Point-of-care ultrasound (POCUS) has become an essential tool for clinical practice in recent years. It should be considered as an extension of the standard physical examination, which complements and enriches it without substituting it. POCUS enables the physician to answer specific clinical questions about the diagnosis, to understand better the pathophysiological context, to orientate the treatment, and to perform invasive procedures more safely. Despite its current use in many centres, and in most paediatric sub-specialties, there are currently no specific recommendations addressing educational aims in the different training areas, as well as methodology practice and the certification process in paediatrics. These ingredients are essential for POCUS implementation in daily practice, with a quality guarantee in terms of efficiency and safety.
Several POCUS experts in different paediatric medicine environments performed a non-systematic review addressing the main paediatric POCUS applications in paediatrics. The lack of educational programmes in POCUS in Spain is also discussed, and the experience in the United States of America in this topic is provided.
Considering the current situation of POCUS in paediatrics, we strongly believe that it is urgent to establish evidence-based recommendations for POCUS training that should be the base to develop educational programmes and to include POCUS in the paediatric residency training.
La ecografía a pie de cama (EPC) se ha convertido en los últimos años en una herramienta imprescindible para la práctica clínica. La EPC debe entenderse como una extensión de la exploración física habitual que, sin sustituirla, la complementa y la enriquece. La EPC permite al clínico responder preguntas concretas sobre el diagnóstico, entender mejor la fisiopatología, orientar el tratamiento o realizar procedimientos invasivos con mayor seguridad. A pesar de su integración en muchos centros y en las diferentes subespecialidades pediátricas, no disponemos de recomendaciones específicas que establezcan los objetivos formativos en las distintas áreas de capacitación, la metodología de entrenamiento o la certificación de competencias en pediatría. Estos elementos son imprescindibles para que la EPC pueda implementarse en la práctica diaria con garantías de eficiencia y seguridad.
Este artículo aborda las principales aplicaciones de la EPC en pediatría mediante una revisión no sistemática por parte de expertos en diferentes áreas de la práctica clínica en España. Además, se discute acerca de la falta de planes formativos a nivel estatal, contando con la aportación de la experiencia de Estados Unidos.
En vista de la situación actual de la EPC, en nuestra opinión es urgente que se establezcan recomendaciones basadas en la evidencia para el entrenamiento en EPC que sirvan como base para el desarrollo de planes formativos y la integración de la EPC en el programa formativo de la especialidad.
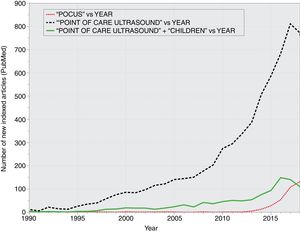
Since its introduction in clinical practice in the mid-20th century, ultrasonography has been a valuable tool that allows non-invasive visualization of various anatomical structures. Its main advantage compared to other imaging tests is that it does not employ ionising radiation. Furthermore, it can be performed quickly and at the bedside (so that patients need not be moved), and it also allows serial imaging, which enables physicians to estimate the effectiveness of interventions prescribed to patients without depending on other professionals. Although it is mainly practiced by radiologists, it has been decades since ultrasonography became an indispensable technique in other medical and surgical specialities, such as cardiology or gynaecology and obstetrics.1 The use of ultrasonography by physicians not specialised in diagnostic imaging as an adjunct to the physical examination has been termed bedside ultrasound or point-of-care ultrasound (PoCUS).1 While the use of PoCUS is not free of controversy and particularities,2,3 it appears to be already established in clinical practice (Fig. 1), compelling several scientific societies to adopt clear positions on the matter.4,5
Due to the broad range of the existing paediatric subspecialties and the anatomical and pathophysiological characteristics of paediatric patients (clearly different from those of adults), the integration of PoCUS in paediatrics involves particular aspects that are not at play when it comes to its use in other fields of medicine.
At present, the educational curriculum for the speciality of paediatrics and its subspecialities in Spain falls under the authority of the Ministry of Health.6 The current curriculum specifies that specialists in paediatrics must have the necessary skills to perform and interpret the diagnostic tests relevant to the practice of paediatrics, including echocardiography and other invasive techniques such as placement of central venous catheters, which requires ultrasound guidance.7 In spite of this, training in PoCUS has not yet been defined specifically within this curriculum, nor in the White Book of Paediatric Specialities, except in the field of paediatric rheumatology.8
In the past decade, working groups have emerged within paediatric societies in Spain with the aim of promoting the use of PoCUS and providing education and conducting research on this technique.9,10
The aim of our article was to offer an overview of the use of PoCUS from the perspective of different fields in paediatrics, taking into account the various applications of this technique and the current training resources and needs in the field.
