Influenza is a generally a benign disease, but occasionally it can cause serious complications. There is controversy about the benefits of antiviral treatment.
ObjectivesTo provide some recommendations on the treatment with oseltamivir in paediatric patients with influenza, based on the best data available and valid in our environment.
MethodsThe Respiratory Infections Group of the Spanish Society of Paediatric Infectious Diseases carried out a review of the literature. The findings were analysed using the GRADE methodology, and recommendations were made.
ResultsThe systematic use of diagnostic tests for influenza in the outpatient setting, or in the emergency room, in immunocompetent patients with a compatible clinical picture is not recommended. If the aim is to prevent serious events, the use of antivirals is not recommended for the vast majority of healthy and asthmatic patients with influenza or suspected seasonal flu. The systematic use of oseltamivir in patients admitted to hospital with influenza is not recommended. Oseltamivir treatment is recommended in any patients with influenza and pneumonia or severe illness, and critically ill patients, especially during the first 48h of illness. The treatment of patients with risk factors is recommended, considering their underlying disease. Influenza vaccination, together with basic isolation measures, continue to be the main tool in the prevention of influenza.
ConclusionIn some situations, there are sufficient data to issue clear recommendations. In other situations, the data are incomplete, and only allows weak recommendations.
La gripe es una enfermedad generalmente benigna, pero en ocasiones puede ocasionar complicaciones graves. Existe controversia sobre los beneficios del tratamiento con antivirales.
ObjetivosProporcionar unas recomendaciones sobre el tratamiento con oseltamivir en pacientes pediátricos con gripe, basadas en los mejores datos disponibles y válidas en nuestro medio.
MétodosEl Grupo de Infecciones Respiratorias de la Sociedad Española de Infectología Pediátrica llevó a cabo una revisión de la bibliografía. Los hallazgos se analizaron mediante la metodología GRADE, y se elaboraron unas recomendaciones.
ResultadosNo se recomienda el uso sistemático de pruebas diagnósticas para la gripe en el ámbito ambulatorio y en urgencias hospitalarias en pacientes inmunocompetentes con un cuadro clínico compatible. No se recomienda el uso de antivirales a la gran mayoría de los pacientes sanos y asmáticos con gripe o sospecha de gripe estacional, si el objetivo es prevenir eventos graves. No se recomienda el uso de oseltamivir de forma sistemática en pacientes hospitalizados con gripe. Se recomienda tratar con oseltamivir a los pacientes con gripe y neumonía o enfermedad grave o a los pacientes críticos, especialmente durante las primeras 48h de enfermedad. Se recomienda el tratamiento de los pacientes con factores de riesgo, teniendo en cuenta su enfermedad de base. La vacunación antigripal, junto a las medidas básicas de evitación, continúan siendo la principal herramienta en la prevención de la gripe.
ConclusiónEn algunas situaciones hay datos suficientes para emitir recomendaciones claras. En otras situaciones los datos son incompletos y solo permiten hacer recomendaciones débiles.
Influenza is an acute respiratory disease caused by the influenza virus, of which 2 subtypes predominate in human infections: A and B. Every year it affects 10–20% of the population, of which 20–40% are children and adolescents. In the latter, viral loads are higher, so they can shed virus for a longer time, approximately from 3 to 5 days before onset of symptoms to 10 to 14 days after onset. The disease is highly contagious through respiratory droplets disseminated by coughing and sneezing. Children are the main vector of disease transmission. Influenza is usually a clinical diagnosis, which may be easy or challenging to reach depending on the circumstances (epidemic season, presentation and age of the patient). Its symptoms are nonspecific, could be caused by other viruses, and may vary based on the age of the patient. The symptoms classically associated with influenza are fever, cough, nasal obstruction, nasal discharge, pain swallowing, myalgia, headache and occasionally gastrointestinal symptoms. In infants, especially those aged less than 6 months, the presentation may be indistinguishable from an episode of sepsis, with fever, irritability and food refusal.
The course of influenza is usually benign, and its most frequent severe manifestations are otitis media, bronchiolitis, pneumonia, and other forms characterised by respiratory distress and wheezing. Influenza follows a seasonal pattern with outbreaks usually occurring in winter.
