The aim of this study was to identify the commonest referrals to a paediatric orthopaedic outpatient clinic and, therefore, to be able to improve the paediatric residency programme in managing musculoskeletal problems.
Material and methodsDemographic data, referrals and final diagnosis were collected prospectively on all patients that were evaluated in a paediatric orthopaedic outpatient clinic.
ResultsThe majority of referrals were to evaluate musculoskeletal pain (37%), foot deformity (20%), spine deformity (15%), walking pattern (11%), alignment of the lower limbs (4%), and development of the hip (4%). A normal physical examination or a normal variation was observed in 42% of patients. A mild condition was observed in 17% of patients that should have only been referred to a paediatric orthopaedic clinic after failing to resolve pain with anti-inflammatories or physiotherapy. A mild deformity that only needed treatment if it became symptomatic was seen in 8% of patients.
ConclusionsThe majority of referrals were due to a normal variation or mild conditions that only required symptomatic treatment. Paediatric residency programmes do not reflect the prevalence of musculoskeletal conditions in clinical practice.
El objetivo de este estudio fue conocer los motivos de consulta más frecuentes en una consulta de Traumatología Infantil de un Centro de Especialidades y así poder mejorar el programa de formación de los residentes de Pediatría en el manejo de problemas músculo-esqueléticos.
Material y métodosSe recogieron prospectivamente los motivos de consulta, la edad, el sexo y el diagnostico final de todos los pacientes menores de 15 años derivados a una consulta específica de Traumatología Infantil de un Centro de Especialidades.
ResultadosLos motivos de consulta más frecuentes fueron el dolor músculo-esquelético (37%), valorar una posible deformidad de los pies (20%), una posible deformidad de la columna (15%), el patrón de marcha (11%), la alineación de los miembros inferiores (4%) y el desarrollo de la cadera (4%). El 42% de los pacientes presentaron una exploración normal o una variante de la normalidad. El 17% de los pacientes presentaron una patología que únicamente requiere ser valorada por parte de Traumatología Infantil si un tratamiento previo con antiinflamatorios no esteroideos o rehabilitación no resuelve la sintomatología. El 8% presentaba una deformidad que solo requiere tratamiento si es sintomática.
ConclusionesLa mayoría de las consultas correspondieron a variantes de la normalidad o a condiciones leves que solo precisan tratamiento sintomático. El programa de formación de la residencia de Pediatría no refleja la prevalencia de los problemas músculo-esqueléticos en la práctica clínica diaria.
Musculoskeletal disorders are very prevalent and account for 20–30% of paediatric primary care visits.1 For example, 6% of paediatric visits are due to musculoskeletal pain.2 However, this high clinical prevalence is not reflected in paediatric residency programmes nor in medical school curricula. At present, only 2.3% of the curriculum time of medical students is devoted to the study of musculoskeletal problems.3 Training in residency programmes is no better, so that when final-year paediatrics residents are asked about their level of comfort in treating various medical problems in the paediatric age group, they report the lowest levels of comfort in the management of musculoskeletal problems.4 As a consequence, in most cases the paediatrician chooses to refer the patient to the paediatric orthopaedist, who becomes the de facto primary care physician for children with musculoskeletal complaints.5
As of now, preventing referrals is not the solution, as there is evidence that when it comes to certain disorders, over half of the cases are misdiagnosed if the patient is not seen by a paediatric orthopaedist.6 Delayed or incorrect diagnoses can result in permanent disabilities for the patient or a vast increase in costs for the healthcare system.7 We need to improve paediatrics residency training in the management of musculoskeletal problems in order to achieve correct and early diagnoses, which would result in reduced costs and better outcomes.
The aim of this study was to determine the most frequent reasons for referral to our paediatric orthopaedic outpatient clinic. This would enable the development of a training programme for paediatrics residents on the most common orthopaedic conditions found in clinical practice.
Patients and methodsWe conducted a prospective descriptive study between September 2012 and September 2013 in the paediatric orthopaedics office of an outpatient specialty clinic affiliated with our hospital. The outpatient clinic where these paediatric orthopaedic visits are held belongs to a tertiary care hospital in a health area that covers a population of 503175 inhabitants (66109 of whom are younger than 14 years) through 20 outpatient health care centres. The orthopaedics office that participated in this study only serves patients younger than 15 years referred to the Orthopaedics and Orthopaedic Surgery service. However, the Orthopaedics and Orthopaedic Surgery service covers another 26 weekly shifts at the four outpatient specialty clinics for both children and adults. Thus, this particular paediatric orthopaedics office is not the only site where paediatric patients can receive care, and it also offers care to paediatric patients from other health care areas referred to our clinic by the centralised scheduling centre of our autonomous community. Office hours were held by a single specialist in orthopaedics and orthopaedic surgery that completed a paediatrics orthopaedic surgery fellowship at a children's hospital affiliated to the University of California (United States) and is part of the team at the paediatric orthopaedics department of our hospital (LM). Thus, the study included patients less than 15 years of age referred to our paediatric orthopaedics office in an outpatient specialty clinic affiliated with our hospital. We excluded patients who sought care for traumatic injuries. We collected demographic data, the reason for referral, and the final diagnosis given by the paediatric orthopaedist.