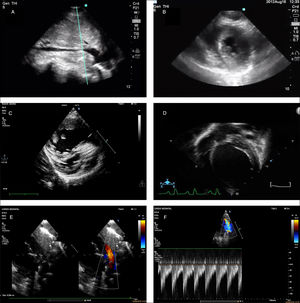
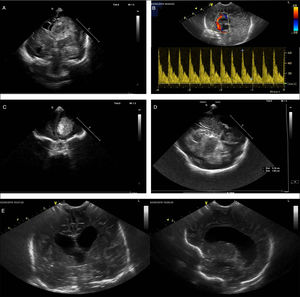
Focused cardiac ultrasound“Focused cardiac ultrasound” (FoCUS) is a widely accepted term to refer to the use of echocardiography performed by clinicians at the bedside for assessment of patients with signs or symptoms of haemodynamic compromise.11 Unlike standard echocardiography performed by a cardiologist, the goal of FoCUS is not a full anatomical or functional evaluation. In FoCUS, the clinician performs a simplified but systematic examination to try to obtain key information regarding the physiology of the haemodynamically unstable patient (why does the patient have low blood pressure? Would the patient benefit from administration of fluids? Would it be better to initiate inotropic therapy? [Fig. 2]) or to detect critical conditions such as cardiac tamponade. The routine FoCUS examination includes the subcostal window (long axis and inferior vena cava), the apical window and the parasternal window (long axis and short axis). The key elements of FoCUS are the assessment of the pericardium, the relative size of the chambers, systolic function and volume status. There is evidence that in patients with shock, FoCUS allows the detection of the predominant underlying mechanism (cardiogenic, obstructive or hypovolemic/distributive shock), leading to changes in management, reducing the delay in treatment initiation and improving outcomes12 (Table 1). In addition, assessment of these patterns can lead to the identification of reversible causes of non-shockable cardiac arrest, and the presence or absence of organised cardiac activity is an important predictor of return of spontaneous circulation.13 Clinical practice guidelines and scientific societies specify that training in FoCUS must be included in the core curriculum of medical specialties such as intensive care, anaesthesiology or emergency medicine, and that guidelines should be established as to how this training should be structured.11,14,15 Although there is substantial variability in the educational methodology, most initiatives this far have promoted learning based on skill assessment and supervised individual practice with real-world patients with review of the obtained images, and highlighted the usefulness of e-learning tools.11 International guidelines support the usefulness of PoCUS in paediatrics and provide recommendations for clinical practice.11,14 Training in FoCUS is already a reality in the curriculum of certain paediatric specialties, such as paediatric intensive care and neonatology.16 However, no consensus has been established to date on how paediatricians should be trained in FoCUS beyond the initiatives in individual institutions.17 Therefore, we need to make a concerted effort to establish curriculum standards for training in FoCUS in the different paediatric subspecialties where it may be used.
Point-of-care ultrasound images corresponding to different clinical situations. (A) Inspiratory collapse of inferior vena cava, subcostal view. Sign indicative of hypovolemia in the context of compatible clinical manifestations. (B) Left ventricular systolic collapse, parasternal short axis view. Sign suggestive of hypovolemia in the context of compatible clinical manifestations. (C) Image compatible with dilatation of right ventricle and septal flattening suggestive of pulmonary hypertension. (D) Image showing dilatation of left ventricle in the context of haemodynamic instability, suggestive of severe ventricular dysfunction. (E) Large patent ductus arteriosus in preterm infant. (F) Doppler image at the level of the left pulmonary artery showing an increased end diastolic flow velocity, suggestive of increased pulmonary blood flow and haemodynamically significant patent ductus arteriosus.
