Point-of-care (bedside) ultrasound is being increasingly used by paediatricians who treat critically ill children. The aim of this study is to describe its availability, use, and specific training in Paediatric Intensive Care Units in Spain.
Material and methodsA descriptive, cross-sectional, multicentre study was performed using an online survey.
ResultsOf a total of 51 PICUs identified in our country, 64.7% responded to the survey. Just over half (53.1%) have their own ultrasound machine, 25% share it, with other units with the usual location in the PICU, and 21.9% share it, but it is usually located outside the PICU. Ultrasound machine availability was not related to size, care complexity, or number PICU admissions. The ultrasound was used daily in 35% of the units, and was associated with the location of the machine in the PICU (P=.026), the existence of a transplant program (P=.009), availability of ECMO (P=.006), and number of admissions (P=.015). 45.5% of PICUs have less than 50% of the medical staff specifically trained in bedside ultrasound, and 18.2% have all their medical staff trained. The presence of more than 50% of medical staff trained was associated with a higher rate of daily use (P=.033), and with specific use to evaluate cardiac function (P=.033), intravascular volume estimation (P=.004), or the presence of intra-abdominal collections (P=.021).
ConclusionsBedside ultrasound is frequently available in Spanish PICUs. Specific training is still variable, but it should serve to enhance its implementation.
La ecografía a pie de cama es cada vez más utilizada por los pediatras que tratan a niños críticos. El objetivo del estudio es describir la disponibilidad, el uso y la formación específica existente para esta técnica en las UCIP de nuestro entorno.
Material y métodosSe realizó un estudio descriptivo transversal multicéntrico mediante una encuesta en línea.
ResultadosSe identificaron 51 UCIP en nuestro país, el 64,7% respondió a la encuesta. El 53,1% dispone de ecógrafo propio, el 25% lo comparte con otras unidades ubicándose en la unidad y el 21,9% dispone de él pero está ubicado en otra unidad. La disponibilidad de ecógrafo no se relacionó con el tamaño, la complejidad asistencial o el número de ingresos anuales. El 35% emplea la ecografía diariamente; esto se relacionó con la ubicación del ecógrafo en la unidad (p=0,026), con la realización de trasplantes (p=0,009), la disponibilidad de ECMO (p=0,006) y con el número de ingresos anuales (p=0,015). El 45,5% tiene menos del 50% de sus médicos con formación específica; el 18,2% ha formado a todos sus médicos. La presencia de más del 50% de médicos formados se asoció con mayor utilización a diario (p=0,033) y con su uso para evaluar la función cardiaca (p=0,033), la volemia (p=0,004) o la presencia de líquido intraabdominal (p=0,021).
ConclusionesLa ecografía a pie de cama es una técnica frecuentemente disponible en las UCIP españolas. La formación específica para su uso es hasta el momento heterogénea pero debe servir para potenciar su implantación.
Point-of-care, bedside or clinical ultrasonography is defined as ultrasonography performed by the doctor in charge directly where the patient is for clinical assessment. It is used for addressing specific problems or questions immediately and in real time.1 Compared to ultrasonography performed by radiologists, which can provide more comprehensive and accurate information, point-of-care ultrasound usually focuses on yes/no questions to facilitate diagnosis and especially on procedural guidance.1 Furthermore, since it is easily repeatable, it can be used to assess changes in different clinical situations or conditions.
The size of paediatric patients facilitates the access of ultrasound waves to different organs while obtaining high-quality images. This fact, along with the elimination of the risks associated with the use of ionising radiation techniques, is clearly stimulating an increase in the use of ultrasonography.2,3 Decreasing costs, decreasing size and improvements in the specifications of ultrasonography systems in recent years have also been essential in the expansion of its use outside radiology units.
