Asthma is a common chronic disease in the paediatric age group that requires close follow-up. Clinical practice guidelines offer evidence-based recommendations to achieve adequate control of the disease.
ObjectiveTo assess the management of childhood asthma in the primary care setting in the Community of Madrid, and the adherence of health care professionals to guideline recommendations. To analyse the association of asthma management with age, the socioeconomic level of the catchment population and the workload of primary care centres.
Methodsretrospective longitudinal study in patients aged 6–14 years newly diagnosed with asthma in primary care centres of the Community of Madrid in 2021. We analysed sociodemographic and clinical variables and the compliance with recommendations at the time of diagnosis and over 1 year of follow-up. The source of data was the electronic health record database of the primary care system.
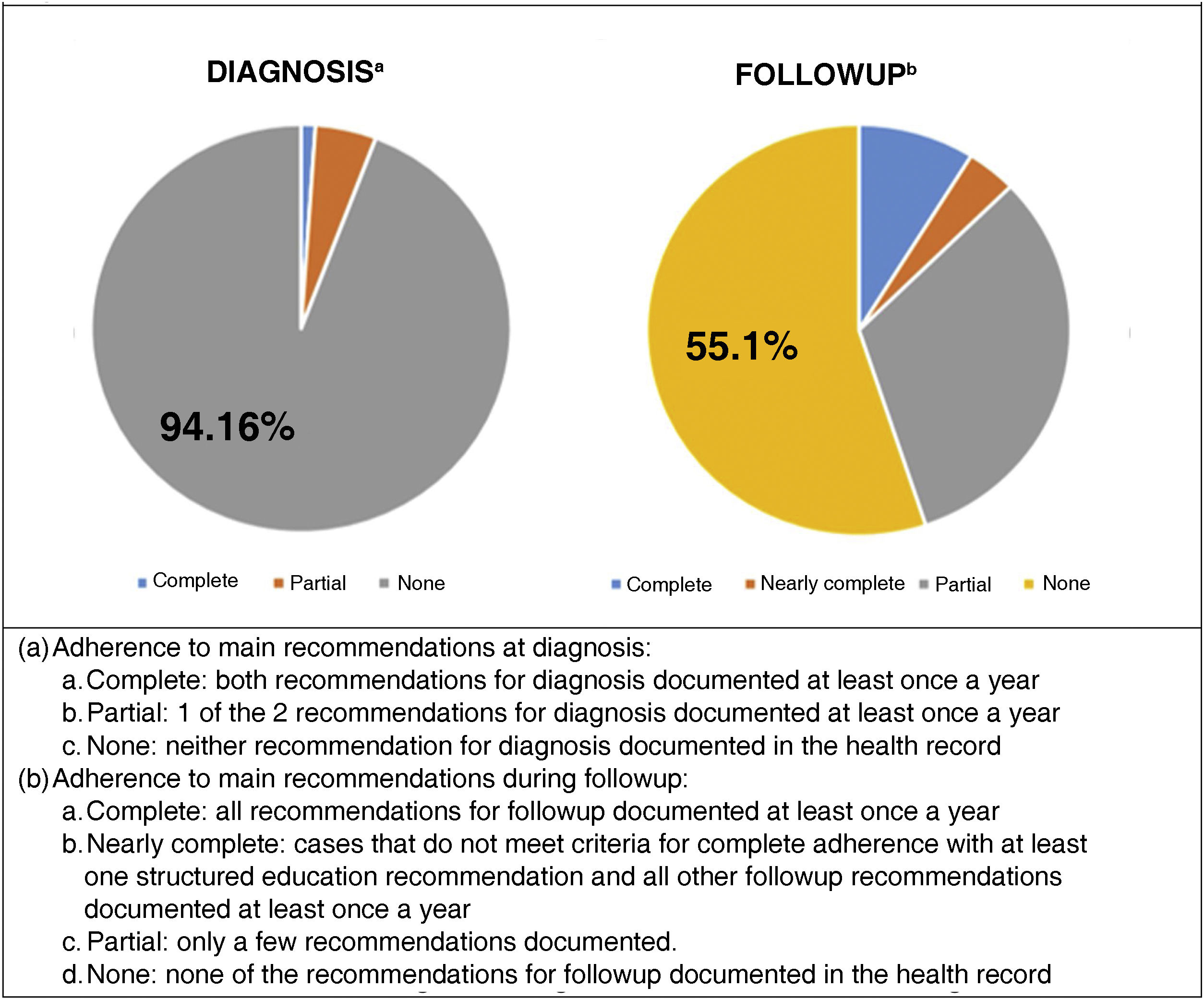
ResultsWe found a proportion of compliance with the recommendations upon diagnosis of the disease of 5.84%, with differences associated to the socioeconomic level of the catchment population (P = .033), and the pressure of care (P = .006). The proportion of compliance with recommendations during follow-up was 12.73%, with differences based on age (P = .01), socioeconomic level (P = 0.006) and centre workloads (P = .002).
ConclusionsCompliance with the recommendations of the main childhood asthma management guidelines in the primary care setting was low in the Community of Madrid. Strategies need to be implemented to improve the management of this disease and the adherence of professionals to the protocols developed for this purpose.
El asma es una enfermedad crónica frecuente en la edad pediátrica y precisa un seguimiento estrecho. Para lograr un buen control de la enfermedad las Guías de Práctica Clínica ofrecen recomendaciones basadas en la evidencia científica.
ObjetivoValorar el manejo del asma que se realiza en Atención Primaria de la Comunidad de Madrid, y la adecuación a las recomendaciones de las guías por parte de los profesionales sanitarios. Analizar la relación del manejo con la edad, el nivel socioeconómico de la población y la presión asistencial de los centros de salud.
MétodosEstudio longitudinal retrospectivo en pacientes de 6 a 14 años con un nuevo diagnóstico de asma durante el año 2021 en los centros de salud de la Comunidad de Madrid. Se analizaron variables sociodemográficas, clínicas y el cumplimiento de las recomendaciones al diagnóstico y durante un año de seguimiento. La fuente de información fue la Historia Clínica Electrónica para Atención Primaria.
ResultadosEl cumplimiento de las recomendaciones al diagnóstico de la enfermedad fue del 5,84%, con diferencias según el nivel socioeconómico (p = 0,033) y la presión asistencial (p = 0,006). El cumplimiento de las recomendaciones durante el seguimiento fue del 12,73%, con diferencias según la edad (p = 0,01), nivel socioeconómico (p = 0,006) y la presión asistencial (p = 0,002).
ConclusionesEl cumplimiento registrado de las recomendaciones sobre el manejo del asma en Atención Primaria de la Comunidad de Madrid es bajo. Es necesario fomentar estrategias para mejorar el manejo de esta enfermedad y, la adhesión de los profesionales a los programas diseñados para ello.
