A boy aged 11 years, correctly vaccinated, was admitted to the paediatric intensive care unit due to hearing loss, sore throat, low-grade fever, decreased level of consciousness and lumbar pain of 3 days duration. The blood panel revealed elevation of acute phase reactants, the computed tomography scan was normal and testing of a lumbar puncture specimen was positive for Streptococcus pyogenes, prompting initiation of treatment with cefotaxime, clindamycin and dexamethasone. The screening for immunodeficiency disorders was negative. An external ventricular drain was placed on account of the presence of manifestations suggestive of increased intracranial pressure, evincing intracranial blood pressure values of 30 mmHg.
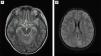
Given the poor response, a magnetic resonance (MR) scan was requested (Fig. 1A) that showed signs of infratentorial meningitis (Fig. 1B), generalised ventriculitis and supratentorial ischaemic encephalitis. At 5 days, once symptoms had improved, the patient was extubated and exhibited flaccid paraparesis with absent reflexes and numbness and cauda equina syndrome. The MRI of the scan was compatible with transverse myelitis1 (Fig. 2A) and evinced the presence of purulent material in the thecal sac with cauda equina radiculitis2 and arachnoiditis (Fig. 2B).
T2-weighted MRI of the brain, horizontal view, showing: (A) Abnormal signal intensity of sulci at supratentorial level. (B) Abnormal signal intensity with pathological restriction of the ependyma of both occipital horns and the third ventricle and mild restriction of the ependyma of the fourth ventricle, with purulent material at the downward slope of both occipital horns.
Spinal cord involvement suggested (A) acute transverse myelitis (longitudinal extensive involvement with T2 hyperintensity over more than 2/3 of the cord thickness), associated with (B) inflammatory-infectious radiculitis of the cauda equina and purulent material at the distal declive portion.
An immune disorder was suspected, so immunoglobulin3 and megadose steroid boluses were administered 12 days after admission, which achieved a good response: improvement of hearing loss, increased mobility and resolution of fever. The patient was referred to an intensive rehabilitation unit. At 6 months, the remaining sequelae are neurogenic bladder and bowel.
FundingThis research did not receive any external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.