This study assesses the clinical characteristics and epidemiology of children with eye trauma presenting to the Emergency Department in Spain and analyze the risk factors associated with immediate sequelae.
MethodsA multicentric prospective case series study conducted during 24 months of patients presenting to the Pediatric Emergency Departments in five hospitals collaborating with the Spanish Pediatric Emergency Research Group. Data were collected from October 2016 through September 2018, including all patients up to the age of 16 years old presenting to the Emergency Department with an ocular trauma. All injuries were classified by Birmingham Eye Trauma Terminology (BETT).
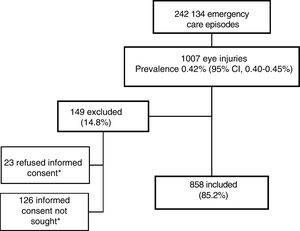
ResultsA total of 242 134 visits to the Emergency Departments took place during the study period, being 1007 ocular traumas (0,42%; IC 95% 0,40−0,45) and 858 were included in the study. Most commonly, injuries occurred while playing (54,7%), except in the 15 or more-age group, in which sports activities were more common (23,1%). The place of the trauma varied depending on the age group, being home (34,7%) and schools or sports areas (34,3%) the most recurrent. Blunt objects were the most frequent mechanism of trauma (48,6%). Most of the injuries were classified as closed globe (85,5%), mainly contusions (52,7%). Fifty-eight patients (6,8%) presented with immediate sequelae, being the impairment of visual acuity the most common (70,7%). The risk factors associated with immediate sequelae were the 10 or more-age group, the preexisting refractive errors, the open globe injuries and the injuries with blunt objects.
ConclusionsOcular trauma is a frequent chief complaint in the Pediatric Emergency Departments in Spain. Increasing awareness of the serious nature of ocular injuries and the study of the risk factors will help to develop a comprehensive plan for educating both parents and children to minimize preventable eye injuries sequelae.
Describir las características clínico-epidemiológicas de los traumatismos oculares atendidos en los servicios de urgencias pediátricas (SUP) españoles y estudiar los factores de riesgo asociados a secuelas inmediatas.
MétodosSerie de casos multicéntrica con recogida de datos prospectiva desarrollada durante 24 meses, desde octubre de 2016, en los servicios de urgencias pediátricos (SUP) de 5 hospitales pertenecientes a la Red de Investigación de la Sociedad Española de Urgencias Pediátricas. Se incluyeron todos los niños de 0 a 16 años que consultaron en Urgencias por traumatismo ocular. Las lesiones fueron clasificadas según la clasificación Birmingham Eye Trauma Terminology (BETT).
ResultadosSe registraron 242.134 episodios, de los que 1.007 correspondieron a traumatismos oculares (0,42%; IC 95% 0,40-0,45), incluyéndose 858 en el estudio.
La mayoría de las lesiones ocurrieron durante el juego infantil (54,8%), salvo en los mayores de 15 años que ocurrió en las actividades deportivas (23,1%). Tuvieron lugar preferentemente en domicilio (34,7%) y centros educativos o deportivos (34,3%). Los objetos contusos fueron el mecanismo más frecuente (48,6%).
La mayoría de las lesiones fueron de globo cerrado (85,5%), sobre todo contusiones (52,7%). El 6,8% de los pacientes presentaron secuelas inmediatas, siendo la disminución de la agudeza visual la más frecuente (70,7%). La edad mayor de 10 años, padecer defectos de la refracción previos, estar causadas por objetos contusos y las lesiones de globo abierto se asociaron a mayor riesgo de secuelas.
ConclusionesLos traumatismos oculares son una entidad relevante en los servicios de urgencias pediátricos por las secuelas visuales que ocasiona. Las causas y los lugares donde se producen varían en función de la edad. El conocimiento de los factores de riesgo es fundamental para implementar medidas preventivas y evitar secuelas visuales inmediatas.