Summary of the main potential applications of point-of-care ultrasound in paediatric intensive care, highlighting the required level of training and the most frequent sonographic findings.
| Clinical context | Application and level of training | Sonographic findings |
|---|---|---|
| CA12,13 | Overall cardiac activity (A) | • Pseudo-PEA: organised cardiac activity• Asystole-true PEA: absence of organised electrical activity (“cardiac standstill”) |
| Haemodynamic assessment11,14,15 | Assessment of volume status (B)• Size of heart chambers• Size and inspiratory collapse of inferior vena cava | Hypovolemic/distributive shock• Small “empty” chambers with tendency to collapse during systole (due to compensatory increased cardiac contractility)• Small IVC diameter with tendency to collapse with inspiration |
| Assessment of LV systolic function (B)• LV size• Visual assessment of function• Inferior vena cava | Cardiogenic shock• Enlarged left ventricle (not always)• Subjective visual assessment of LV function (“eye-balling”): decreased overall systolic motion, reduced diastolic mitral valve leaflet excursion towards the septal wall, reduced to non-existent thickening of LV walls during systole.• Dilated IVC with reduced respiratory changes | |
| Right ventricle size and pressure (B)• Relative ventricle sizes• Septal curve | Obstructive shock with RV failure/enlargement• RV enlargement (RV:LV ratio >0.6 in older children and >1 in young children)• Interventricular septum bowing towards the left (increased RV pressure) | |
| Pericardium (B)• Effusion• Compression of heart chambers | Obstructive shock with cardiac tamponade• Presence of pericardial effusion and diastolic collapse or right heart compression• LV underfilling and hypercontractility | |
| Respiratory assessment1,8–16 | Pleural effusion (B) | • Identification and measurement of fluid collection in pleural cavity• Characteristics of effusion (complicated/uncomplicated) |
| Consolidation (B) | • Hepatization of lung parenchyma, absence of signs of lung aeration | |
| Lung aeration and/or extravascular lung water (A) | B-lines and consolidation/atelectasis (number, size and shape) | |
| Detection of pneumothorax (B) | • Absence of lung sliding.• Lung point sign• Absence of lung pulse and B-lines | |
| Diaphragm motion (A) | Diaphragmatic excursion (B-mode and M-mode)Percent change in diaphragm thickness in inspiration | |
| Neurologic assessment | Midline shift17 (A) | Measurement of the distance from the transducer to the third ventricle from the left and right sides through the transtemporal window (under normal circumstances, they should be approximately the same) |
| Transcranial Doppler1,18–28 (A) | Assessment of cerebral blood flow: measurement of flow velocities in the vessels of the circle of Willis. Calculation of PI and RI | |
| Assessment of pupillary function (A) | Assessment of pupillary diameter and light reflex | |
| Optic nerve sheath29–32 (A) | Increased diameter in context of increased ICP | |
| Abdominal assessment (polytrauma) | eFAST33–35 (B) | • Detection de haemoperitoneum• Detection de haemopericardium• Detection de haemopneumothorax |
| Performance of ultrasound-guided procedures | Vascular access1,36–40,41–43 (B) | Ultrasound-guided insertion of arterial, central venous and peripheral venous catheters |
| Endotracheal intubation (A) | Assessment of air column in trachea and oesophagus, lung sliding and endotracheal tube placement (TRUE protocol) | |
| Shunt placement1,44–52 (A) | Ultrasound-guided procedures (thoracentesis, paracentesis and pericardiocentesis) | |
| Monitoring of urinary catheter35 (B) | Bladder volume, catheter patency, assessment of placement and volume of catheter balloon |
(A), advanced training; (B), basic training; CA, cardiac arrest; eFAST, extended focused assessment with sonography in trauma; ICP, intracranial pressure; IVC, inferior vena cava; LV, left ventricle; PEA, pulseless electrical activity; PI, pulsatility index; RI, resistance index; RV, right ventricle.
Despite the late introduction of PoCUS in primary care (PC), the technique has experiencing substantial grow in this setting in recent years.18 The use of PoCUS has been introduced in everyday clinical practice in adult care in many primary care centres in Spain.19 Point-of-care ultrasound could also be very useful to PC paediatricians. However, its use in this field is still rare, probably due to a lack of training and continuing education resources, low staffing, heavy caseloads, the perception of encroachment on the scope of practice of other professionals and concerns regarding potential medico-legal issues. Nevertheless, there are initiatives such as the Working Group on Clinical Ultrasonography of the Asociación Española de Pediatría de Atención Primaria (Spanish Association of Primary Care Paediatrics, AEPAP) that seek to extend its use, promoting education and the diffusion of information among PC paediatricians.20 An essential aspect to take into account in this particular setting is that the purpose of PoCUS is to explore specific clinical questions as opposed to performing a comprehensive anatomical assessment, with selective use for assessment of the most prevalent diseases in which it has demonstrated a superior effectiveness compared to the physical examination alone.19 One obvious example is the diagnosis of community-acquired pneumonia.21 Other situations in which PoCUS could lead to improved care are the diagnosis of soft-tissue infections (cellulitis vs abscesses), detection of joint effusion or screening of developmental dysplasia of the hip in infants (Table 2). We ought to underscore that the introduction of PoCUS in the practice of PC paediatrics requires adequate planning, not only in terms of material costs, but also by adapting the duration of visits to allow its correct use.