The management of influenza is based on supportive and symptomatic care, with the additional use of antivirals, chiefly neuraminidase inhibitors, under specific circumstances.
The World Health Organization (WHO), the American Academy of Pediatrics (AAP), the Centers for Disease Control (CDC) and numerous public health institutions recommend the use of neuraminidase inhibitors for treatment and prevention of seasonal and pandemic flu, especially since the 2009 pandemic, in individuals with personal or occupational risk factors.1–3
The summary of product characteristics of oseltamivir specifies that it is indicated “in adults and children including full term neonates who present with symptoms typical of influenza, when influenza virus is circulating in the community. Efficacy has been demonstrated when treatment is initiated within two days of first onset of symptoms. [Also as] post-exposure prevention in individuals 1 year of age or older following contact with a clinically diagnosed influenza case when influenza virus is circulating in the community”.
However, there is still considerable controversy regarding its usefulness in everyday clinical practice.
Our aim was to offer clinicians recommendations that are valid in our geographical region and aimed at the population of individuals under 18 years of age based on the highest-quality evidence available, to be developed through the performance of a systematic review and analysis of the literature applying the Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology.
MethodsThis article summarises the recommendations. The supplemental material, available online, presents the rationale and references for the responses given to the questions of interest applying the GRADE methodology.4,5
We chose to use the GRADE approach to develop these recommendations because it is one of the most rigorous methods for establishing evidence-based guidelines for decision making.
We established a subgroup within the Working Group (WG) on Respiratory Diseases of the Sociedad Española de Infectología Pediátrica (Spanish Society of Paediatric Infectious Disease, SEIP). We appointed a coordinator for the project, who selected the experts for the panel that would develop the consensus document.
The panel started by defining the relevant variables by asking questions of interest. Potential clinical questions and the most relevant variables were found through brainstorming. Questions were formulated based on the identified variables following the Population-Intervention-Comparison-Outcome (PICO) model. We surveyed the entire WG. Fourteen out of it 15 members rated the relevance of the variables on a scale from 1 to 9. The variables rated 6 or higher were defined as “very important” (score of 6) or “key variables” (score of 7–9) and were included in the evaluation performed by the panel. All the proposed questions but 1 reached the 6-point threshold for inclusion.
Eight of the members of the panel made a review of the literature by searching the Cochrane, EMBASE and PubMed databases for articles published in the past 5 years focused on the variables of interest, with particular emphasis on high-quality studies. These authors specifically searched for articles published after review articles. The quality of the studies was determined based on the study design (high: meta-analyses and clinical trials, low: observational studies) and finetuned based on factors that increased or decreased the quality of the evidence. The quality categories were “high”, “moderate”, “low” and “very low”, assigned based on the limitations and inconsistencies of the study and whether the evidence was direct or indirect.
The questions that had been formulated and then selected were addressed using the evidence collected by the panel in the literature review. After this, the panel drafted the recommendations (strong/weak, in favour/against). The panel contacted some of the authors of clinical trials to request clarifications. The strength of the recommendation was based on the confidence of the panel that the benefits of the recommended action exceeded its risks (side effects, drug resistance) and vice versa.
At least 75% of the panel had to agree on a recommendation for it to be included as such in the document. The entire WG had the option to comment on the document and suggest corrections.