It has multiple applications in the field of paediatrics, which are clearly expanding.4–6 This is demonstrated by the increasing availability of ultrasound units in the paediatric emergency departments of some countries, as well as its increasingly frequent inclusion in clinical practice guidelines and training curriculums of different specialties.7–9
Paediatric critical care and emergency care are probably the fields in which the use of bedside ultrasonography by the paediatrician in charge is becoming most widespread. This is probably due to several factors, such as the immediacy of its use, the possibility of performing serial assessments, and above all the increasing number of clinical applications. More specifically, in the field of intensive care, there is evidence that ultrasonography can be used by critical care physicians to guide the performance of other techniques, such as establishing vascular access10,11 or the drainage of effusions in different locations.12 Furthermore, clinical ultrasonography can be used to answer specific questions regarding multiple organs and systems, and has demonstrated a high sensitivity and specificity in the diagnosis of various lung diseases.13 It allows the assessment of different aspects to determine the haemodynamic status of a patient, such as myocardiac contractility or blood volume,14,15 detect the presence of intra-abdominal lesions16 or assess changes in blood flow in different vital organs, such as the brain17 or kidneys.18
To date, although some studies have found clear evidence of its increasing use in adult intensive care units and paediatric emergency departments,7 only one study conducted in the United States has described its availability and the characteristics of its use in paediatric intensive care units (PICUs).19
The main objective of our study was to characterise the availability and use of point-of-care ultrasonography in Spanish PICUs. More specifically, we sought to identify the most widely used clinical applications. Our secondary objective was to determine the level of training on the use of ultrasonography in the care of critical paediatric patients of Spanish clinicians.
Materials and methodsWe conducted a multicentric cross-sectional descriptive study. We developed an online survey using the Google Forms online platform that consisted of 45 questions organised into three sections. We gathered contact information for 51 PICUs in Spain. The survey was distributed by the Sociedad Española de Cuidados Intensivos Pediátricos (Spanish Society of Paediatric Critical Care) by electronic mail to the service chief or contact person of the different paediatric intensive care units. In a second phase, we attempted to contact the units that had not completed the questionnaire by electronic mail.
The first section of the survey consisted of questions that explored the characteristics of the PICU and its activity and those of the hospital to which it belonged.
The second section explored the availability of ultrasound machines, their location, exclusive or shared use, frequency of use and use for different applications. In the last section, the questionnaire asked about the training on ultrasonography of the PICU staff including physicians and nurses, the need for training and guidelines, and the usefulness of specific training in ultrasonography.
We analysed the responses by means of the SPSS software for Mac OS X version 20.0.0 (IBM Corp, Armonk, New York, USA). We described categorical variables by the percentage of answers in each category, and continuous variables as median and interquartile range. We compared groups by means of nonparametric tests (Kruskal–Wallis, Fisher's exact and Mann–Whitney U), and defined statistical significance as a p-value of less than 0.05 in these tests.
ResultsCharacteristics of participating paediatric intensive care unitsOf the 51 identified units, 33 (64.7%) responded to the survey. Of all the submitted surveys, 60.6% had been completed by the individual in charge of the unit (chief of service, department chief or coordinator) and the rest by attending physicians. Each unit submitted the survey only once.
Of all participating units, 84.8% operated in public hospitals, 6.1% in privately managed public hospitals, and 9.1% in private hospitals; while 93.9% of all PICUs were in university hospitals.
Most PICUs (72.7%) cared exclusively for paediatric patients, while 27.3% were mixed units offering both paediatric and neonatal care. Table 1 summarises the type of patients routinely admitted to the PICUs.
When it came to the size of the surveyed units, the median number of beds was eleven (IQR, 6.5). Of all units, 51.5% had more than ten beds, 39.4% between six and ten beds and 9.1% fewer than five. The median number of admissions per year was 368 (IQR, 290); five units (5.6%) had more than 600 admissions a year, 59.4% between 300 and 600 and 25% fewer than 300. The median number of physicians on staff was seven (IQR, 3.5); 27.3% of the units had more than eight physicians on staff, 57.6% between five and eight, and 15.2% fewer than five.
Ultrasound machine availabilityOf all the PICUs, 53.1% had a dedicated ultrasound machine and the rest shared it with other units in the hospital (in 25%, the device was usually kept in the PICU and in 21.9% outside the PICU). Only two (6.1%) of the units that responded to our survey reported not having access to an ultrasound machine. We did not find an association between the availability of ultrasound systems and the number of beds, the number of physicians, the number of admissions per year or the type of patients routinely served in the unit. Of the PICUs with ultrasound machines, 43.8% had portable units, while 56.2% had large non-portable systems.