Summary of the main potential applications of point-of-care ultrasound in paediatric emergency care, primary care and inpatient care, highlighting the required level of training and the most frequent sonographic findings.
| Clinical context | Application and level of training | Sonographic findings |
|---|---|---|
| Haemodynamic assessment | See Table 1 on echocardiography in PICU setting | |
| Respiratory assessment | ||
| Neurologic assessment | ||
| Polytrauma assessment | ||
| Abdominal assessment | Intussusception (B) | Target/doughnut signPseudokidney sign |
| Appendicitis (A) | Diameter of appendix>6mm, noncompressible appendix, appendicolithIndirect signs: hyperechogenic surrounding fat, free fluid, collections of fluid around appendix (abscess) | |
| Hypertrophic pyloric stenosis (B) | Measurement of length of pyloric canalMeasurement of thickness of muscular layer | |
| Cholecystitis (A) | Thickening and distension of gallbladderDetection of gallstones (calculous cholecystitis) | |
| Musculoskeletal assessment | Hip dysplasia screening (A) | α angle (bony roof)β angle (cartilaginous roof) |
| Long bone and clavicle fractures (B) | Cortical disruption/step-offPosterior fat pad sign in supracondylar region | |
| Skull fractures (B) | Cortical disruption/step-off | |
| Joint effusion (B) | Detection of intra-articular fluid | |
| Soft tissue assessment | Soft-tissue infection (B) | Cellulitis (subcutaneous oedema with cobblestone appearance, hyperaemia)Abscesses (anechoic fluid collection with no vessels inside, hypoechoic halo)Pyomyositis (muscular oedema with or without abscesses) |
| Foreign body (B) | Detection of foreign bodyIdentification of type of foreign body based on ultrasound artefacts | |
| Cervical mass (A) | Evaluation of lymphadenopathyCystic vs solid cervical masses | |
| Nephrourologic evaluation | Assessment of bladder volume (B) | Assess for presence of urineCalculation of bladder volume (Volume=0.52×maximum anteroposterior×transversal×longitudinal diameters) |
| Hydronephrosis (B) | Dilatation of renal pelvis and calyces, thinning of renal parenchymaUreteral (dilatation (ureterohydronephrosis) | |
| Urolithiasis (A) | Detection of renal lithiasisDilatation of urinary tract | |
| Testicular (A) | Assessment of testicular blood flowTesticular size and sonographic pattern (comparison with contralateral testis) | |
| Ophthalmologic evaluation | Intraocular disease (A) | Detection of intraocular disease: detached retina, vitreous haemorrhage, etc. |
| Ultrasound-guided/-assisted procedures1,9,26–28 | Vascular access (B) | Arterial, central venous and peripheral venous access |
| Thoracentesis (B) | Ultrasound-assisted puncture (identification of optimal puncture site)Ultrasound-guided puncture (small effusions near solid organs) | |
| Lumbar puncture (A) | Location of interspinous space for puncture (e.g. obesity)Visualization of epidural and subarachnoidal spaces (newborns and infants) | |
| Reduction of fractures (B) | Post-reduction alignment of cortical bone | |
| Suprapubic puncture (B) | Verification of presence of urine. Selection of puncture site | |
| Arthrocentesis (B) | Ultrasound-assisted (identification of optimal puncture site) | |
| Abscess drainage/removal of foreign bodies (B) | Identification of optimal drainage site | |
| Confirmation of intraosseous vascular access (A) | Needle crossing cortex | |
(A), advanced training; (B), basic training.