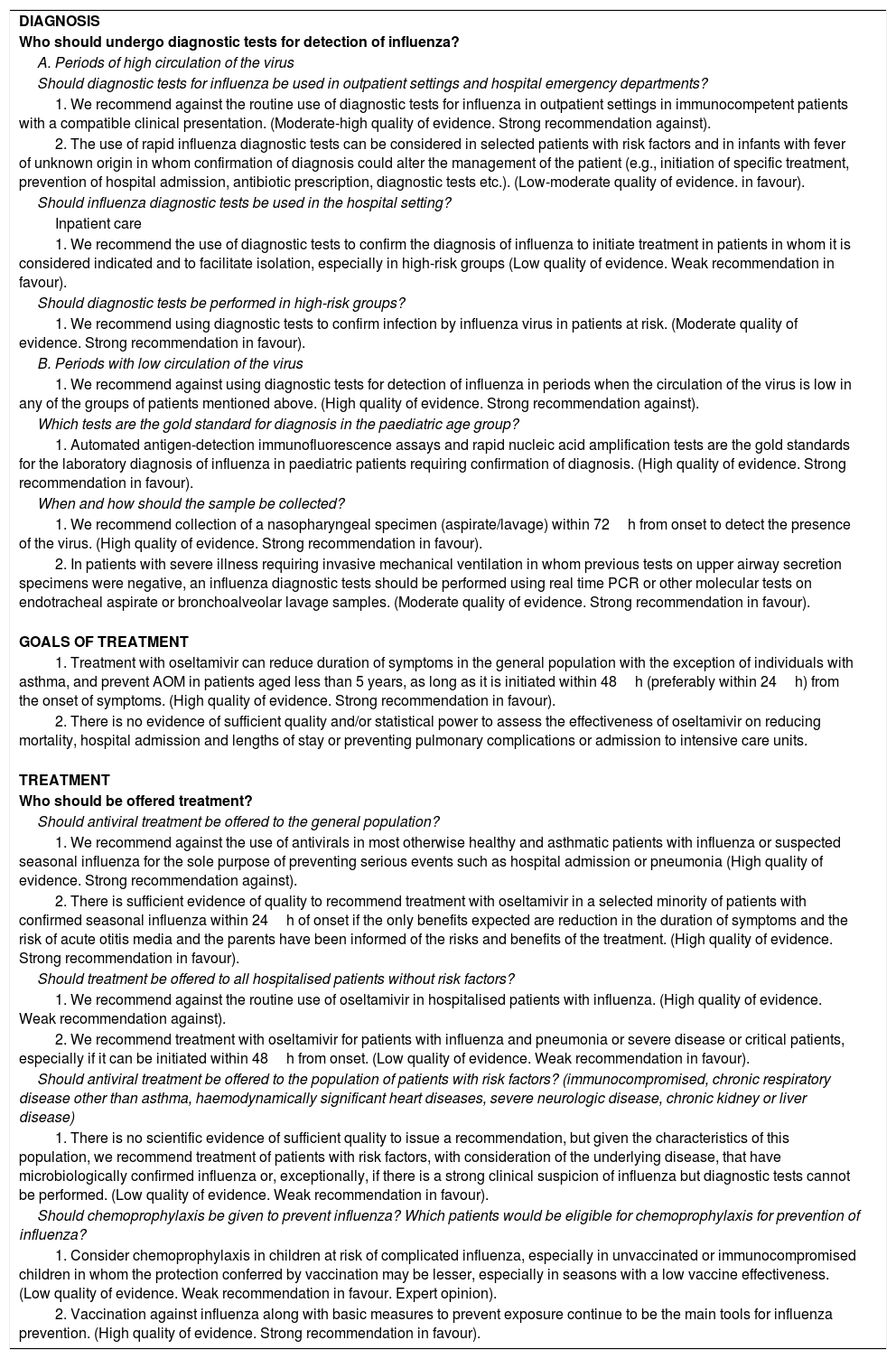
The panel drafted the final recommendations taking into account the quality of the evidence, the risk of bias, the risk–benefit ratio and economic considerations. In case evidence was unavailable or of inadequate quality, the recommendations were founded on expert opinion. All members of the WG eventually agreed on the recommendations. Table 1 presents a summary of the final recommendations.
