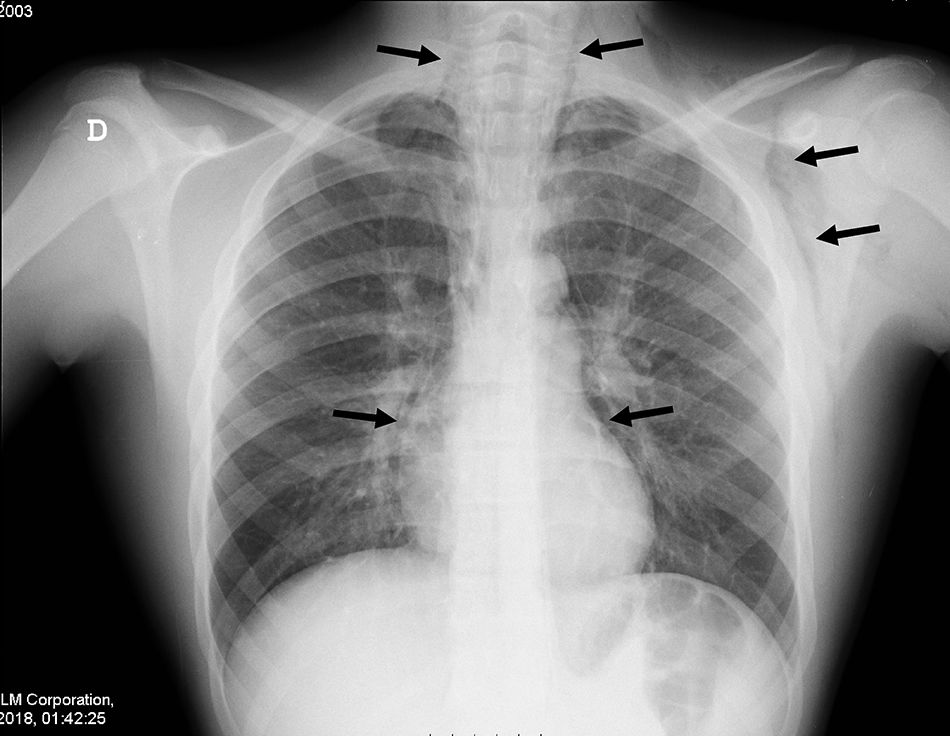
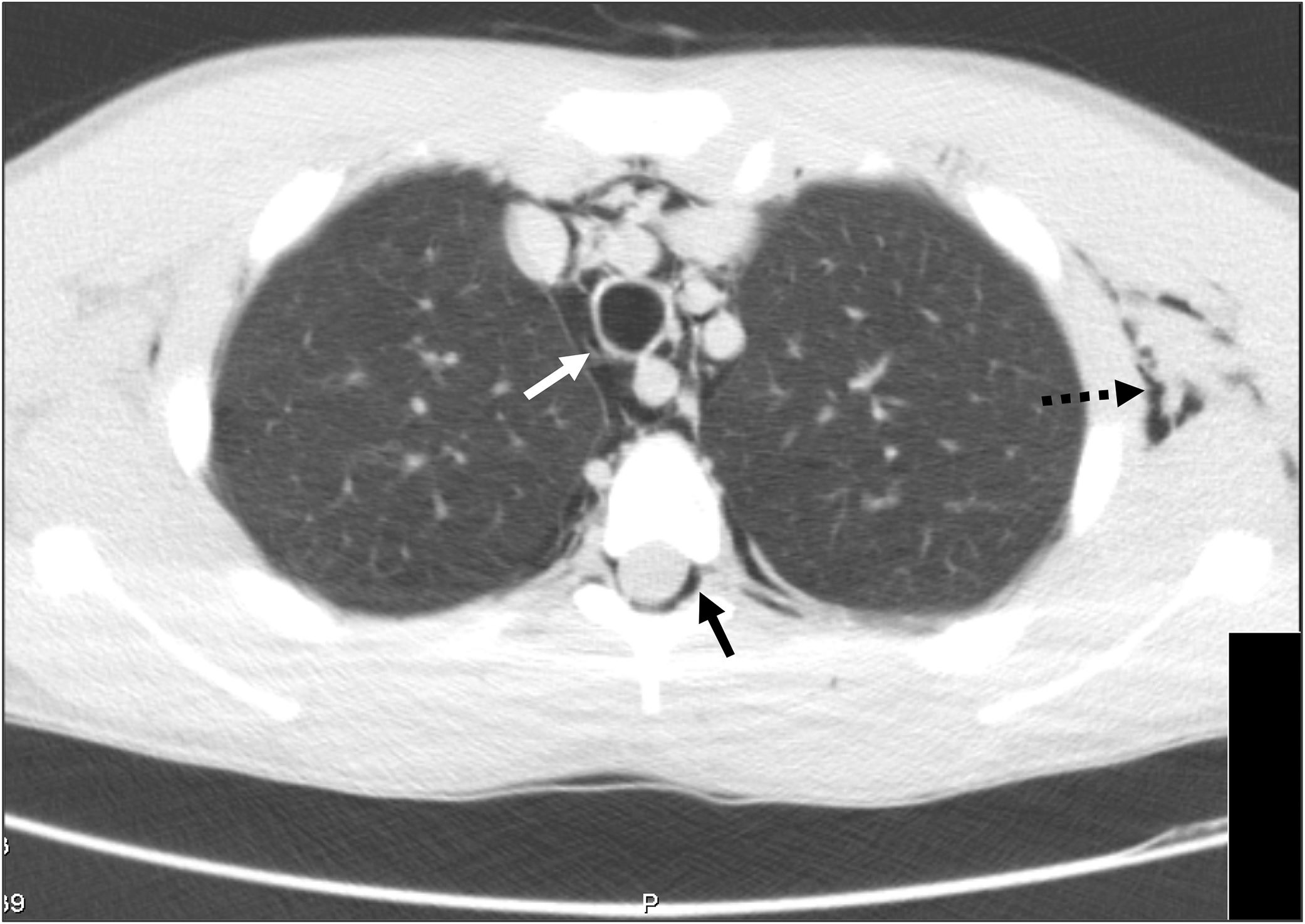
A 14-year-old boy with asthma presented to the emergency department with dyspnoea, persistent cough and left-sided cervical pain that did not improve after administration of a short-acting β2-agonist and oral corticosteroid. He was afebrile, with an oxygen saturation of 92%, a respiratory rate of 24 breaths/min, chest retractions and subcutaneous crepitus at the level of the left armpit and neck. Auscultation revealed bilateral decreased breath sounds and biphasic wheezing. The rest of the physical and neurological examination was normal. A plain radiograph of the chest revealed pneumomediastinum associated with subcutaneous emphysema and no signs of pneumothorax (Fig. 1). The patient was admitted and treated with analgesics, high-concentration oxygen (15L/min), inhaled salbutamol and ipratropium bromide, and intravenous methylprednisolone. Computed tomography revealed air within the spinal canal in addition to a moderate-sized emphysema and pneumomediastinum (Fig. 2). The patient was discharged home after 7 days.
Spontaneous pneumomediastinum results from a sudden increase in intra-alveolar pressure during acute or chronic pulmonary disease, causing alveolar rupture and a leak of air that gives rise to the interstitial emphysema.1 It is uncommon in the paediatric age group, and acute asthma is the most frequent cause in adolescents. The triad of acute chest pain under the sternum, subcutaneous emphysema and dyspnoea of varying severity allows its diagnosis.1 Pneumorrhachis occurs when air dissects from the posterior mediastinum or the retropharyngeal space through the neural foramens into the epidural space.2,3 It does not generally cause neurologic symptoms and resolves spontaneously in 98% of cases, and it is now identified thanks to the increased use of computed tomography.2 Spontaneous pneumomediastinum is usually benign and self-limiting, and the same approach with supportive care including clinical monitoring, rest and analgesia and treatment of the underlying disease is recommended for all patients, even in the unlikely event of concomitant pneumorrhachis.1–3
Please cite this article as: Brandão Silva J, Lira J, Ferreira G, Rodrigues J. Neumorraquis: un hallazgo en el neumomediastino espontaneo. An Pediatr (Barc). 2019;90:319–320.