Point-of-care ultrasound has been integrated progressively in inpatient paediatric care in the past few decades, with the strongest impact in paediatric emergency care.22 The inclusion of PoCUS in the educational curriculum of emergency care paediatricians23 and the position of the American Academy of Pediatrics in support of its use in this setting5 have promoted the consolidation of PoCUS as an essential technique in paediatric emergency departments. Its use in this setting has been described relative to its use in inpatient care and other medical specialities.
Of the applications of PoCUS in the hospital setting (Table 2), the ones currently supported by an adequate amount of evidence include focused assessment with sonography for trauma (FAST), the detection of pneumonia, detection of fractures, assessment of soft tissues (cellulitis/abscesses) and guidance in the performance of interventions such as insertion of vascular catheters, reduction of fractures, lumbar puncture or suprapubic puncture.5,24 Research has also been conducted on the use of PoCUS in other situations (abdominal complaints, bronchiolitis, presence of foreign bodies, joint effusion and cervical masses), although the evidence published to date in scarce. In any case, when it comes to the introduction of PoCUS, each facility needs to determine which applications would be most beneficial based not only on the current evidence, but also on its specific needs and available resources.
Training in PoCUS is widely available in the form of courses, books and online materials.25 However, the lack of nationwide hospital-based training programmes hinders the acquisition of practical skills, which depends largely on the availability of sonographers and experienced staff. In this regard, future efforts should focus on the consolidation of hospital-based training programmes in PoCUS to promote a more comprehensive and standardized education on the technique.
Point-of-care ultrasound in paediatric intensive care:The use of PoCUS in paediatric intensive care units (PICUs) has grown considerably in the past few years.7,26 Several authors claim that its use in the PICU improves clinical assessment, leads to changes in management in up to 40% of patients27 and increases the safety of invasive procedures.28 In the field of adult intensive care, there are already consensus guidelines for training in ultrasound published by medical societies in related fields,4,14 including some recommendations for paediatric patients.14
The main applications of PoCUS in the PICU include (Table 1):
- •
FoCUS: already described in the section on echocardiography (Fig. 2).
- •
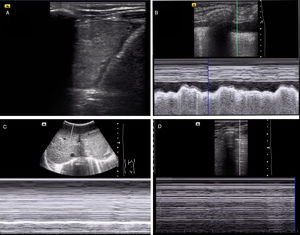
Lung ultrasound: Allow ruling out/diagnosis of pneumothorax and detection of lung consolidation and pleural effusion (Fig. 3). It is also useful for detection of diaphragmatic paresis/paralysis and to verify endotracheal tube placement.29
Figure 3.Diagnosis of different respiratory diseases by means of PoCUS. (A) Lung consolidation associated with pleural effusion. (B) Identification of pleural effusion on M-mode (sinusoid sign). (C) Evaluation of diaphragm motion in M-mode, with absence of diaphragmatic excursion (compatible with diaphragm paresis). (D) Absence of lung sliding in M-mode, suggestive of pneumothorax (stratosphere/barcode sign).
- •
Neurosonology: estimation of intracranial pressure and its effects by transcranial Doppler ultrasound, measurement of optic nerve sheath diameter.26 It is also useful to assess midline shift in space-occupying lesions.
- •
Abdomen: Mainly detection of free fluid with the FAST protocol.30 It is also useful to monitor urinary catheters and the condition of the bladder in cases of anuria.
- •
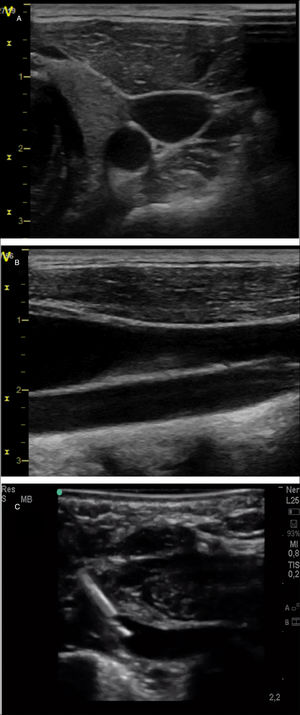
Ultrasound-guided procedures: vascular catheter placement9 (Fig. 4), paracentesis, pericardiocentesis, thoracentesis/chest tube insertion.9
Figure 4.Exploration of cervical vessels by means of PoCUS. (A) Transversal view of vessels, with identification of carotid artery as a round hypoechoic structure and the jugular vein as an oval, more superficial hypoechoic structure. (B) Longitudinal view of the vessels, with identification of jugular vein in a more superficial level and the carotid artery in a deeper level. (C) Subclavian vein cannulation in a newborn infant with a long-axis/in-plane approach.