It is estimated that up to 6 million children worldwide experience some form of ocular trauma each year, of who up to 5% require hospital admission.1 Furthermore, the long-term morbidity of ocular trauma is significant, and it is the leading cause of acquired unilateral blindness in the paediatric age group.2
The sequelae of eye injuries in children are more severe compared to adults, since ocular maturity is not achieved until age 9–10 years, thereby increasing the risk of amblyopia and the years of impaired vision.3 Between 8% and 14% of these children develop severe visual impairment or blindness, which has an impact on their personal, social and occupational development.4
Fortunately, it is estimated that paediatric ocular trauma can be prevented in up to 90% of cases.5 In order to implement preventive measures, we first need to know the circumstances surrounding these injuries.
Although the epidemiological characteristics of ocular trauma have been described in the literature in both developed and developing countries,2 to date only one retrospective, single-centre study published by Burgueño et al. in 1998 has been conducted in Spain describing the epidemiology, injury mechanisms and preventive aspects of eye injuries in children aged less than 14 years managed in the emergency department.6
Since that study had a local scope, its results may not be representative of all of Spain, which motivated the study presented here, the objectives of which were to describe the prevalence and epidemiological characteristics of traumatic eye injuries managed in paediatric emergency departments (PEDs) in Spain, and to analyse potential risk factors for immediate sequelae.
Material and methodsDesignWe conducted a prospective multicentre study with case-control subgroup analysis over 24 months in 5 PEDs of secondary and tertiary hospitals members of the research network of the Sociedad Española de Urgencias Pediátricas (Spanish Society of Paediatric Emergency Medicine) (RiSEUP-SPERG): 2 hospitals in the Community of Madrid, 1 in the Basque Country, 1 in Andalusia and 1 in the Valencian Community (Appendix A).
All participating hospitals recruited patients over a period of 2 years, with data collection starting in October 2016.
We recruited every child aged 0–16 years that sought care for ocular trauma in any of the participating PEDs. We excluded patients for who we did not obtain informed consent, either because it was not sought or because it was not given.
We developed a data collection form to be filled out by the provider that managed the patient after obtaining informed consent. If the patient required care from an ophthalmologist or another specialist, we collected data from the health records once the episode of care had finished. We designated a research collaborator in each participating hospital. These individuals were responsible for submitting the data through a Google Drive questionnaire. The resulting database could only be accessed by the principal investigators.
Patients were managed in adherence with hospital protocols and the judgment of the attending physician, ensuring that participation in the study did not interfere with customary clinical practice.
The study was approved by the clinical research ethics committee of each participating hospital. The handling of the data adhered to Organic Law 15/1999 of 13 December on the protection of personal data. To safeguard the confidentiality of the patient, each individual was assigned an alphanumeric code before entering the data in the database to prevent identification. For children aged less than 12 years, we obtained consent by the parents or legal guardians, and for older children, we obtained consent from the parents or guardians as well as the assent of the child.
Study variablesWe collected data on epidemiological variables (age, sex and pre-existing refractive errors), data on the circumstances of the traumatic injury (day of the week and time, setting, presence of an adult, site of injury, mechanism of injury and causative agent), and data on its management (time elapsed from the traumatic event to receiving care, setting of initial care, primary diagnosis, referral to ophthalmology, surgical intervention such as repair of the globe or ocular adnexa, hospital admission and presence of immediate sequelae).
We made the final diagnosis based on the data documented in the health records applying the Birmingham Eye Trauma Terminology (BETT).7–9
We defined immediate sequelae as any new acute complaint or worsening of the initial complaint following and resulting from ocular trauma identified in the emergency department. The term encompasses a broad spectrum of permanent problems, such as mild to full vision loss in one or both eyes, temporary or persistent diplopia, minor to severe cosmetic abnormalities of the eyes and face, and ocular or periocular pain.10 We defined vision loss as a decrease in visual acuity identified by an ophthalmologist.