Child and adolescent asthma is an important public health problem1 on account of its high prevalence2–4 and high associated health care costs.1 Daily living limitations and school absenteeism in patients and lost workdays in caregivers have a significant impact on the quality of life of affected children and their families.2,5
Asthma is a heterogeneous disease whose clinical presentation can change over time and that affects different patients differently, so it requires evaluation at regular intervals.5 The main goal of treatment is to achieve adequate disease control for the patient to be able to live without limitations.4,6–8 However, it is estimated that fewer than 50% of patients maintain adequate asthma control.5,6 Patient education and follow-up are essential,3 and primary care (PC) paediatricians are the professionals in the ideal position to provide them.1
Clinical practice guidelines (CPGs) have been developed to offer evidence-based recommendations for diagnosis and treatment.1 The main reference at the global level is the Global Strategy for Asthma Management and Prevention of the Global Initiative for Asthma (GINA),9 while the chief guideline is Spain is the Guía Española para el Manejo del Asma (GEMA, Spanish Guideline for the Management of Asthma), developed through the collaboration of all professional collectives involved in asthma care.10
Health care in Spain falls under the authority of the regional governments of autonomous communities. Since 2002, paediatric asthma care protocols and programmes have been developed adapting the recommendations of CPGs to the resources available in each autonomous community.1,11 However, there is concern that the adherence to recommendations and care protocols on the part of PC paediatricians is poorer than would be desired. Possible contributing factors include the excessive workloads of health care professionals, socioeconomic inequalities in the population and the profile of patients, giving rise to heterogeneity in clinical practice and suboptimal care delivery. In the Community of Madrid, paediatric asthma care was included among the health care service portfolio of the public health system in 2007.12 The latest update to the service portfolio, from 2021, includes an asthma care protocol integrated in the electronic health record (EHR) system to allow easy documentation in the patient’s chart.13 It includes quality indicators as an objective means to assess the quality of delivered care and the adherence to official practice guidelines.14,15
The aim of our study was to describe the management of patients with asthma newly diagnosed in 2021 in the primary care system of the Community of Madrid and the degree of adherence of PC paediatricians to the recommendations of current CPGs during the study period16,17 based on the data recorded in the paediatric asthma care protocol integrated in the regional EHR system. We analysed the association of the adherence to recommendations with patient age, the socioeconomic level of the catchment population and the workload of PC centres.
MethodsDesign: Retrospective longitudinal descriptive study.
Setting: Two hundred and sixty PC centres of the Madrid public health system that managed paediatric patients.
Source of data. Data were retrieved from the centralised, unified primary care electronic health records system of the Community of Madrid (AP-Madrid). Technical Directorate of Health Care Information Systems of the Primary Care Administration of the Community of Madrid provided the anonymised data.
Sample. Patients with a new diagnosis of asthma received in 2021, documented in the EHR with code R96 (asthma) of the International Classification of Primary Care, 2nd Edition (ICPC-2), aged 6–14 years, who underwent a follow-up evaluation at least once in 2022. We excluded patients who received a diagnosis of asthma before 2021.
The follow-up period in the study ranged from the date of diagnosis in 2021 to up to December 31, 2022 (minimum of 1 year of follow-up).
Study variablesSociodemographic variables- •
Sex and age
- •
Socioeconomic status (SES): assessed by means of the deprivation index (DI) assigned to each primary care centre, calculate based on 5 indicators: educational attainment, quality of residence, demographics, culture and employment. The sample was classified in four groups based in the quartile distribution (DI <25th percentile to DI >75th percentile, with higher percentiles indicating a lower SES).18
- •
Workload of primary care centre: the patient volume was calculated with the following formula: number of patients managed in paediatric primary care clinic per year/ number of paediatricians in the centre × total workdays in the year in 2022, which was the year that comprehended most of the follow-up of the patients.
Variables included in the asthma care protocol integrated in the EHR system.13 In the case more than one value had been entered for a variable in the EHR, we collected the most recent value for the analysis:
- •
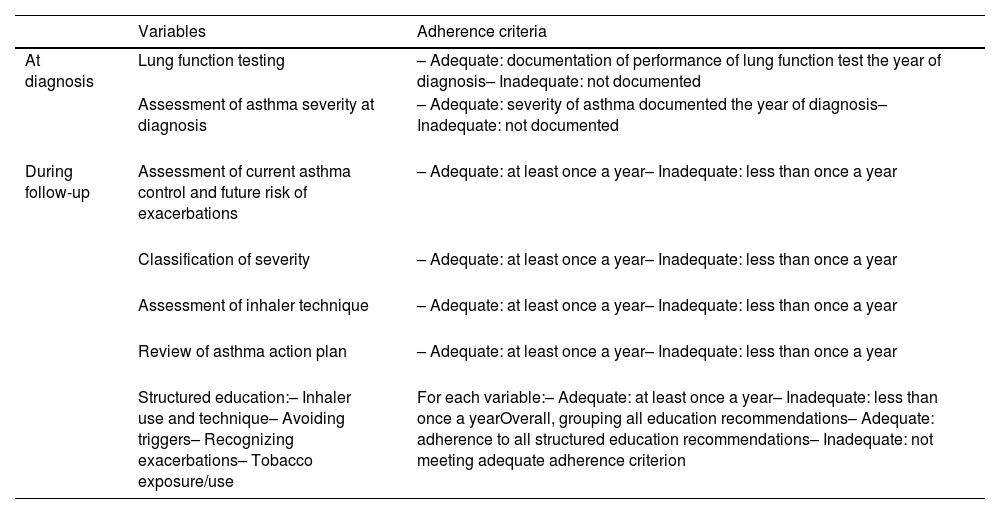
Adherence of health care providers to the recommendations in the GEMA16 and GINA guidelines17 based on the indicators listed in Table 1.
Table 1.Variables and criteria used to determine adherence to recommendationsa.
Variables Adherence criteria At diagnosis Lung function testing – Adequate: documentation of performance of lung function test the year of diagnosis– Inadequate: not documented Assessment of asthma severity at diagnosis – Adequate: severity of asthma documented the year of diagnosis– Inadequate: not documented During follow-up Assessment of current asthma control and future risk of exacerbations – Adequate: at least once a year– Inadequate: less than once a year Classification of severity – Adequate: at least once a year– Inadequate: less than once a year Assessment of inhaler technique – Adequate: at least once a year– Inadequate: less than once a year Review of asthma action plan – Adequate: at least once a year– Inadequate: less than once a year Structured education:– Inhaler use and technique– Avoiding triggers– Recognizing exacerbations– Tobacco exposure/use For each variable:– Adequate: at least once a year– Inadequate: less than once a yearOverall, grouping all education recommendations– Adequate: adherence to all structured education recommendations– Inadequate: not meeting adequate adherence criterion - •
Classification of asthma severity based on the GEMA guideline version 4.4,19 included in the 2021 asthma care protocol of the Community of Madrid.