A key aspect in the use of sonography in the PICU is training, and to this date a standardized educational programme has not been established. Conlon et al. proposed a 16-hour theoretical and practical training programme followed by correct performance of a minimum of 25 studies in non-procedural applications (haemodynamic, thoracic and abdominal assessment) to assess competence in these skills,17 which is similar to the recommendations of the American College of Emergency Physicians.15 However, in our experience and that of other authors,4 the number of supervised ultrasound studies varies significantly between individuals, making it difficult to estimate an appropriate minimum number.
The consensus guidelines for training in adult intensive care sonography in Spain suggests different levels of training and specifies the different requirements for the main applications of PoCUS in this field. The basic level includes: lung ultrasound, ultrasound-guided vascular access, abdominal ultrasound, transcranial doppler ultrasound and basic echocardiography.4
The ultimate objective is to design a longitudinal curriculum with several training stages detailing the use of simulation, the number of ultrasound studies required for practice and the exams to be performed for certification and recertification in the overall use of sonography or specific applications, in addition to the development of a system for instructor accreditation.4,31 This calls for the development of guidelines and recommendations by the Working Group of the Sociedad Española de Cuidados Intensivos Pediátricos (Spanish Society of Paediatric Intensive Care, SECIP).
Point-of-care ultrasound in newborn infantsAt present, PoCUS is an indispensable diagnostic tool in neonatal unites, where the advantages that we have already mentioned allow its use in this vulnerable subset of patients.
It is mainly used for evaluation of the brain, heart, abdomen and lungs and performance of ultrasound-guided procedures (Table 3).
Summary of the main potential applications of point-of-care ultrasound in neonatal care, highlighting the required level of training and the most frequent sonographic findings.
| Clinical context | Application and level of training | Sonographic findings |
|---|---|---|
| Haemodynamic assessment10,33,38 | CO and SVC flow (A) | • Measurement of LVOT, RVOT and SVC diameters.• Measurement of velocity-time integral |
| Systolic and diastolic function in each ventricle(A) | • Ejection fraction and fractional shortening, tissue Doppler, strain (left ventricle)• TAPSE, tissue Doppler, FAC (right ventricle)• E/A ratio and tissue Doppler (filling pressure) | |
| Assessment of PDA (pulmonary overcirculation and/or systemic hypoperfusion)(A) | • Ductus diameter>1.5mm or 1.4mm/kg, pulsatile pattern and/or low flow velocity (<1.5m/seg) are indicative of Hs-PDA• DV in LPB (>0.2m/seg in end diastole indicative of overcirculation), LA/Ao ratio (>1.4, suggests LA enlargement), mitral flow E/A ratio (E>A indicates an increase in filling pressure), left CO/SVC flow ratio (>4 is indicative of a significant shunt), DV in postductal arteries (“diastolic steal” indicative of peripheral hypoperfusion). | |
| Assessment of pulmonary flows(A) | • Direction of shunt in ductus and foramen (bidirectional or right-left)• Peak TR velocity (estimation of pulmonary pressure)• Leftward shift of interventricular septum• Doppler pattern and pulmonary acceleration time | |
| Presence of pericardial effusion (B) | Detection of fluid collection in pericardial cavitySigns of compression of right side of heart | |
| Neurologic assessment32 | Confirmation of normal anatomy (B) | • Confirmation of symmetry• Assessment of midline |
| Structural lesion (ischaemic or haemorrhagic) (A) | Intraventricular haemorrhage, periventricular infarction, arterial infarction, parenchymatous haemorrhage, extra-axial bleeding. | |
| Diagnosis of venous and arterial strokes. Assessment of dural venous sinuses (A) | • Measurement of flow velocity in anterior cerebral, middle cerebral and carotid arteries.• Calculation of PI and RI.• Confirmation of patency of dural venous sinuses. | |
| Pattern of brain maturation in preterm infants. Assessment of white matter lesions (A) | Monitoring of periventricular echogenicity, ventricular size and extra-axial spaces as markers of white matter injury | |
| Assessment of hydrocephalus (A) | Levene index, diameters of frontal horn, third ventricle and fourth ventricle, thalamo-occipital distance | |
| Respiratory and abdominal assessment34 | Assessment of pneumothorax (B) | • Absence of lung sliding or equivalent signs• Lung point sign |
| Pleural effusion or excess abdominal fluid (B) | Detection of excess fluid in pleural spaceDetection of free fluid in abdomen | |
| Lung consolidation B) | • Hepatization of lung parenchyma• Absence of signs of lung aeration | |
| Assessment of lung aeration (A) | Presence of B-lines and consolidation/atelectasis (number, size and shape) | |