ResultsBetween September 2012 and September 2013, 3174 patients less than 15 years of age received care in the shifts that the Orthopaedics and Orthopaedic Surgery department covers in the outpatient specialty clinics in our health area. Of these patients, 455 younger than 15 years referred from primary care were seen at the PTRA22 office for a non-traumatic condition. These were the 455 patients included in this study.
Patients were referred from 37 health care centres. Eighty-eight came from centres that belong to our health area. The percentage of patients referred from each healthcare centre ranged between 0.3% and 16%.
Table 1 gathers the demographic data for our sample. Ninety-one percent of referrals were made to assess musculoskeletal pain (37%), foot deformities (20%), spinal deformities (15%), gait patterns (11%), lower limb alignment (4%) or hip development (4%). The most frequent reasons for referral varied by age group: in the first year of life, it was assessment of hip development; in toddlers and early childhood, assessment of a foot deformities or gait abnormalities; and in mid-childhood and adolescence, assessment of musculoskeletal pain (Table 2).
Demographic characteristics of the sample.
| Number of patients | 455 |
| Sex | |
| Male | 202 |
| Female | 253 |
| Age, years±SD | 9.1±8.4 |
| Patients by age group, mean±SD, years | |
| Infancy | 31±0.5 |
| Toddlerhood (1–3 years) | 45±2.1 |
| Preschool (3–6 years) | 69±4.2 |
| Middle childhood (6–12 years) | 167±9.2 |
| Adolescence (>12 years) | 143±13.9 |
Percentage of patients that sought care by reason for referral and age group.
| Infancy | Toddlerhood | Preschool | Middle childhood | Adolescence | |
|---|---|---|---|---|---|
| Musculoskeletal pain | 6% | 14% | 17% | 43% | 51% |
| Foot deformity | 13% | 34% | 40% | 20% | 7% |
| Gait pattern | 0% | 32% | 13% | 12% | 3% |
| Lower limb alignment | 3% | 7% | 11% | 3% | 2.5% |
| Hip development | 50% | 2% | 0% | 0% | 0% |
| Spinal deformity | 0% | 0% | 4% | 15% | 27% |
| Bulge | 3% | 2% | 4% | 3% | 3% |
| Limited mobility of the thumb | 3% | 5% | 3% | 0.5% | 0% |
| Chest deformity | 3% | 0% | 1% | 2% | 2% |
| Other | 19% | 4% | 7% | 1.5% | 4.5% |
The incidence of musculoskeletal pain increased with patient age, and it affected school-aged children and adolescents most frequently. The location of the pain also varied with age: the most frequent location was the foot in school-aged children and the knee in adolescents. Table 3 shows the most frequent diagnoses in patients that sought care for musculoskeletal pain.
Most frequent diagnoses in patients referred for musculoskeletal pain, their percentages, and the mean age at the time of referral.
| Percentage | Mean age±SD | |
|---|---|---|
| Back pain | 14 | 12±3 years |
| Patellofemoral pain | 11 | 13±2.3 years |
| Sever's disease | 9 | 10±2.4 years |
| Osgood–Schlatter disease | 8 | 13±1 years |
| Growing pains in lower limbs | 8 | 6±3.9 years (median 4.2) |
| Ankle instability | 4 | 10±3.8 years |
| Accessory navicular bone | 4 | 10±4.6 years |
| Tarsal coalition | 4 | 11±2.8 years |
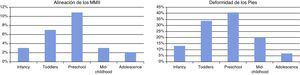
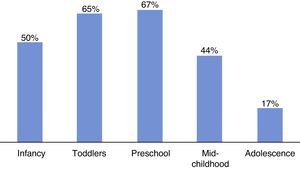
In 42% of the patients, the physical examination was normal (10%) or revealed normal variants: angular (4%) or rotational (9%) deformities of the lower limbs within the normal range, postural deformities of the feet within the normal range (14%), growing pains (3%), postural kyphosis (1%) and leg length discrepancy of less than 1cm (1%) (Fig. 1). The percentage of patients that had normal variants was higher in middle childhood and preschool age (Fig. 2).
The normal course of development of lower limb alignment (there is a physiological genu valgum between 2 and 8 years of age that peaks between 3 and 4 years of age) correlates with a high number of referrals for the assessment of the lower limbs in early childhood and preschool age (left chart). The normal development of the footprint,12 with the presence of flat foot in 44% of children between 3 and 6 years of age,13 is associated with considerable concern for static foot structure in early childhood and preschool age (right chart).
Incidence of normal variant diagnosis in different age groups. Approximately 90% of the patients with normal variants (rotational or angular abnormalities in the lower limbs, abnormalities in static foot structure) improve spontaneously in the first 8–10 years of life, which accounts for the decrease in this diagnosis observed in adolescence (17%).