- •
Level of control based on the results in the Spanish questionnaire for assessment of asthma control in children (Control del Asma en Niños [CAN]).20
- •
Impact of asthma on daily living, presence of symptoms between exacerbations, limitations to physical activity and/or impact on sleep.
- •
Exacerbations, emergency department visits and hospitalizations during the follow-up.
Quantitative data were summarised as mean and standard deviation (SD) and qualitative data as absolute frequency and percentage distributions.
We used the χ2 test to compare clinical and sociodemographic variables based on sex, age group and SES (all variables followed a normal distribution).
To compare the adherence to recommendations based on age and SES, we carried out univariate logistic regression analyses; and to compare it in terms of patient volume, we used the Student t test or analysis of variance depending on the number of categories.
We calculated crude incidence rates per 1000 inhabitants/year, overall, by sex and by age group, using the number of cases in the numerator and the population size (number of active health care card holders for the year under study) in the denominator, along with the corresponding 95% confidence intervals (CIs).
Ethical and legal aspectsThe study was approved by the Research Ethics Committee of the Hospital 12 de Octubre of Madrid and received a favourable evaluation from the Central Research Committee of the Primary Health Care Administration of Madrid. All the collected data were anonymised.
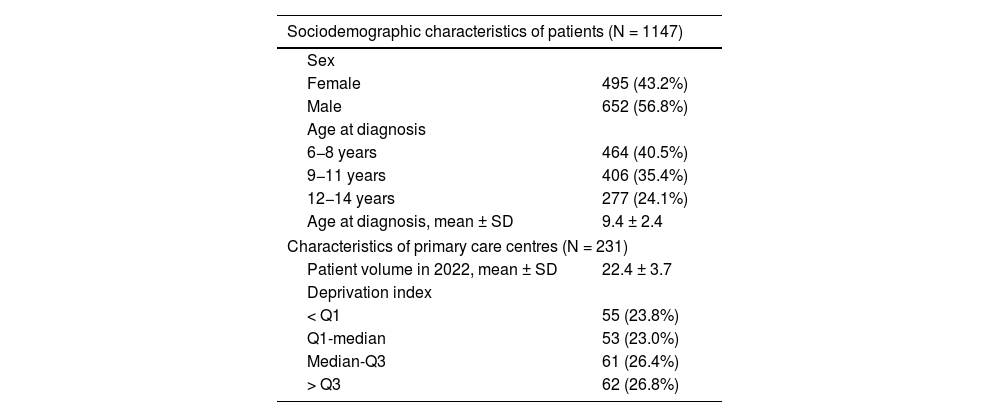
ResultsThe study included 1147 patients aged 6–14 years with asthma newly diagnosed in 2021 (Table 2).
Description of study sample.
| Sociodemographic characteristics of patients (N = 1147) | |
|---|---|
| Sex | |
| Female | 495 (43.2%) |
| Male | 652 (56.8%) |
| Age at diagnosis | |
| 6−8 years | 464 (40.5%) |
| 9−11 years | 406 (35.4%) |
| 12−14 years | 277 (24.1%) |
| Age at diagnosis, mean ± SD | 9.4 ± 2.4 |
| Characteristics of primary care centres (N = 231) | |
| Patient volume in 2022, mean ± SD | 22.4 ± 3.7 |
| Deprivation index | |
| < Q1 | 55 (23.8%) |
| Q1-median | 53 (23.0%) |
| Median-Q3 | 61 (26.4%) |
| > Q3 | 62 (26.8%) |
Q1, first quartile; Q3, third quartile; SD, standard deviation.
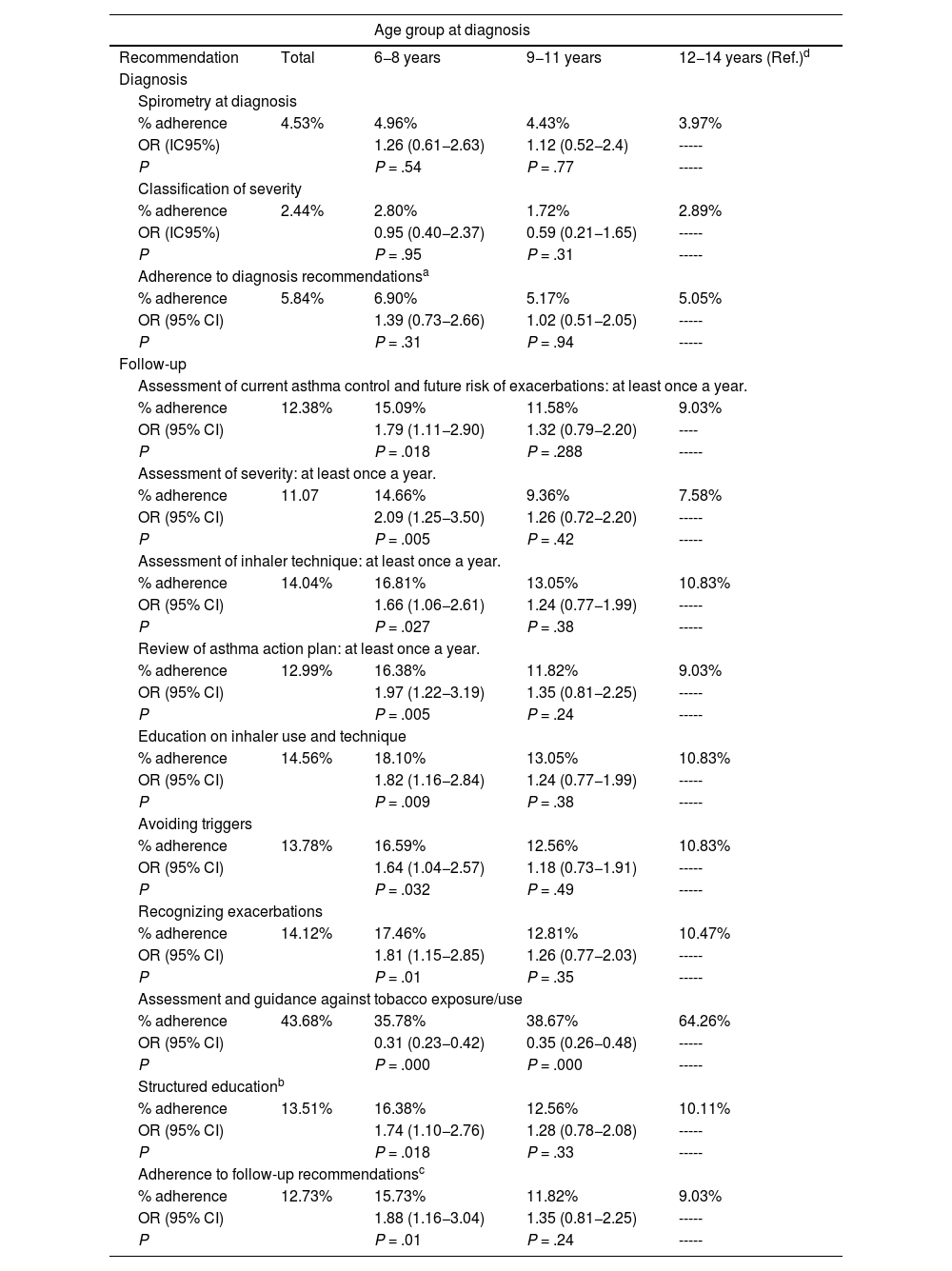
Fig. 1 shows the overall adherence to the analysed diagnosis and follow-up recommendations. Tables 3 and 4 present the results on adherence by age group and SES, respectively. We calculated odds ratios (ORs) with the corresponding 95% confidence intervals (CIs), and the reference group was the oldest age group in Table 3 and the most disadvantaged SES group (deprivation index > 75th percentile) in Table 4.