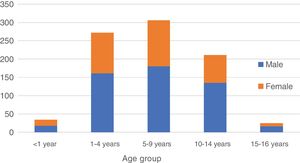
We divided patients in different age groups based on the previous literature on the subject of unintentional injuries in the paediatric population (> 1 years, 1−4 years, 5−9 years, 10−14 years and > 15 years). We divided the days of the week into weekdays (Monday-Friday) and weekend/holidays (Saturdays, Sundays and holidays). We divided the hours of the day into morning (8:00 to 15:00), afternoon (15:00 to 22:00) and night (22:00 to 08:00).
Sample size and statistical analysisWe estimated that we needed a sample of 707 traumatic eye injuries to describe their sequelae, assuming a frequency of 8% based on studies in our region,6 for a precision of 2% and a 95% level of confidence. Since based on unpublished data reported at the XIX Annual Meeting of the SEUP (Trauma Ocular Pediátrico) the proportion of the total emergency care episodes that correspond to ocular trauma is 0.3%, we calculated that we needed a sample size of at least 220 000 emergencies. After reaching the required sample size, we continued gathering data until a full year was completed to eliminate the risk of seasonal bias in the collection of epidemiological data.
We have expressed qualitative data as absolute frequencies and percentages and quantitative data, which had an asymmetrical distribution, as median an interquartile range (IQR). We assessed the association between qualitative variables by means of the chi square test. We performed a case-control subgroup analysis comparing patients that developed immediate ophthalmological sequelae vs those that did not. We fitted univariate and multivariate logistic regression models to assess the association of potential risk factors, measuring the strength of the association by means of odds ratios (ORs) with the corresponding 95% confidence intervals (95% CIs).
The statistical analysis was performed with the Statistical Package for Social Science (SPSS 22.0) and the Software for Statistics and Data Science (STATA 12.0). We defined statistical significance as a p-value of less than 0.05 (2-tailed tests).
ResultsIn the period under study, participating PEDs received a total of 242 134 visits, of which 1007 corresponded to episodes of ocular trauma (0.42%; 95% CI, 0.40−0.45%), and 858 were included in the study (Fig. 1).
Epidemiological characteristicsPatients with ocular trauma were predominantly male (60.1%) and had a median age of 6.5 years (IQR, 3.5–10.5). We found an increasing proportion of male patients with increasing age (age < 1 year: 52.9%; 1−4 years: 59.2%; 5−9 years: 58.8%; 10−14 years: 64.0%; 15–16 years: 68.0%), although the trend was not statistically significant (P = .134) (Fig. 2).
Table 1 presents the characteristics of patients with ocular trauma.
Epidemiological characteristics of traumatic eye injuries.
| N | n | % | 95% CI |
|---|---|---|---|
| Sex | |||
| Male | 511 | 60.1% | (56.7−63.4%) |
| Female | 339 | 39.9% | (36.6−43.3%) |
| Unknown | 8 | 0.9% | |
| Age group | |||
| < 1 year | 34 | 4.0% | (2.8−5.5%) |
| 1−4 years | 274 | 32.0% | (28.9−35.3%) |
| 5−9 years | 309 | 36.1% | (32.9−39.4%) |
| 10−14 years | 213 | 24.9% | (22.0−27.9%) |