| Ultrasound-guided procedures35 | Thoracentesis/paracentesis (B) | Identification of site for needle access and fluid drainage |
| Vascular access (B) | Ultrasound-guided puncture and assessment of position of CVC tip |
(A), advanced training; (B), basic training; CO, cardiac output; CSF, cerebrospinal fluid; CVC, central venous catheter; DV, diastolic velocity; E/A, early filling (E) wave to atrial contraction (A) wave ratio; FAC, fractional area change; Hs, haemodynamically significant; LA/Ao, left atrial to aortic root ratio; LPB, left pulmonary branch; LVOT, left ventricular outflow tract; PDA, patent ductus arteriosus; PI, pulsatility index; RI, resistance index; RVOT, right ventricular outflow tract; SVC, superior vena cava; TAPSE, tricuspid annular plane systolic excursion; TR, tricuspid regurgitation.
Transcranial Doppler ultrasound (Fig. 5): allows detection of brain lesions using different acoustic windows (anterior, posterior, mastoid and temporal fontanelles), offering information useful for diagnosis and prognosis. Serial studies allow assessment of brain maturation in preterm infants to determine whether it is adequate, and it is an essential tool in the identification of the aetiology of structural lesions.32
- 1.
Echocardiography: it assesses the structure and function of the heart. Functional echocardiography can be used to measure rapid haemodynamic changes in the newborn and assess response to treatment (Fig. 2). The concept of neonatologist-performed echocardiography (NPE) has been gaining ground in neonatal units in the past 20 years, advancing the notion that neonatologists are the professionals best suited to evaluate haemodynamic function in infants with a structurally normal heart (with no evidence of congenital heart defects, excluding patent foramen ovale and patent ductus arteriosus).33
- 2.
Chest ultrasound: assessment for presence of pneumothorax, pleural effusion, lung consolidation or atelectasis.29,34
- 3.
Abdominal ultrasound: assessment of malformations of abdominal organs, ascites, splanchnic haemodynamic changes and placement of urinary catheters.
- 4.
Insertion and assessment of placement of intravascular catheters: useful to reduce the risk of complications associated with central venous catheter insertion, including in very-low-birthweight newborns, and to verify correct placement of the catheter.35
Brain examinations performed by means of PoCUS in newborn infants. (A) Coronal plane, hypoechoic image compatible with intraventricular haemorrhage with midline shift. (B) Doppler ultrasound image of pericallosal artery in a patient with decompensating hydrocephalus revealing increased resistance (pulsatility index, 1.94) compatible with increased intracranial pressure. (C) Coronal view showing a hyperechoic lesion in the frontal region. (D) Ultrasound image obtained through the transtemporal window showing a hyperechoic lesion compatible with haemorrhage with midline shift. (E) Coronal view (left) and sagittal view (right) of a newborn infant with meningitis, with detection of ventriculomegaly.
In the United States (US), paediatric ultrasound imaging has traditionally belonged to the scope of radiology and cardiology subspecialty practice. Adult emergency care physicians recognized the importance of integrating point-of-care ultrasound (POCUS) in their practice and representative societies supported its clinical use in the 1990s, followed by the publication of the first guidelines on the subject in 2001.15 Diagnostic and procedural ultrasound training is now a required component of training in emergency medicine residency and adult critical care fellowship programmes.36
Paediatric specialists in the US have followed the lead of their peers in adult medicine. In 2015, the American Academy of Pediatrics endorsed broadening the scope of ultrasound practice to include paediatric emergency care providers.5 The Society of Critical Care Medicine recently supported guidelines for use of POCUS in critical care that included a narrow range of paediatric diagnostic and procedural applications. The applications, training and credentialing processes relevant to paediatric critical care medicine (PCCM) have been described in the literature.17 Furthermore, a 2017 survey of PCCM programmes accredited in the US by the Accreditation Council for Graduate Medical Education found that 64% included practice of diagnostic POCUS and 98% offered access to ultrasound machines.37 In 2011, The American Society of Echocardiography (ASE), in collaboration other societies in Europe, published practice guidelines and recommendations for targeted neonatal echocardiography training.38 These guidelines have been criticized as overly prescriptive and the training requirements unfeasible for neonatal specialists.39 More recently, the ASE has recognized the clinical benefit of “focused cardiac ultrasound,” defined as “an adjunct to the physical examination to recognize specific ultrasonic signs,” though the scope of these recommendations is limited to adult care.