Adherence to recommendations by patient age.
| Age group at diagnosis | ||||
|---|---|---|---|---|
| Recommendation | Total | 6−8 years | 9−11 years | 12−14 years (Ref.)d |
| Diagnosis | ||||
| Spirometry at diagnosis | ||||
| % adherence | 4.53% | 4.96% | 4.43% | 3.97% |
| OR (IC95%) | 1.26 (0.61−2.63) | 1.12 (0.52−2.4) | ----- | |
| P | P = .54 | P = .77 | ----- | |
| Classification of severity | ||||
| % adherence | 2.44% | 2.80% | 1.72% | 2.89% |
| OR (IC95%) | 0.95 (0.40−2.37) | 0.59 (0.21−1.65) | ----- | |
| P | P = .95 | P = .31 | ----- | |
| Adherence to diagnosis recommendationsa | ||||
| % adherence | 5.84% | 6.90% | 5.17% | 5.05% |
| OR (95% CI) | 1.39 (0.73−2.66) | 1.02 (0.51−2.05) | ----- | |
| P | P = .31 | P = .94 | ----- | |
| Follow-up | ||||
| Assessment of current asthma control and future risk of exacerbations: at least once a year. | ||||
| % adherence | 12.38% | 15.09% | 11.58% | 9.03% |
| OR (95% CI) | 1.79 (1.11−2.90) | 1.32 (0.79−2.20) | ---- | |
| P | P = .018 | P = .288 | ----- | |
| Assessment of severity: at least once a year. | ||||
| % adherence | 11.07 | 14.66% | 9.36% | 7.58% |
| OR (95% CI) | 2.09 (1.25−3.50) | 1.26 (0.72−2.20) | ----- | |
| P | P = .005 | P = .42 | ----- | |
| Assessment of inhaler technique: at least once a year. | ||||
| % adherence | 14.04% | 16.81% | 13.05% | 10.83% |
| OR (95% CI) | 1.66 (1.06−2.61) | 1.24 (0.77−1.99) | ----- | |
| P | P = .027 | P = .38 | ----- | |
| Review of asthma action plan: at least once a year. | ||||
| % adherence | 12.99% | 16.38% | 11.82% | 9.03% |
| OR (95% CI) | 1.97 (1.22−3.19) | 1.35 (0.81−2.25) | ----- | |
| P | P = .005 | P = .24 | ----- | |
| Education on inhaler use and technique | ||||
| % adherence | 14.56% | 18.10% | 13.05% | 10.83% |
| OR (95% CI) | 1.82 (1.16−2.84) | 1.24 (0.77−1.99) | ----- | |
| P | P = .009 | P = .38 | ----- | |
| Avoiding triggers | ||||
| % adherence | 13.78% | 16.59% | 12.56% | 10.83% |
| OR (95% CI) | 1.64 (1.04−2.57) | 1.18 (0.73−1.91) | ----- | |
| P | P = .032 | P = .49 | ----- | |
| Recognizing exacerbations | ||||
| % adherence | 14.12% | 17.46% | 12.81% | 10.47% |
| OR (95% CI) | 1.81 (1.15−2.85) | 1.26 (0.77−2.03) | ----- | |
| P | P = .01 | P = .35 | ----- | |
| Assessment and guidance against tobacco exposure/use | ||||
| % adherence | 43.68% | 35.78% | 38.67% | 64.26% |
| OR (95% CI) | 0.31 (0.23−0.42) | 0.35 (0.26−0.48) | ----- | |
| P | P = .000 | P = .000 | ----- | |
| Structured educationb | ||||
| % adherence | 13.51% | 16.38% | 12.56% | 10.11% |
| OR (95% CI) | 1.74 (1.10−2.76) | 1.28 (0.78−2.08) | ----- | |
| P | P = .018 | P = .33 | ----- | |
| Adherence to follow-up recommendationsc | ||||
| % adherence | 12.73% | 15.73% | 11.82% | 9.03% |
| OR (95% CI) | 1.88 (1.16−3.04) | 1.35 (0.81−2.25) | ----- | |
| P | P = .01 | P = .24 | ----- | |
CI, confidence interval; OR, odds ratio.