Use of clinical ultrasonographyOnly one unit reported never having used clinical ultrasonography. A total of 35.5% of the units reported using clinical ultrasonography daily, 32.3% every two or three days, 19.4% weekly and 12.9% only occasionally. The daily use of ultrasonography was more frequent in PICUs where the ultrasound unit was kept in the PICU itself as opposed to PICUs where the machine was available but usually kept outside the PICU (52.9% versus 12.5%; P=.026). Tables 2 and 3 compare the PICUs that used ultrasonography daily by their characteristics and type of patients served.
Percentage of PICUs that used ultrasonography daily by unit characteristics.
| Unit characteristics | Yes (%) | No (%) | P |
|---|---|---|---|
| Paediatrics-only ICU | 90.9 | 63.6 | .212 |
| Availability of ultrasound machine | 45.5 | 42.9 | 1 |
| Neurosurgery | 100 | 95.5 | 1 |
| Polytrauma | 90.9 | 90.9 | 1 |
| Oncology | 100 | 81.8 | .276 |
| Cardiac surgery | 63.6 | 31.8 | .136 |
| Transplants | 72.7 | 22.7 | .009 |
| ECMO | 63.6 | 13.6 | .006 |
Statistically significant results are presented in boldface.
Comparison of units that used ultrasonography daily and units that did not.
| Yes | No | P | |||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| Number of beds in PICU | 12 | 6 | 9 | 6 | .067 |
| Number of admissions/year | 462.5 | 220 | 350 | 200 | .015 |
| Number of physicians on staff | 7 | 7 | 7 | 3 | .233 |
Statistically significant results are presented in boldface.
In 29% of the PICUs, more than 75% of physicians used clinical ultrasonography regularly, in 25.8% of the units, this percentage of physicians ranged between 50% and 70%; in 29% of the units, it was used regularly by 25% to 50% of physicians, and in 16.1% of the units by fewer than 25% of physicians.
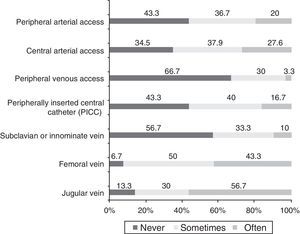
Fig. 1 represents the frequency of the use of ultrasonography to establish different types of vascular access. In most ultrasound-guided procedures for establishing central access, cannulation was performed with real-time visualisation (insertion of 74.1% of jugular vein catheters; 85.7% of femoral vein catheters; 66.7% of subclavian or innominate vein catheters; and 75% of arterial catheters), and cannulation without direct visualisation after performance of ultrasonography was a much less frequent approach (insertion of 25.9% of jugular vein catheters, 14.3% of femoral vein catheters, 26.7% of subclavian or innominate vein catheters and 25% of arterial catheters).
Table 4 shows the percentage of units that used ultrasonography to guide vascular cannulation for different purposes.
Percentage of units that used ultrasonography to guide vascular cannulation for different purposes.
| Purpose | % of units that used ultrasound |
|---|---|
| Assessment of free intraperitoneal fluid | 86.2 |
| Diagnosis and drainage of pleural effusion | 73.3 |
| Assessment of cardiac function | 72.7 |
| Diagnosis and drainage of pericardial effusion | 72.4 |
| Head ultrasound | 72.4 |
| Assessment of increased intracranial pressure | 63.3 |
| Diagnosis of pneumothorax | 50 |
| Diagnosis of other lung diseases | 46.7 |
| Assessment of blood volume | 46.7 |
| Renal ultrasound | 33.3 |
| Management of cardiorespiratory arrest | 26.7 |
| Assessment of optic nerve | 1.3 |
| Transcranial Doppler | 3.4 |
| Basic echocardiography | 3.4 |
| Assessment of airway | 3.4 |
Only a small percentage of the PICUs (18.2%) reported that all of their physicians had been specifically trained on the use of ultrasonography in the care of critical patients; 33.3% of the units reported that more than 50% had this training, 45.5% of the units reported that fewer than 50% had this training, and 3% not having trained any of the physicians. Physicians had received specific training on critical care ultrasonography in intensive care units, emergency departments or paediatric resuscitation units (68.8%) or through specific courses on the subject (18.8%). Training in adult units or radiology departments was less frequent (3.1% and 6.3%, respectively).