Summary of the recommendations.
| DIAGNOSIS |
| Who should undergo diagnostic tests for detection of influenza? |
| A. Periods of high circulation of the virus |
| Should diagnostic tests for influenza be used in outpatient settings and hospital emergency departments? |
| 1. We recommend against the routine use of diagnostic tests for influenza in outpatient settings in immunocompetent patients with a compatible clinical presentation. (Moderate-high quality of evidence. Strong recommendation against). |
| 2. The use of rapid influenza diagnostic tests can be considered in selected patients with risk factors and in infants with fever of unknown origin in whom confirmation of diagnosis could alter the management of the patient (e.g., initiation of specific treatment, prevention of hospital admission, antibiotic prescription, diagnostic tests etc.). (Low-moderate quality of evidence. in favour). |
| Should influenza diagnostic tests be used in the hospital setting? |
| Inpatient care |
| 1. We recommend the use of diagnostic tests to confirm the diagnosis of influenza to initiate treatment in patients in whom it is considered indicated and to facilitate isolation, especially in high-risk groups (Low quality of evidence. Weak recommendation in favour). |
| Should diagnostic tests be performed in high-risk groups? |
| 1. We recommend using diagnostic tests to confirm infection by influenza virus in patients at risk. (Moderate quality of evidence. Strong recommendation in favour). |
| B. Periods with low circulation of the virus |
| 1. We recommend against using diagnostic tests for detection of influenza in periods when the circulation of the virus is low in any of the groups of patients mentioned above. (High quality of evidence. Strong recommendation against). |
| Which tests are the gold standard for diagnosis in the paediatric age group? |
| 1. Automated antigen-detection immunofluorescence assays and rapid nucleic acid amplification tests are the gold standards for the laboratory diagnosis of influenza in paediatric patients requiring confirmation of diagnosis. (High quality of evidence. Strong recommendation in favour). |
| When and how should the sample be collected? |
| 1. We recommend collection of a nasopharyngeal specimen (aspirate/lavage) within 72h from onset to detect the presence of the virus. (High quality of evidence. Strong recommendation in favour). |
| 2. In patients with severe illness requiring invasive mechanical ventilation in whom previous tests on upper airway secretion specimens were negative, an influenza diagnostic tests should be performed using real time PCR or other molecular tests on endotracheal aspirate or bronchoalveolar lavage samples. (Moderate quality of evidence. Strong recommendation in favour). |
| GOALS OF TREATMENT |
| 1. Treatment with oseltamivir can reduce duration of symptoms in the general population with the exception of individuals with asthma, and prevent AOM in patients aged less than 5 years, as long as it is initiated within 48h (preferably within 24h) from the onset of symptoms. (High quality of evidence. Strong recommendation in favour). |
| 2. There is no evidence of sufficient quality and/or statistical power to assess the effectiveness of oseltamivir on reducing mortality, hospital admission and lengths of stay or preventing pulmonary complications or admission to intensive care units. |
TREATMENT |
| Who should be offered treatment? |
| Should antiviral treatment be offered to the general population? |
| 1. We recommend against the use of antivirals in most otherwise healthy and asthmatic patients with influenza or suspected seasonal influenza for the sole purpose of preventing serious events such as hospital admission or pneumonia (High quality of evidence. Strong recommendation against). |
| 2. There is sufficient evidence of quality to recommend treatment with oseltamivir in a selected minority of patients with confirmed seasonal influenza within 24h of onset if the only benefits expected are reduction in the duration of symptoms and the risk of acute otitis media and the parents have been informed of the risks and benefits of the treatment. (High quality of evidence. Strong recommendation in favour). |
| Should treatment be offered to all hospitalised patients without risk factors? |
| 1. We recommend against the routine use of oseltamivir in hospitalised patients with influenza. (High quality of evidence. Weak recommendation against). |
| 2. We recommend treatment with oseltamivir for patients with influenza and pneumonia or severe disease or critical patients, especially if it can be initiated within 48h from onset. (Low quality of evidence. Weak recommendation in favour). |
| Should antiviral treatment be offered to the population of patients with risk factors? (immunocompromised, chronic respiratory disease other than asthma, haemodynamically significant heart diseases, severe neurologic disease, chronic kidney or liver disease) |
| 1. There is no scientific evidence of sufficient quality to issue a recommendation, but given the characteristics of this population, we recommend treatment of patients with risk factors, with consideration of the underlying disease, that have microbiologically confirmed influenza or, exceptionally, if there is a strong clinical suspicion of influenza but diagnostic tests cannot be performed. (Low quality of evidence. Weak recommendation in favour). |
| Should chemoprophylaxis be given to prevent influenza? Which patients would be eligible for chemoprophylaxis for prevention of influenza? |
| 1. Consider chemoprophylaxis in children at risk of complicated influenza, especially in unvaccinated or immunocompromised children in whom the protection conferred by vaccination may be lesser, especially in seasons with a low vaccine effectiveness. (Low quality of evidence. Weak recommendation in favour. Expert opinion). |
| 2. Vaccination against influenza along with basic measures to prevent exposure continue to be the main tools for influenza prevention. (High quality of evidence. Strong recommendation in favour). |
These recommendations do not yet incorporate the preferences of patients. Since influenza is an acute disease, there are no patient associations specific to it. For the time being, it is not clear how the preferences of patients and their families should weigh on these recommendations.