Seventeen percent of patients had mild conditions that require assessment by a paediatric orthopaedist only when treatment with anti-inflammatory agents and rehabilitation has failed: self-limiting osteochondroses (Sever 3%, Osgood–Schlatter 3%, Sinding–Larse–Johanson <1%, or apophysitis of the fifth metatarsal base <1%); back pain with no abnormal findings in the examination (6%); transient synovitis of the hip (0.4%); symptomatic accessory navicular bone (1%), and tendinitis, periostitis, sesamoiditis, trochanteritis or coccydynia (3%).
Eight percent of patients had a deformity that only requires treatment if symptomatic: clinodactyly in the feet, claw foot, overlapping fifth toe, tailor's bunion, hallux valgus, hallux interphalangeus, or ganglion or Baker's cysts.
The rest of the patients had one of the following disorders: scoliosis (9%), anterior knee pain syndrome (4%), metatarsus adductus, tarsal coalition, cavovarus foot, delta phalanx, trigger finger, nonspecific limp, ankle instability, patellar instability, shoulder instability, meniscus tear, knee osteochondritis dissecans, osteochondroma, angioma, idiopathic toe walking, torticollis, scapular dyskinesis, genu valgum in patients more than 10 years of age, genu varum in patients more than 18 months of age, fibrous cortical defect, postural plagiocephaly, calcaneovalgus foot or immature hip.
DiscussionThere are established guidelines and protocols for the referral of patients from primary care to a paediatric orthopaedics clinic.8 However, these guidelines have proved ineffective, as paediatricians continue to refer patients with conditions that they should treat themselves.1,8,9 McCarthy et al. declared that 75% of the patients referred to their office came from the primary care paediatrician, and that 95% of referrals were for mild conditions or normal variants.9 The study of Hsu et al. reported that 47% of the patients referred to their office should have been treated by their paediatrician.8 The rate of appropriate referrals to the paediatric orthopaedist based on the recommendations of the American Academy of Pediatrics ranges from 14% to 35% in the published literature.1,8 In our series, 67% of the referrals corresponded to normal variants or mild conditions that should be managed, at least initially, by the paediatrician.
We believe that the failure of the referral guidelines does not stem from an unwillingness to treat these patients on the part of paediatricians, but to a lack of training, both during medical school and in residency programmes, on the development of the musculoskeletal system during growth and on the most common musculoskeletal disorders.3 The official curriculum for the paediatrics specialty and its specific areas published by the BOE does not include a mandatory rotation in paediatric orthopaedics.10 This gap in training results in a lack of confidence of paediatricians in the management of these patients,4 so that paediatric orthopaedists become the primary care physician for musculoskeletal disorders.5
Thus, paediatrics residents must be trained on the normal variants that occur in the development of the musculoskeletal system, and also on the most common mild pathologies affecting this system. In our study, we found that angular or rotational problems of the lower limb and abnormalities of the static foot structure within normality are a frequent source of concern in parents. These reasons for referral occur more frequently in age ranges where genu valgum is physiological or in which there is a higher prevalence of flexible flat foot.11,12 The official curriculum for the paediatrics specialty and its specific areas establishes that the primary objectives of care are “evaluating normality in children and adolescents through the various stages of development by means of specific assessment methods” followed by “the identification of deviations from normality by means of the appropriate diagnostic methods”.10 Thus, paediatricians must be familiar with the normal development of the lower limbs through childhood to be able to reassure and advise parents on this subject.11–16
Similarly, our study found that musculoskeletal pain was the most frequent reason for referral, especially in schoolchildren and adolescents. Most of the causes of musculoskeletal pain involve mild disorders that only require symptomatic treatment and rehabilitation, as well as informing the parents of the self-limited course and lack of sequelae at skeletal maturity of many of these causes.
There are limitations to this study concerning the representativeness of its sample due to its size, to the fact that the paediatric orthopaedics specialty clinic is not the only site offering care to paediatric patients in our health area (only 14% of patients that received care through the Orthopaedics and Orthopaedic Surgery service were seen in our clinic) and because the sample consists only of patients from our health area. Furthermore, we need to emphasise that the cited studies were conducted in countries with health systems that differ from Spain in the way patients are referred from primary care to specialised paediatric orthopaedic care, and thus, comparing figures poses challenges. However, we do not believe that there is a referral bias in any of the paediatricians. The percentage of patients that corresponded to each healthcare centre ranged between 0.3% and 16%. Sixty-four percent of patients came from six healthcare centres that serve 39% of the population under 15 years of age in our health area, while 15% of the patients came from nine healthcare centres that serve 41% of the population under 15 years of age in our health area. Considering that four outpatient specialty clinics in our health area offer orthopaedic surgery and orthopaedics services, we believe that the differences in the percentages of referrals from the different healthcare centres are due to their distribution among the different outpatient specialty clinics.
In conclusion, most referrals from paediatrics departments to a paediatric orthopaedics specialist are due to normal variants or to mild pathologies that only require symptomatic treatment. An improvement in the paediatric residency training on the development of the musculoskeletal system through childhood and on the most prevalent mild musculoskeletal disorders could decrease the number of referrals or requested imaging tests, which would reduce healthcare costs and save the parents unnecessary worry and healthcare visits.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Moraleda L, Castellote M. Motivos de derivación a una consulta ambulatoria de Traumatología Infantil. An Pediatr (Barc). 2015;83:89–93.