compared to Western countries. Considering that for the purpose of prediction the cut-off point should be selected with the aim of detecting the highest possible number of mothers at risk of BF discontinuation, we decided to use the sensitivity as the parameter used to select the optimal cut-off value. The ultimate purpose of identifying mothers at risk of discontinuing BF is to offer increased BF support.4 We arbitrarily selected a minimum sensitivity of 80% to define adequate predictive power, although any other of the values presented in Table 2 could be applied. Thus, we propose using a cut-off score of 58 points, as it offers a sensitivity greater than 80% in the 2 age groups in which we calculated the threshold.
Most studies on scales used for assessment of BF have been made in the hospital setting and in the first days post birth.5,18–22,27 We only found one study conducted in the primary care setting that used the BSES-SF to assess factors that affect BF.24 Our analysis revealed that the application of scales in the primary care setting to predict BF outcomes can be useful. The BSES-SF is completed in a short time and can be administered in the first visit of newborn infants that are exclusively breastfed. However, the best approach would be to implement follow-up plans developed and implemented by hospital maternity departments in collaboration with primary care services.6 Breastfeeding assessment data collected in hospital should reach the primary care system, ensuring continuity of care. The best way to convey this information would be through standardised instruments6 like the BSES-SF or scales used to assess observed feeds.8
One of the limitations of this study was the loss to follow-up of some patients, a common limitation of longitudinal studies that also affected the LAyDI project. Although 17.4% of the initial sample did not complete the follow-up, the number of participants that continued in the study at 6 months post birth was greater than the estimated minimum necessary sample size. Thus, although there were losses to follow-up, the results are still valid. On the other hand, since we analysed secondary data, we did not perform a sample size calculation specifically for our study. As a result, there were considerable differences between the participants in the 2 feeding modality groups that we analysed separately (exclusive BF and mixed feeding). Nevertheless, due to its substantial size, the sample yielded BSES-SF scores representative of the population despite the disparities between the feeding modality groups.
Due to all of the above, we conclude that the BSES-SF is a useful instrument at the primary care level to identify mothers at risk of discontinuing BF before 2 months post birth. Mothers with scores of 58 points or lower should receive additional BF support.
FundingThe LAyDI study was awarded one of the research grants of the Asociación Española de Pediatría de Atención Primaria-Fundación Pediatría y Salud (AEPap-FPS) in 2017.
Conflicts of interestThe authors have no conflicts of interest to declare.
Abad-Balaguer B., AcitoresSuz E., Acosta-Navas B., Aguilera-López L., Albaladejo- Beltrán S., Albañil-Ballesteros M.R., Alcaraz-Quiñonero M., Álvarez-Bueno E., Angulo-Moreno M.E., Anllo-Lago J., Aparicio-Rodrigo M., Arana-Cañedo-Argüelles C., Arranz-Sanjuan R., Arroyo-Úbeda R., Asensi-Monzo M.T., Astiz-Blanco M.I., Azor-Martínez E., Baliela-García B.C., Barea-García J.J., Barrios-González E.M., Batalla-Fadó L., Bejarano-López M.A., Belda-García M.T., Benítez-Rubio M.R., Bercedo-Sanz A., BernadUsoz J.V., Biosca-Pàmies M., Blesa-Baviera L.C., Bombín-Granado J.M., Bonet-Garrosa A., Botella-Serrano B., Bravo-Acuña J., Bretón-Peña A.I., Burgaleta-Sagaseta A.M., Calvo-Lorenzo M.T., Canadell-Villaret D., Carballal-Mariño M., Carmona-Cedrés