RecommendationsDiagnosisHow should influenza be diagnosed?The diagnosis of influenza is usually clinical, but it is challenging in the paediatric age group, especially in infants and young children. Studies with moderate to high quality of evidence have found very low sensitivity and positive predictive values of clinical diagnosis. Fever is the most frequent manifestation, present in 95% of cases, and the only predictor of influenza that is consistent across studies. In infants aged less than 6 months, influenza frequently presents with a picture suggestive of sepsis. Many of the review studies were unable to confirm the usefulness of the presence of cough or throat pain, features that are commonly included in definitions of “influenza-like illness”.6,7
Who should undergo diagnostic tests for detection of influenza?A. Periods with high circulation of the virusShould diagnostic tests for influenza be used in outpatient settings?
- 1.
We recommend against the routine use of diagnostic tests for influenza in outpatient settings in immunocompetent patients with a compatible clinical presentation. (Moderate-high quality of evidence. Strong recommendation against8,9).
- 2.
The use of rapid influenza diagnostic tests can be considered in selected patients with risk factors and in infants with fever of unknown origin in whom confirmation of diagnosis could alter the management of the patient (e.g., prevent hospital admission, antibiotic prescription, diagnostic tests). (Low-moderate quality of evidence. Weak recommendation in favour8,9).
Emergency department
- 1.
We recommend against the routine use of influenza diagnostic tests in hospital emergency departments in immunocompetent patients with a compatible clinical presentation who are going to be managed at the outpatient level. (Moderate to high quality of evidence. Strong recommendation against8,10).
- 2.
The use of influenza diagnostic tests can be considered in selected patients with risk factors and in infants with fever of unknown origin in whom confirmation of diagnosis could alter the management of the patient (e.g., initiation of specific treatment, prevention of antibiotic prescription or hospital admission, diagnostic tests, etc.). (Low to moderate quality of evidence. Weak recommendation in favour10).
Inpatient care
- 1.
We recommend the use of diagnostic tests to confirm the diagnosis of influenza to initiate treatment in patients in whom it is considered indicated and to facilitate isolation, especially in high-risk groups, and in the paediatric intensive care unit or units that manage immunocompromised patients. (Low quality of evidence. Weak recommendation in favour8,11,12).
Should diagnostic tests be performed in high-risk groups?
- 1.
We recommend using diagnostic tests to confirm infection by influenza virus in patients at risk. (Moderate quality of evidence. Strong recommendation in favour13).
- 1.
We recommend against using diagnostic tests for detection of influenza in periods when the circulation of the virus is low in any of the groups of patients mentioned above. (High quality of evidence. Strong recommendation against13).
Which tests are the gold standard for diagnosis in the paediatric age group?
- 1.
Although there is high-quality evidence that traditional rapid influenza diagnostic tests that detect viral antigens by immunoassay have an acceptable sensitivity and specificity, especially during the epidemic season, there is also high-quality evidence that newer automated antigen-detection immunofluorescence assays and rapid nucleic acid amplification or detection tests are much more sensitive, so we recommend the latter as the tests of choice for the laboratory detection of influenza in paediatric patients that require confirmation of diagnosis (High quality of evidence. Strong recommendation in favour14).
When and how should the sample be collected?
- 1.