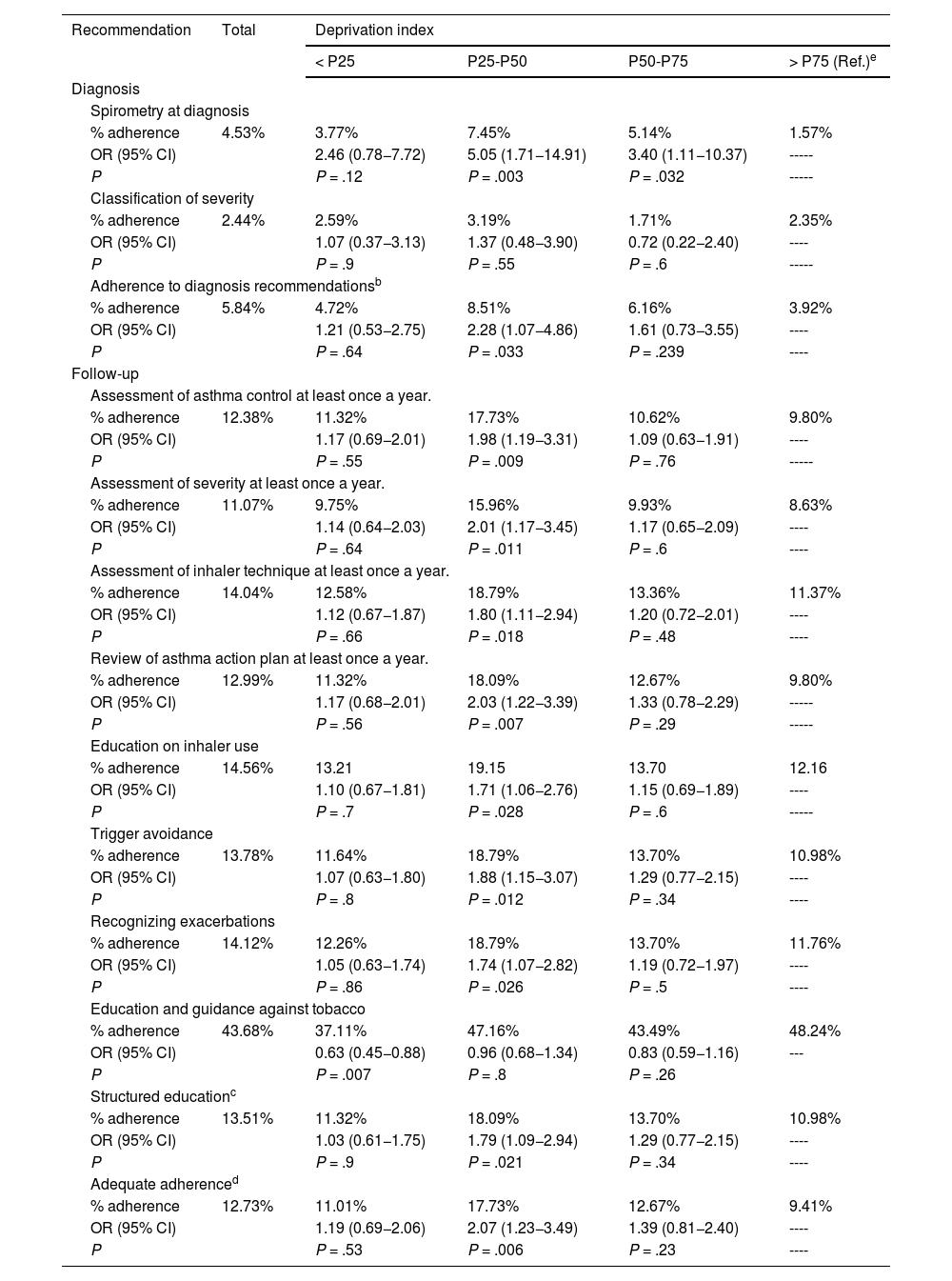
Adherence to recommendations based on deprivation indexa.
| Recommendation | Total | Deprivation index | |||
|---|---|---|---|---|---|
| < P25 | P25-P50 | P50-P75 | > P75 (Ref.)e | ||
| Diagnosis | |||||
| Spirometry at diagnosis | |||||
| % adherence | 4.53% | 3.77% | 7.45% | 5.14% | 1.57% |
| OR (95% CI) | 2.46 (0.78−7.72) | 5.05 (1.71−14.91) | 3.40 (1.11−10.37) | ----- | |
| P | P = .12 | P = .003 | P = .032 | ----- | |
| Classification of severity | |||||
| % adherence | 2.44% | 2.59% | 3.19% | 1.71% | 2.35% |
| OR (95% CI) | 1.07 (0.37−3.13) | 1.37 (0.48−3.90) | 0.72 (0.22−2.40) | ---- | |
| P | P = .9 | P = .55 | P = .6 | ----- | |
| Adherence to diagnosis recommendationsb | |||||
| % adherence | 5.84% | 4.72% | 8.51% | 6.16% | 3.92% |
| OR (95% CI) | 1.21 (0.53−2.75) | 2.28 (1.07−4.86) | 1.61 (0.73−3.55) | ---- | |
| P | P = .64 | P = .033 | P = .239 | ---- | |
| Follow-up | |||||
| Assessment of asthma control at least once a year. | |||||
| % adherence | 12.38% | 11.32% | 17.73% | 10.62% | 9.80% |
| OR (95% CI) | 1.17 (0.69−2.01) | 1.98 (1.19−3.31) | 1.09 (0.63−1.91) | ---- | |
| P | P = .55 | P = .009 | P = .76 | ----- | |
| Assessment of severity at least once a year. | |||||
| % adherence | 11.07% | 9.75% | 15.96% | 9.93% | 8.63% |
| OR (95% CI) | 1.14 (0.64−2.03) | 2.01 (1.17−3.45) | 1.17 (0.65−2.09) | ---- | |
| P | P = .64 | P = .011 | P = .6 | ---- | |
| Assessment of inhaler technique at least once a year. | |||||
| % adherence | 14.04% | 12.58% | 18.79% | 13.36% | 11.37% |
| OR (95% CI) | 1.12 (0.67−1.87) | 1.80 (1.11−2.94) | 1.20 (0.72−2.01) | ---- | |
| P | P = .66 | P = .018 | P = .48 | ---- | |
| Review of asthma action plan at least once a year. | |||||
| % adherence | 12.99% | 11.32% | 18.09% | 12.67% | 9.80% |
| OR (95% CI) | 1.17 (0.68−2.01) | 2.03 (1.22−3.39) | 1.33 (0.78−2.29) | ----- | |
| P | P = .56 | P = .007 | P = .29 | ----- | |
| Education on inhaler use | |||||
| % adherence | 14.56% | 13.21 | 19.15 | 13.70 | 12.16 |
| OR (95% CI) | 1.10 (0.67−1.81) | 1.71 (1.06−2.76) | 1.15 (0.69−1.89) | ---- | |
| P | P = .7 | P = .028 | P = .6 | ----- | |
| Trigger avoidance | |||||
| % adherence | 13.78% | 11.64% | 18.79% | 13.70% | 10.98% |
| OR (95% CI) | 1.07 (0.63−1.80) | 1.88 (1.15−3.07) | 1.29 (0.77−2.15) | ---- | |
| P | P = .8 | P = .012 | P = .34 | ---- | |
| Recognizing exacerbations | |||||
| % adherence | 14.12% | 12.26% | 18.79% | 13.70% | 11.76% |
| OR (95% CI) | 1.05 (0.63−1.74) | 1.74 (1.07−2.82) | 1.19 (0.72−1.97) | ---- | |
| P | P = .86 | P = .026 | P = .5 | ---- | |
| Education and guidance against tobacco | |||||
| % adherence | 43.68% | 37.11% | 47.16% | 43.49% | 48.24% |
| OR (95% CI) | 0.63 (0.45−0.88) | 0.96 (0.68−1.34) | 0.83 (0.59−1.16) | --- | |
| P | P = .007 | P = .8 | P = .26 | ||
| Structured educationc | |||||
| % adherence | 13.51% | 11.32% | 18.09% | 13.70% | 10.98% |
| OR (95% CI) | 1.03 (0.61−1.75) | 1.79 (1.09−2.94) | 1.29 (0.77−2.15) | ---- | |
| P | P = .9 | P = .021 | P = .34 | ---- | |
| Adequate adherenced | |||||
| % adherence | 12.73% | 11.01% | 17.73% | 12.67% | 9.41% |
| OR (95% CI) | 1.19 (0.69−2.06) | 2.07 (1.23−3.49) | 1.39 (0.81−2.40) | ---- | |
| P | P = .53 | P = .006 | P = .23 | ---- | |
CI, confidence interval; OR, odds ratio. P25, P50, P75: 25th, 50th and 75th percentiles in the deprivation index distribution.