N., Carrera-Polanco M., Carretero-Carretero L., Casado-Sánchez M.L., Casares-Alonso I., Castillo-Marcalain A., CaubetBusquet I., Cayuela-Guerrero C., Coto-Fuente M.M., Cruz-Navarro I., De Haro-López M.A., De La Serna-Higuera P.M., Del Castillos-Aguas G., Del Toro-Calero C., Diaz-Cirujano A.I., Díaz-Pedrouzo A., Díez-Zaera O., Duelo-Marcos M., Edo-Jimeno M.J., Elorz-Ibáñez A.C., Escanciano- García Y., Escribano-Romero M.J., Esparza-Olcina M.J., Espinazo-Ramos O., Espínola-Docio B., Esquivel-Ojeda J.N., Fabregat-Ferrer E., Fernández-Francés M., Fernández-León A., Fernández-López F.J., Fernández-Pastor F., Fernández-Rodríguez M., Fernández-Segura M.E., Ferrándiz-Cerdá B., Flores-Erro U., Galán-Calvo M.J., Galán-Rico J., Galardi-Andonegui M.S., Garach-Gómez., García-Arroyo I., García- Lara G.M., García-Mérida M.J., García-Merino A., García-Rebollar C.A., García- Santiago M., García-Onieva-Artázcoz M., García-Vera C., Garnelo-Suarez L., Garrido- Redondo M., Gatell-Carbo A., Gil-Alexandres I., Giribet-Folch M., Gómez-Casares R., Gómez-Sorrigueta P., González-Marcos M.I., González-Rodríguez M.P., Gracia-Alfonso M.A., Grau-García A.I., Gutiérrez-Abad C., Heras-Galindo J.A., Hernández- Ortiz M.Y., Hernando-Helguero P., Herrero-Rey S., Iribarren-Udobro I., Jaramillo- Hidalgo D., Jiménez-Alés R., Jiménez-Hereza J.M., Jové-Naval J., Juanes-De Toledo B., Ledesma-Albarrán J.M., Lobera-Navaz P., López-Alonso R., López-Vilar P., Lorente-García-Mauriño A.M., Manero-Oteiza A., Marco-Puche A., Marfil-Olink S., Márquez-Moreno M.D., Martín-Carballo G., Martín-Cuesta B., Martín-Ibáñez I., Martín-Peinador Y., Martín-Rial S., Martínez-Espligares L., Martínez-Moral N., Martínez-Rubio M.V., Martínez-Ruiz M.M., Menéndez-Bada T., Menéndez-González N., Mengual-Gil J., Merino-Villeneuve I., Mínguez-Verdejo R., Miranda- Berrioategortua I., Moneo-Hernández I., Monje C., Montañés-Sánchez A.M., Montes- Peña M., Montoro-Romero M.S., Monzón-Bueno A.I., Morell-Bernabé J.J., Muñoz- García N.P., Muñoz-Hiraldo M.E., Mustieles-Moreno C., Navarro-Cabañas G., Navas- Heredia C.M., Nóvoa-García E., Oliva-Alfonso A., Olmos-García J.M., Ordoñez- Alonso M.A., Padilla-Esteban M.L., Padilla-Sánchez M.C., Palomares-Gimeno M.J., Palomino-Urda N., Panizo-Santos M.B., Parejo-Carranza R., Pavía-Lafuente M., Pavo- García M.R., PeixSambola M.A., PeñarrojaPeirats S., Pérez-Candás J.I., Pérez-de Saracho-Taramona M., Pérez-Gavilán J., Puig-García C., Puyuelo-Del Val P., Quintanilla Sánchez MM, Ramos Zugasti M, Rey Del Castillo C, Ribera Sirvent C, Ripoll-Lozano A., Rivas-Abraldes N., Riveros-Huckstadt M.P., Robles-García J., Rodríguez-Delgado J., Rodríguez-Fernández M.M., Rodríguez-Fernández-Oliva C.R., Rodríguez-Pérez E.G., Rodríguez-Santana Y., Rodríguez-López-Márquez G.A., Rodríguez-Salinas-Pérez E., Rojo-Portolés P., Rubio-Remiro O., Ruiz-Chércoles E., Sáenz-de Urturi-Sánchez A., Sáez-de Lafuente-Arriazu A., Salcedo-Pacheco I., Sánchez-Andrés M.T., Sánchez-Calderón M., Sánchez-Cordero N., Sánchez-Echenique M., Sánchez-Fuentes V., Sánchez-González B., Sánchez-Jiménez M.C., Sánchez-Pina C., Sánchez-Precioso S., Sánchez-Prieto E.I., Sancho-Madrid B., Satrústegui-Gamboa F., Serna-Saugar M.C., Servera-Ginard C.I., Suárez-Vicent E., Surribas-Murillo C., Torres-Álvarez-de Arcaya M.L., Valerio-Hernández E., Vaquerizo-Pollino M.J., Vega- Pérez M.S., Velasco-Guijarro O., Viar-Urieta M., Villafruela-Álvarez C., Villaizán- Pérez C., Viver-Gómez S.
Please cite this article as: Balaguer-Martínez JV, García-Pérez R, Gallego-Iborra A, Sánchez-Almeida E, Sánchez-Díaz MD, Ciriza-Barea E. Capacidad predictiva para la lactancia y determinación del mejor punto de corte de la escala BSES-SF. An Pediatr. 2022;96:51–58.
Previous presentation: the results of this study were presented at the 17th Congress of the AEPap, February 13–15, 2020, Madrid, Spain.