The presence of more than 50% of physicians with training on ultrasonography for critical patient care was not associated with any of the characteristics under study; however, it was significantly associated with greater daily use of ultrasonography (P=.033) and the use of ultrasonography for the assessment of cardiac function (P=.033), blood volume (P=.004) and free intraperitoneal fluid (P=.021).
In 36.4% of the PICUs, the nursing staff had training in ultrasonography, and 87.9% of respondents answered that they thought this training was necessary. Ninety-seven percent believed that if there were more training, point-of-care ultrasound would be used more frequently. All respondents considered that the availability of guidelines and educational materials on ultrasonography in critically ill paediatric patients in the SECIP website was helpful. They also considered that skills in ultrasonography for the care of paediatric critical patients should be part of the training of paediatricians that work in PICUs.
DiscussionPoint-of-care ultrasound is a tool used increasingly in the care of critical patients and has a clear impact on the diagnostic and therapeutic approach.2,20 Our study describes the extent to which clinical ultrasonography is used in Spanish PICUs. The results of our survey are a good reflection of the current status quo, as the response rate was high, greater than the one reported by Lambert et al. in the United States,19 and it included PICUs of very different sizes and with different types of patients.
One salient finding was that the availability of ultrasound machines was not associated with the size or level of care of the PICUs, which may be due to many different factors (the attitude of professionals, the resources of each hospital, etc.). However, a more frequent use of this technique was associated with the number of admissions per year and the type of patients usually served in the PICU, as well as with the existence of a transplant programme or the availability of ECMO. Units that had more beds used point-of-care ultrasound more frequently, but this difference was not statistically significant. A study published by Lambert et al., however, did find a clear association between the use of this technique and the number of beds in the unit, the number of admissions and the existence of paediatric intensive care training programmes.19
We ought to note that when it came to the specific applications of point-of-care ultrasound, we found that this technique has ceased to be solely used to guide other procedures and has become just another tool that contributes to the assessment of multiple organs and systems. The ability to quickly and directly address specific questions concerning the patient's haemodynamic, respiratory or neurologic status, among others, helps clinical decision-making in the daily practise of paediatric intensivists. In our study, we found a high proportion of PICUs that used point-of-care ultrasound for purposes other than cannulation (more than 70% for many uses). This percentage exceeded the 50% reported in the study Lambert et al.19
The use of ultrasonography can reduce the risk of complications in certain procedures, such as vascular cannulation or the assessment of effusion (mainly pleural and pericardial). We found it surprising that while the percentage of units that reported using ultrasonography to guide these procedures in our study was high, its use is not yet widespread, despite the mounting scientific evidence and international recommendations that support it.21,22 More specifically, when it came to the use of ultrasound for guiding vascular cannulation, a high percentage of the PICUs (between 30% and 50%, depending on the type of vascular access) reported ultrasound was only used sometimes. Likewise, the frequent use of ultrasound to guide vascular cannulation only reached approximately 60% when it came to placement of jugular vein catheters. Thus, the use of ultrasound for guiding these procedures needs to be promoted.
As one would expect, we found that ultrasonography was used more frequently in PICUs with staff trained in its use. Given the high availability of ultrasound machines, we think that the development of a structured training programme in ultrasonography is essential.
Several studies have analysed the status quo of specialised training in point-of-care ultrasound in intensive and emergency care units in the United States.7–9,23,24 In the United States, training on point-of-care ultrasound is part of the educational curriculum of paediatric intensive care and paediatric emergency care subspecialties. In Spain, these subspecialties are not officially recognised in paediatrics, although most subspecialties have established educational curricula. We believe that basic competencies in the use of point-of-care ultrasound should be included in the learning objectives of paediatricians that will be working in paediatric intensive care settings, as is the case of other techniques such as incubation care or vascular cannulation. This has already been done in other countries, such as Canada, through consensus meetings.25
Our study shows that there is large proportion of physicians in the surveyed PICUs that had training on point-of-care ultrasonography (in up to one third of the PICUs, up to 50% of the medical staff had training in ultrasonography). This proportion was higher than the one found by the study by Lambert et al.19 from 2011, in which the percentage of institutions with formal training did not reach 30%. Most respondents in our study considered that the availability of online educational resources on clinical ultrasonography in paediatric patients is useful, and that paediatricians that care for critical paediatric patients should be trained on this technique. We believe that specific training in point-of-care ultrasound is essential to standardise its use and reduce errors in its interpretation.