The deprivation index divides the population in four groups based on socioeconomic status, so that the group below P25 has the highest socioeconomic status and the group above P75 the lowest.
Considered adequate when performance of spirometry and/or assessment of asthma severity at diagnosis documented in health record.
In 94.2% of the sample, none of the actions recommended for diagnosis had been documented, with no differences based on age group. Based on SES, centres in areas with a deprivation index between the 25th and 50th percentiles exhibited significantly greater adherence overall (P = .03; OR, 2.28; 95% CI, 1.07−4.86) (Table 4).
The mean patient volume was 19.81 patients/day (SD, 3.39) in the full adherence group compared to 22.63 patients/day (SD, 3.65) in the partial or absent adherence group (P = .006; mean difference, 2.82; 95% CI, 0.83–4.82).
Adherence to follow-up recommendationsIn 44.9% of the patients, the EHR included documentation of one or more of the interventions recommended during follow-up, most frequently guidance for prevention of tobacco use or exposure (43.7%).
We found significant differences based on age and SES on the adherence to recommendations overall and on the adherence to most of the individual recommendations under study (Tables 3 and 4).
The percentage of adherence to recommendations was significantly greater for the younger age group, with the exception of guidance against tobacco, which was documented in a greater proportion of patients aged 12−14 years.
Based on SES, the overall adherence was greater in providers in centres with a deprivation index between the 25th and 50th percentiles, except for the guidance against tobacco, which was documented more frequently in the most disadvantaged group (DI above 75th percentile).
The mean patient volume of the PC paediatrics clinic was of 21.77 patients/day (SD, 3/19) in the subset of patients in which all recommendations were recorded and 22.69 patients/day (SD, 3.64) in the subset with gaps in the documentation (P = .05; mean difference, 0.92; 95% CI, 0.02–1.82).
We also found differences in the documentation of all individual recommendations except the guidance against tobacco use.
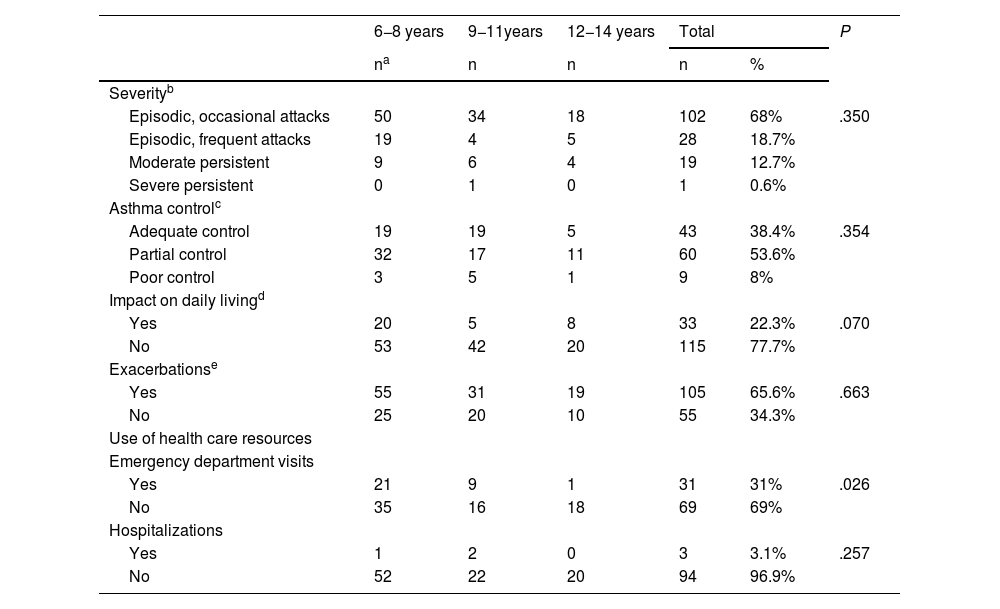
Clinical characteristics of the study sampleIn 68% of patients, the disease was classified as episodic or intermittent asthma. Asthma was partially controlled in 53.6%. Daily living was somehow affected in 22.3%. We found no significant differences in the clinical characteristics based on sex, age or SES, except in the frequency of emergency department visits in the past year, which was lower in the oldest age group (Table 5).
Clinical characteristics of the patients by age group at diagnosis in the patients in whom they were documented.
| 6−8 years | 9−11years | 12−14 years | Total | P | ||
|---|---|---|---|---|---|---|
| na | n | n | n | % | ||
| Severityb | ||||||
| Episodic, occasional attacks | 50 | 34 | 18 | 102 | 68% | .350 |
| Episodic, frequent attacks | 19 | 4 | 5 | 28 | 18.7% | |
| Moderate persistent | 9 | 6 | 4 | 19 | 12.7% | |
| Severe persistent | 0 | 1 | 0 | 1 | 0.6% | |
| Asthma controlc | ||||||
| Adequate control | 19 | 19 | 5 | 43 | 38.4% | .354 |
| Partial control | 32 | 17 | 11 | 60 | 53.6% | |
| Poor control | 3 | 5 | 1 | 9 | 8% | |
| Impact on daily livingd | ||||||
| Yes | 20 | 5 | 8 | 33 | 22.3% | .070 |
| No | 53 | 42 | 20 | 115 | 77.7% | |
| Exacerbationse | ||||||
| Yes | 55 | 31 | 19 | 105 | 65.6% | .663 |
| No | 25 | 20 | 10 | 55 | 34.3% | |
| Use of health care resources | ||||||
| Emergency department visits | ||||||
| Yes | 21 | 9 | 1 | 31 | 31% | .026 |
| No | 35 | 16 | 18 | 69 | 69% | |
| Hospitalizations | ||||||
| Yes | 1 | 2 | 0 | 3 | 3.1% | .257 |
| No | 52 | 22 | 20 | 94 | 96.9% | |
Most recent documentation of severity. The classification used was the classification included in the asthma care protocol of the Community of Madrid for 2021–2022 based on the GEMA guideline version 4.4, which establishes 4 severity categories at diagnosis.
Most recent documentation of asthma control using the CAN questionnaire. The questionnaire consists of 9 items about the symptoms experienced in the past month and establishes 3 levels of control: adequate (0 points), partial (1–8 points), poor (>8 points).