Bedside ultrasound providers across paediatric specialties continue to work on standardizing the training curriculum, offering training, developing competency, structuring quality assurance and creating paths for institutional credentialing. Such structural elements have been successful in advancing adult emergency medicine POCUS programmes,15 but have yet to be established in paediatric specialties.17 Medical liability concerns are often identified as barriers to the integration of POCUS in clinical practice in the US, even though both the adult and paediatric medical literature suggest that not performing ultrasound examinations when the technology is available puts providers at greater risk of medico-legal problems.3 In 2012, a survey of US medical schools found that 62% of responding institutions included ultrasound training in their curricula.40 Thus, a generation of medical students that have already been trained in the use of ultrasound will soon be pursuing careers in paediatrics. Integrating clinical knowledge and experience with POCUS technology in the next generation of paediatric providers will be an exciting challenge in paediatric clinical practice in the US.
Discussion and conclusionsThis article aimed at offering a multidisciplinary perspective on the use of PoCUS in different fields within paediatrics. To do so, we engaged the collaboration in developing the manuscript of paediatricians in different paediatric subspecialities that have played key roles in the introduction and diffusion of PoCUS in Spain (and in the United States).7,9,10,17 We ought to highlight that while this article includes numerous references to the current scientific evidence in support of the use of PoCUS in paediatrics, we did not carry out a systematic review and meta-analysis of the scientific literature on the applications proposed in this article, especially as regards their classification as basic or advanced.
The use of PoCUS, a non-invasive, safe, repeatable technique that can be useful in everyday clinical practice if performed by a skilled individual, is already widespread in different fields in paediatrics in several countries, including Spain.5,7 Some international guidelines include recommendations for use in paediatrics, for instance for lung ultrasound in critical paediatric patients or for FoCUS.11,29 However, with the exception of its use in paediatric emergency care in the United States,5,23 there are no clinical guidelines specifying the basic applications of PoCUS in the field of paediatrics or how training on this technique should be delivered and accredited. We believe that this is a key aspect for the adequate introduction of PoCUS, whose application, as is the case of other methods, requires adequate knowledge of the technique and its limitations, and must always fit the clinical situation of the patient. Disregarding these prerequisites could lead to mistakes in clinical decision-making and have a negative impact on patients.1
An essential aspect that must be underscored is that PoCUS is to be used as an adjunct to the customary clinical evaluation to address specific questions relevant to the management of the patient, and never in place of a comprehensive ultrasound evaluation by the cardiologist or radiologist when one is needed.
Some authors have reported that the learning curve for some ultrasound applications is relatively quick, so that only a few additional ultrasound studies need to be performed after theoretical and practical training for an adequate educational outcome.17,37 Another advantage of PoCUS is that several of its applications are used across subspecialities, as is the case of lung ultrasound.
In light of all of the above, we advise the definition of a minimum set of PoCUS applications that ought to be included in the educational curriculum of medical residencies in paediatrics at different levels of care and its different subspecialities. This should be accompanied by the establishment of criteria for the maintenance of these competencies, such as the minimum number of PoCUS studies that must be performed per year.
Another necessary step is for the different paediatric societies in Spain and Europe to establish their positions regarding the use of PoCUS, which would foster the development of specific training programmes and thus promote a more widespread and better integration of this technique in clinical practice.
Last of all, further evidence is required on the use of PoCUS in different fields within paediatrics for the purpose of establishing clear recommendations for its use as well as adequate educational programmes.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Mayordomo-Colunga J, González Cortés R, Bravo MC, Martínez Mas R, Vázquez Martínez JL, Renter Valdovinos L, et al. Ecografía a pie de cama: ¿es el momento de incluirla en la formación del pediatra? An Pediatr (Barc). 2019;91:206.