Absence of the pericardium (AoP) is a rare anomaly usually detected by chance. Its incidence is less than 1 case per 10 000 inhabitants.1 It is classified based on its extension (complete or partial) and position (left, right or bilateral), and complete left-sided defects are the most frequent form (70%).2–4 In 30%–50% of cases, AoP is associated with congenital heart defects such as tetralogy of Fallot, atrial septal defect, patent ductus arteriosus, mitral valve defects or sinus venosus defects with partial anomalous pulmonary venous drainage3 as well as pulmonary malformations, Marfan syndrome, VATER syndrome and Palliester–Killian syndrome.2 Although most cases are asymptomatic, patients with partial absence of the pericardium (PAoP) may experience chest pain, palpitations, syncope or even sudden death secondary to herniation of cardiac structures through the pericardial defect.
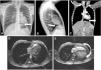
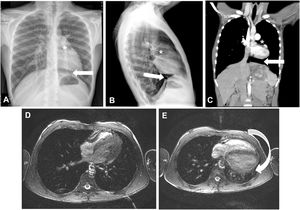
We present 2 cases of incidental finding of AoP. The first corresponded to a patient referred at the age of 13 years due to abnormal position of the heart in the chest radiography (CXR). He was symptomatic and did not have any relevant personal or family history. The physical examination was normal. The electrocardiogram (ECG) (Fig. 1A) showed sinus bradycardia with right axis deviation (+112 °), incomplete right bundle branch block (IRBBB), slow R wave progression, nonspecific intraventricular conduction delay (QRS duration of 96 ms) and abnormal repolarization (inverted T waves in V1–V4, transitioning in V5 and positive in V6). The CXR showed lung interposition between the aorta and pulmonary artery (PA), leftward shift of the heart with no visible right heart border and lung interposition between the left diaphragm and the base of the left heart (Fig. 2A–B). After performing an echocardiogram, PAoP was suspected on account of the posterior and leftward shift of the apex, paradoxical septal motion and apparent dilatation of the right ventricle due to leftward cardiac displacement (Fig. 1C; Supplemental material Appendix B, videos 1 and 2). Computed tomography (CT) and magnetic resonance imaging (MRI) findings confirmed the diagnosis (Fig. 2C–E). His exercise test was normal. As the patient was asymptomatic, a conservative approach was chosen. He has remained asmptomatic with no complications after 7 years follow-up.
(A–C) Chest radiography, posteroanterior (A) and lateral (B); cardiac CT (C); leftward shift of the heart with lung interposition between the aorta and the pulmonary artery (*) and interposition of lung parenchyma between the left diaphragm and the border of the base of the left heart (arrow). (D) Cardiac MRI with the patient in the right lateral decubitus position. (E) Cardiac MRI with patient in supine position showing posterior shift of the cardiac silhouette (arrow).
The second patient was referred at the age of 5 years due to deviation of the heart in the CXR. During surveillance, she was diagnosed with Behcet disease. She was asymptomatic from the cardiac point of view and she did not have any other relevant personal or family history. She had normal physical examination. The ECG (at the age of 15 years, Fig. 1B) revealed mild right axis deviation (+94°), IRBBB, poor R wave progression, nonspecific intraventricular conduction delay (QRS duration of 98 ms) and abnormal repolarization (inverted T waves in V1–V3, transitioning in V4 and positive in V5–V6). The CXR and echocardiogram (supplementary material Appendix B, videos 3 and 4) revealed the same features described in patient 1. Her diagnosis was confirmed by MRI. She had a normal exercise test. A conservative management was chosen in view of the absence of symptoms. She has remained asymptomatic with no evidence of complications after 13 years of follow-up.
Although AoP is a rare disease, it is important to keep a high level of suspicion, mainly because patients with PAoP, in addition to being symptomatic more frequently, are at risk of herniation and strangulation of the left ventricle through the pericardial defect and, therefore, of sudden death.2,3,5
CXR, ECG, echocardiogram and CT are useful for diagnosis of AoP. However, the gold standard is MRI, which in black blood fast spin echo and steady-state free precession sequences evinces cardiac indentation at the location of the defect, interposition of lung tissue between the aorta and the PA or between the diaphragm and the base of the heart and leftward and posterior displacement of the heart. A rotation angle greater than 60° between the anterior-posterior line passing through the vertebral body and left ventricle main axis in the end-diastolic phase of the axial cine stack offers a good sensitivity for detection of left ventricular AoP.6
Although there is no global consensus on the management of these patients, close follow-up and monitoring for complications is recommended in asymptomatic patients in whom AoP is an incidental finding and in the case of complete bilateral or left-sided AoP. Surgery is reserved for patients with PAoP or at risk of complications.2,5
In conclusion, we have presented 2 cases of incidental diagnosis of AoP, a disease that is difficult to diagnose due to its rarity and usually asymptomatic, whose early detection is vital due to its potential association with sudden death. Although MRI is the gold standard of diagnosis, the abovementioned imaging investigations can also be useful. Despite the absence of a global consensus, the approach to treatment is conservative, reserving surgery for patients with symptoms or with PAoP at risk of complications.
FundingThis research did not receive any external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Brunet-Garcia L, Carretero Bellon JM, Pérez-Casares A, Prada Martínez FH, Sánchez-de-Toledo J, Ausencia parcial de pericardio: ¿únicamente un hallazgo incidental? Anales de Pediatría. 2022;96:540–542.