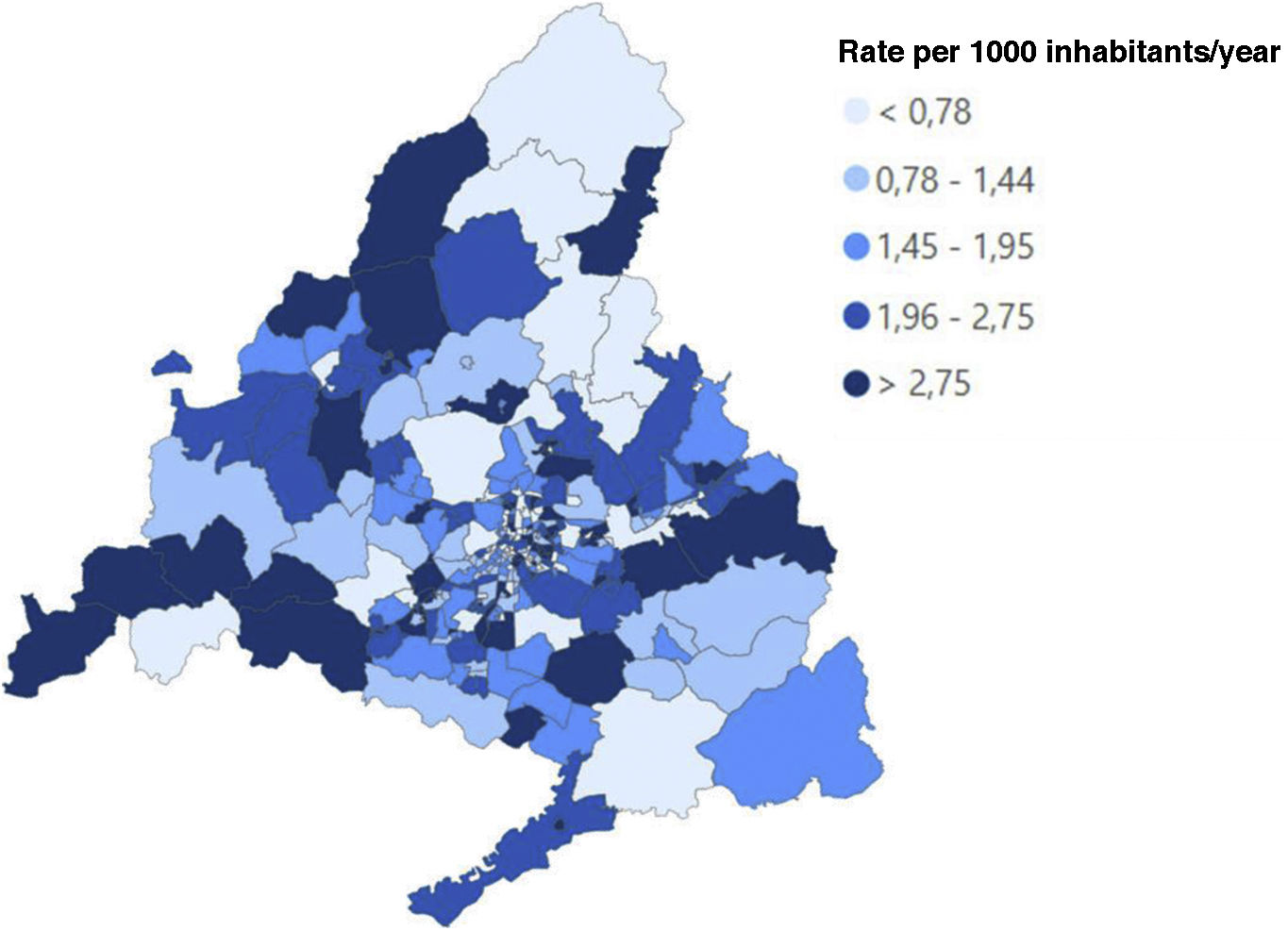
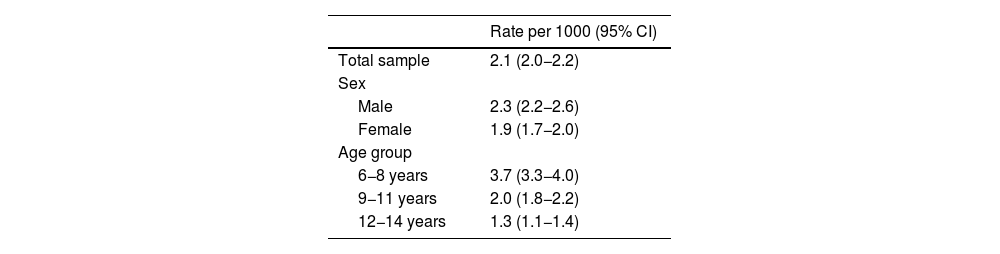
The recorded incidence of asthma was 2.1 newly diagnosed cases per 1000 children aged 6–14 years, with a higher incidence in the 6−8 years age group and male patients. We did not find any geographical clustering in the adjusted analysis (Fig. 2, Table 6).
Incidence of asthma (documented newly diagnosed cases) in the Community of Madrid in 2021.
| Rate per 1000 (95% CI) | |
|---|---|
| Total sample | 2.1 (2.0−2.2) |
| Sex | |
| Male | 2.3 (2.2−2.6) |
| Female | 1.9 (1.7−2.0) |
| Age group | |
| 6−8 years | 3.7 (3.3−4.0) |
| 9−11 years | 2.0 (1.8−2.2) |
| 12−14 years | 1.3 (1.1−1.4) |
CI, confidence interval.
To our knowledge, results on objective health care process and outcome indicators documented in patient health records at the PC level have never been published in Spain. Previous studies have been based on data obtained through self-report questionnaires completed by providers,11,21 which entails intrinsic risks of bias. Two studies in Spain used objective data to assess asthma drug prescribing obtained through the register of prescriptions dispensed in pharmacies (a study that reflected improvement in prescribing after a training intervention in paediatricians)22 and the implementation of a paediatric asthma care protocol.23
Process indicators provide information about the quality of health care resources and delivery14 in relation to the objectives set in CPGs.9,10 These indicators can be used in the development of a clinical audit programme to identify opportunities for improvement in asthma care. Research on the activities or resources that contribute most to improve health care outcomes in paediatric asthma has yet to be conducted in Spain.
Our study is the first conducted in Spain to contribute objective data on the adherence to CPGs by health care providers in the management of paediatric asthma, taking into account the clinical characteristics of the patients, the workload of physicians and the SES of the catchment population. The reproduction of this study in successive time periods could help improve health care outcomes in the asthma care protocol.