We recommend collection of a nasopharyngeal specimen (aspirate/lavage) to detect the virus on account of the higher sensitivity of testing in these samples as opposed to isolated nasal or oropharyngeal specimens. (High quality of evidence. Strong recommendation in favour15).
- 2.
The sample should be collected as soon as possible, as the maximum yield of testing is achieved when specimens are obtained within 72h from onset, although in infants, young children and immunocompromised patients, the duration of viral dissemination may be of more than 1 week. (High quality of evidence. Strong recommendation in favour15,16).
- 3.
An acceptable alternative to a nasopharyngeal specimen (aspirate or lavage) is the collection of both a nasal and oropharyngeal specimen in a single container, as this causes less discomfort to the patient and offers an acceptable sensitivity for detection of the virus with molecular tests (Moderate to low quality of evidence. Weak recommendation in favour15,16).
- 4.
In patients with severe illness requiring invasive mechanical ventilation in whom previous tests on upper airway secretion specimens were negative, an influenza diagnostic tests should be performed using real time PCR or other molecular tests on endotracheal aspirate or bronchoalveolar lavage samples. (Moderate quality of evidence. Strong recommendation in favour15,16).
Reducing duration of symptoms
- 1.
There are no quality hospital-based studies allowing evaluation of this aspect.
- 2.
At the outpatient level, there are studies of moderate to high quality that show that treatment with oseltamivir in the first 48h from onset and preferably within 24h reduces the duration of symptoms by 1–2 days, so treating outpatients could be recommended for the purpose of reducing the duration of symptoms. (High quality of evidence. Strong recommendation in favour17).
- 3.
There is high quality evidence that asthmatic patients do not benefit from outpatient treatment with oseltamivir, so these patients should not receive this treatment with the aim of reducing duration of symptoms. (High quality of evidence. Strong recommendation against18).
Reducing mortality
- 1.
Although there is evidence of moderate-to-high quality that antiviral treatment does not reduce mortality in hospitalised patients, the low frequency of death in paediatric patients makes it difficult to establish a recommendation. The current data, however, allow for a weak recommendation in favour of early initiation of antiviral treatment in hospitalised patients with influenza associated with pneumonia and/or respiratory failure or patients admitted to the intensive care unit. (Moderate quality of evidence. Weak recommendation in favour19,20).
Reducing admissions to paediatric intensive care units
- 1.
The quality of the evidence available to assess this item is low. However, since requiring intensive care or mechanical ventilation are considered key outcome measures, the use at an early stage of oseltamivir to reduce the need for either may be justified in certain high-risk populations. (Low quality of evidence. Weak recommendation in favour19,21).
Reducing rate of hospitalization
- 1.
Due to the low quality of the available evidence, we give a weak recommendation against the routine use of oseltamivir in paediatric patients with influenza with the aim of reducing the number of hospital admissions. (Low quality of evidence. Weak recommendation against18).
Reducing length of hospital stay
- 1.
There are no quality studies allowing the evaluation of this outcome. The scarce data currently available justify a weak recommendation against the use of oseltamivir in hospitalised patients for the purpose of reducing length of stay. (Low quality of evidence. Weak recommendation against22).
Reducing or preventing pulmonary complications
- 1.
The data are insufficient to evaluate this outcome. The current evidence is contradictory and of low quality, so we are unable to make a recommendation.
Reducing or preventing extrapulmonary complications
- 1.
There is evidence of moderate to high quality that treatment with oseltamivir in patients with microbiologically confirmed influenza prevents acute otitis media, especially in those aged less than 5 years, if treatment is initiated within 12–24h from the onset of symptoms. (High quality of evidence. Strong recommendation in favour23,24).
- 2.
There is no evidence of sufficient quality to make a general recommendation for treatment with oseltamivir for prevention of acute otitis media in all other patients. (Low quality of evidence. Weak recommendation against20,21).
- 3.
There are no data to assess the use of oseltamivir in the prevention or treatment of other extrapulmonary complications (myositis, myocarditis, neurologic complications, etc.).
Should antiviral treatment be offered to the general population?
- 1.