LimitationsThe main limitation of our study, which applies to all voluntary surveys, is that it does not reflect reality directly, but rather the views of those surveyed. Despite the high response rate (64.7% of the identified units), we cannot rule out the possibility that the PICUs that responded to the survey were those that use ultrasonography more frequently.
On the other hand, when it came to training on point-of-care ultrasound, there were no established criteria to assess the quality and homogeneity of the training received, so it may have varied widely between units.
ConclusionsPoint-of-care ultrasound is a frequently used technique in Spanish PICUs. Ultrasound units are available at a high percentage of the PICUs independently of their level of care. Point-of-care ultrasound was used not only to guide vascular cannulation or drainage placement, but also for the assessment of different organs and systems to complement physical examination and monitoring. Specific training is irregular and should be an essential strategy to promote its use.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank the representatives of every participating unit for collaborating in the collection of data through the online survey, which we proceed to list alphabetically: Amalia Martínez Antón (Hospital Universitario Fundación Jiménez Díaz), Antonio Bonillo Perales (Complejo Hospitalario Torrecárdenas), Antonio Jiménez Bravo de Laguna (Complejo Hospitalario Universitario Insular Maternoinfantil de Canarias), Antonio Rodríguez Núñez (Complexo Hospitalario Universitario de Santiago), Asunción Pino Vázquez (Hospital Clínico Universitario de Valladolid), Begoña Arias Novas (Hospital Universitario Sanitas La Zarzuela), Carlos Solís Reyes (Hospital Universitario Nuestras Señora de la Candelaria), Concha Goñi Orayen (Complejo Hospitalario de Navarra), Corsino Rey Galán (Hospital Universitario Central de Asturias), Roberto Reig Sáenz (Hospital General Universitario de Alicante), Eduard Carreras González (Hospital de la Santa Creu i Sant Pau), Ender Oñate Vergara (Hospital Universitario Donostia), Francisco José Cambra Lassaloa (Hospital Sant Joan de Déu), Gerardo Romera Modamio (Hospital Universitario HM Madrid-Montepríncipe), Guillermo Milano Manso (Hospital Regional Universitario de Málaga), Irene Centelles Sales (Hospital General Universitario de Castellón), Javier Pilar Orive (Hospital Universitario de Cruces), Jesús de la Cruz Moreno (Complejo Hospitalario de Jaén), Joan Ballcels Ramírez (Hospital Vall d’Hebron), José Luis Vázquez Martínez (Hospital Universitario Ramón y Cajal), Juan Carlos de Carlos (Hospital Universitario Son Espases), Luis Moreno Fernández (Hospital San Rafael), Luis Renter Valdovinos (Hospital Universitario Parc Tauli), Manuel Ortiz Pallarés (Hospital Xeral de Vigo), Mario Sánchez Fernández (Hospital Universitari Dr. Josep Trueta), Montserrat Nieto Moro (Hospital Infantil Universitario Niño Jesús), Paula Madurga Revilla (Hospital Universitario Miguel Servet), Rafael González Cortés (Hospital General Universitario Gregorio Marañón), Susana Jaraba Caballero (Hospital Universitario Reina Sofía de Córdoba), Susana Reyes Domínguez (Hospital Clínico Universitario Virgen de la Arrixaca) and Sylvia Belda-Hofheinz (Hospital Universitario Doce de Octubre).
Please cite this article as: González Cortés R, Renter Valdovinos L, Coca Pérez A, Vázquez Martínez JL. Ecografía en el punto de cuidado en las unidades de cuidados intensivos pediátricos españolas. An Pediatr (Barc). 2017;86:344–349.