Our findings show that the documented adherence to the main recommendations for the management of paediatric asthma by health care professionals in the Community of Madrid is low. The adherence was greater for follow-up recommendations (12.73%) compared to diagnosis recommendations (5.84%).
In the separate analysis of each variable, performance of a lung function test was documented in only 4.5% of the patients at the time of diagnosis, a lesser percentage compared to previous studies conducted in Spain based on data from self-report questionnaires.21 This indicator could be underestimated, as not all PC centres routinely perform spirometry tests. In addition, the period under study followed the COVID-19 pandemic, when the conditions required to perform spirometry could not be met in PC settings.24
The severity of asthma was documented at the time of diagnosis in only 2.4% of the patients, compared to 11.1% of patients in subsequent follow-up evaluations. The low percentage documented at diagnosis may be related to the infrequent performance of spirometry in the PC setting, without which the classification of asthma severity is more challenging. A study in the Valencian Community based on self-reported data found that 59% of paediatricians reported recording the severity of asthma in the health record,21 yet a small clinical audit study found that the severity of asthma was documented in only 40% of children aged 6–14 years.25 Establishing the severity of disease is of vital importance to determine the required maintenance treatment.10
Structured asthma education and assessment of inhaler techniqueThe health record showed documentation of every recommended component of asthma education in only 13.5% of the patients. This frequency was lower compared to the results of previous studies in the PC setting (60%–85%), which were based on self-report questionnaire data.11,21 All guidelines highlight education as a key element in asthma management.9,11,26 One of the most important components of asthma education is teaching adequate inhaler technique.9,11 The assessment of inhaler technique at the office was documented in 14% of the patients, and education on behavioural changes to avoid exposure to triggers in 13.8%, with the exception of education about avoiding exposure to tobacco smoke, which was documented in 43%. These figures are far from the frequency reported in the aforementioned studies based on questionnaire data (93% and 84%, respectively).11 The greater adherence to the recommendation regarding education against tobacco use and exposure was probably due to the fact that this is also an intervention included in the routine healthy child preventive care programme and in the management of other diseases.
Analysis of adherence with recommendations by patient age, socioeconomic level and patient volumeWe found a higher frequency of documentation for all follow-up recommendations in children aged 6–8 years (Table 3). Younger children make more visits to the PC paediatrician, which provides an opportunity to initiate and continue asthma management and monitoring.27 Guidance against tobacco exposure was the sole recommendation documented more frequently in the group aged 12–14 years, probably on account of the increased risk of tobacco use in these patients.
The adherence to follow-up recommendations was greater in PC centres with a DI between the 25th and 50th percentiles, and the difference in frequency was significant for nearly all recommendations, with a directly proportional association between the adherence to follow-up recommendations and SES, except in centres with the highest SES (DI < 25th percentile) (Table 4). These differences could be explained by the lower attendance to PC centres in more disadvantaged segments of the population. Households in the highest SES group have more disposable income and may be more likely to use private health care services. This may explain why this is the only group in which the observed trend in the level of adherence was not maintained.
The only recommendation implemented more frequently in more disadvantaged groups based on the EHR was the education and guidance against tobacco, probably due to the known association between tobacco use and lower socioeconomic status.28
Previous studies conducted in other countries have concluded that socioeconomic inequality is associated with poorer asthma control and lower health care quality.29 However, in Spain, the only study conducted to date did not find evidence of this association.29
In our study, a higher patient volume was associated with less frequent documentation of the implementation of nearly all recommendations, possibly because providers had less time to devote to each patient, which affects the quality of health care records.
Recorded incidence and clinical characteristics of the sampleMost epidemiological studies on paediatric asthma in Spain have focused on the prevalence of the disease.30,31 Our study found incidence values similar to those reported in other studies conducted in Europe, which also found a greater incidence in the younger age group32–34 and in male patients.31,35
Most of the patients in the sample had partially controlled episodic asthma, in agreement with other studies conducted in Spain6,16,35,36 (Table 5). The poor asthma control observed in our study may be partly explained by the recent diagnosis of the patients, which is associated with a limited knowledge of the disease and its management. Asthma control was poorer in the oldest age group, which was consistent with the poorer adherence to treatment in adolescents.37 Paradoxically, most patients denied any impact of the disease in their daily lives (77.7%), probably on account of a low awareness of asthma symptoms in the patients or family members.9 As reported by other authors,38 we found the highest frequency of emergency department visits in the youngest age group (Table 5).
Limitations and strengthsThe main limitation of the study was the possible underestimation of the implementation of CPG recommendations due to a low frequency of documentation in the EHR by health care providers. This would explain the differences in relation to previous studies, which were based on surveys of health care professionals, who tend to overestimate the frequency of implementation. Another limitation is that we only had access to data for patients who use public PC services, so we were unable to assess the adherence to recommendations in other care settings. However, we ought to highlight that in the Community of Madrid, the percentage of the paediatric population that uses public health services out of the total population registered in the public health system is high (89.15% in 2021), so the data represented a large part of the population.39
The study period, one year after the COVID pandemic, may have affected the level of adherence in PC paediatricians compared to usual clinical practice.
The incidence of asthma found in our study may to be accurate. In real-world clinical practice, ICPC-2 code R96 is sometimes used to document acute episodes compatible with an asthma attack, leading to the inaccurate classification of some patients as having asthma. There may also have been patients with asthma in whom the records showed a different ICPC-2 code that would have therefore been left out of the study.
Among the strengths of the study, we ought to highlight that we assessed clinical practice by analysing quality indicators documented in the EHR, which offers more objective information. This approach allows the evaluation of provider performance for the purpose of developing strategies to improve clinical documentation and establish a baseline to analyse trends in quality indicators in future studies.
The low frequency of recorded implementation observed in our study provides a baseline from which to verify progress in the implementation of asthma care protocol indicators in the Community of Madrid.
Another strength was the identification of the association of care quality with the SES of the catchment population and the patient volume, which opens a new line of research on the external factors that may have an impact on the level of adherence to follow-up recommendations at the PC level.
Future lines of researchOur study evinced the need to improve asthma care in the Community of Madrid and the adherence of providers to care protocols developed for the purpose. Strategies to improve the training of PC paediatricians should be promoted, with emphasis on the importance of performing spirometry tests and periodic assessments of inhaler technique and the crucial role of education. Repeating this study would be interesting to determine whether analysed care quality indicators improve after such training.
ConclusionIn this study, we found a low level of adherence to the recommendations of child asthma CPGs, although this statement must be interpreted with caution due to the infrequent documentation. Adherence increased in younger patients, with increasing SES and with decreasing patient volume. Identifying the factors associated with poorer adherence can help identify those patients who require more attention from health care professionals and, ultimately, to improve the management of asthma at the PC level, where additional studies will be required to assess for changes.
FundingThis research did not receive any external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.