We recommend against the use of antivirals in most otherwise healthy and asthmatic patients with known or suspected influenza for the sole purpose of preventing serious events such as hospital admission or pneumonia. (High quality of evidence. Strong recommendation against18,23,24).
- 2.
There is sufficient evidence of quality to recommend treatment with oseltamivir in a selected minority of patients with confirmed influenza within 24h of onset if the only benefits expected are reduction in the duration of symptoms and the risk of acute otitis media and the parents have been informed of the risks and benefits of the treatment. (High quality of evidence. Strong recommendation in favour18,23,24).
Should treatment be offered to all hospitalised patients without risk factors?
- 1.
We recommend against the use of antivirals in most hospitalised patients for prevention of most relevant outcomes (death, complications, prolonged length of stay). This recommendation derives from high-quality studies which, qualified by the low number of patients that have serious outcomes, leads us to grade the recommendation as weak. (High quality of evidence. Weak recommendation against18,23,24).
- 2.
We recommend treatment with oseltamivir for patients with influenza and pneumonia or severe disease or critical patients, especially if it can be initiated within 48h from onset. (Low quality of evidence. Weak recommendation in favour15–17,20,21).
Should antiviral treatment be offered to the population of patients that have risk factors? (immunocompromised, chronic respiratory disease other than asthma, haemodynamically significant heart diseases, severe neurologic disease, chronic kidney or liver disease)
- 1.
There is no scientific evidence of sufficient quality to issue a recommendation, but given the characteristics of this population, we recommend treatment of patients with risk factors, with consideration of the underlying disease, that have microbiologically confirmed influenza or, only exceptionally, if there is a strong clinical suspicion of influenza but diagnostic tests cannot be performed. (Low quality of evidence. Weak recommendation in favour23,24).
- 2.
It is important to provide health education to these patients due to their increased vulnerability, so they will seek care early upon development of flu-like symptoms and, should infection by influenza be confirmed and treatment indicated, be able to start treatment within 48h from onset. (Expert opinion).
Should chemoprophylaxis be given to prevent influenza? Which patients would be eligible for chemoprophylaxis for prevention of influenza?
- 1.
Vaccination against influenza along with basic measures to prevent exposure continue to be the best tools for the prevention of influenza. (High quality of evidence. Strong recommendation in favour). Raising awareness about vaccination among health care professionals and in the community should be made a priority.2,25
- 2.
Although the quality of the evidence is low, chemoprophylaxis should be considered in children with risk factors for complicated influenza, especially in those who are not vaccinated or who are immunocompromised (in whom the protection conferred by vaccination may be lesser), especially in seasons with a low vaccine effectiveness (Low quality of evidence. Weak recommendation in favour. Expert opinion2,25).
This document offers recommendations for the treatment of influenza with oseltamivir. These recommendations are based on the evidence of highest quality available and have been developed using the GRADE method to adapt them to real-world clinical conditions. In some cases, the evidence was sufficient to propose clear recommendations. In other cases, the data were inadequate and only allowed weak recommendations. Further research in the paediatric population is required to clearly establish the benefits of antiviral drugs against influenza.
FundingWe received no funding towards the development of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Members of the Working Group on Respiratory Infections of the SEIP that participated in the review of the manuscript:
Cristina Calvo. Department of Paediatrics and Infectious Diseases, Hospital Universitario La Paz, Madrid. Fundación IdiPaz, Madrid. Network for Translational Research on Paediatric Infectious Disease (RITIP). European Network of Excellence for Paediatric Clinical Research (TEDDY Network), Italy.
Carlos Rodrigo-Gonzalo de Liria. Research Group on Paediatric Infectious Disease, Hospital Sant Joan de Déu, Universitat de Barcelona. Biomedical Research Centre Network of Epidemiology and Public Health (CIBERESP), Instituto Nacional de Salud Carlos III, Madrid.
Please cite this article as: Tagarro A, Cruz-Cañete M, Otheo E, Launes C, Couceiro JA, Pérez C, et al. Oseltamivir para el tratamiento de la gripe en niños y adolescentes. An Pediatr (Barc). 2019. https://doi.org/10.1016/j.anpedi.2019.01.009