| ≥ 15 years | 26 | 3.0% | (2.0−4.4%) |
| Unknown | 2 | 0.2% | |
| Day of the week | |||
| Monday-Friday | 653 | 76.3% | (73.3−79.1%) |
| Saturday | 84 | 9.8% | (7.9−12.0%) |
| Sunday or holiday | 119 | 13.9% | (11.7−16.4%) |
| Unknown | 2 | 0.2% | (0−0.8%) |
| Time of day | |||
| Morning | 356 | 41.6% | (38.3−45.0%) |
| Afternoon | 393 | 46.0% | (42.5−49.3%) |
| Night | 106 | 12.4% | (10.3−14.8%) |
| Unknown | 3 | 0.3% | (0.1−1.0%) |
| Time to seeking care | |||
| < 1 h | 159 | 18.7% | (16.1−21.4%) |
| 1−24 hours | 578 | 67.8% | (64.6−71.0%) |
| >24 h | 115 | 13.5% | (11.3−16.0%) |
| Unknown | 6 | 0.7% | (0.3−1.5%) |
| Setting | |||
| Home | 291 | 34.9% | (31.6−38.2%) |
| School/sports grounds | 286 | 34.3% | (31.0−37.6%) |
| Streets | 99 | 11.9% | (9.7−14.2%) |
| Park/countryside | 104 | 12.5% | (10.3−14.9%) |
| Other outdoor | 21 | 2.5% | (1.6−3.8%) |
| Other indoor | 34 | 4.1% | (2.8−5.6%) |
| Unknown | 23 | 2.7% | (1.7−4.0%) |
| Witnessed by an adult | |||
| No | 273 | 31.8% | (28.7−34.9%) |
| Yes | 556 | 64.8% | (61.6−68.0%) |
| Unknown | 29 | 3.4% | (2.2−4.6%) |
| Location | |||
| Right | 424 | 49.4% | (46.0−52.8%) |
| Left | 412 | 48.5% | (45.1−51.9%) |
| Bilateral | 22 | 2.6% | (1.6−3.9%) |
| Cause | |||
| Sports | 82 | 9.6% | (7.7−11.8%) |
| Physical fight | 17 | 2.0% | (1.2−3.2%) |
| Play | 469 | 54.8% | (51.4−58.2%) |
| Household accident | 49 | 5.7% | (4.3−7.5%) |
| Outdoors | 69 | 8.1% | (6.3−10.1%) |
| Person | 25 | 2.9% | (1.9−4.3%) |
| Other unintentional | 96 | 11.2% | (9.2−13.5%) |
| Unknown | 51 | 6.0% | (4.5−7.8%) |
| Causative agent | |||
| Blunt | 417 | 48.7% | (45.3−52.1%) |
| Sharp | 258 | 30.1% | (27.1−33.3%) |
| Burn | 50 | 5.8% | (4.4−7.6%) |
| Other | 133 | 15.5% | (13.2−18.1%) |
| Previous care | |||
| None | 539 | 62.8% | (59.5−66.1%) |
| Health professional | 300 | 35.0% | (31.8−38.3%) |
| School staff | 19 | 2.2% | (1.3−3.4%) |
| Pre-existing refractive error | |||
| No | 822 | 96.0% | (94.5−97.2%) |
| Yes | 36 | 4.2% | (3.0−5.8%) |
Values expressed as absolute frequency (n) and percentage (%) with the corresponding 95% confidence interval (CI).
In children aged less than 5 years, the most frequent setting where the injury took place was the home, compared to schools or sports/recreation facilities in children aged 5–14 years or the street in patients aged more than 15 years (Table 2).
Distribution of settings of injury by age group.
| [0,1–9]Setting | ||||||||
|---|---|---|---|---|---|---|---|---|
| Home | School/Sports grounds | Street | Park | Other outdoors | Other indoors | Unknown | Total | |
| < 1 year% (95% CI) | 2058.8% (40.7−75.4%) | 38.8% (1.9−23.7%) | 411.8% (3.3−27.5%) | 12.9% (0.1−15.3%) | 0 | 38.8% (1.9−23.7%) | 38.8% (1.9−23.7%) | 34 |
| 1−4 years% (95% CI) | 13850.4% (44.5−56.4%) | 6021.9% (17.1−27.3%) | 269.5% (6.3−13.6%) | 2910.6% (7.2−14.8%) | 41.5% (0.4−3.7%) | 114.0% (2.0−7.1%) | 62.2% (0.8−4.7%) | 274 |
| 5−9 years% (95% CI) | 8828.5% (23.5−33.9%) | 11336.6% (31.2−42.2%) | 299.4% (6.4−13.2%) | 4514.6% (10.8−19.0%) | 92.9% (1.3−5.5%) | 165.2% (3.0−8.3%) | 92.9% (1.3−5.5%) | 309 |
| 10−14 years% (95% CI) | 3717.4% (12.5−23.1%) | 10448.8% (41.9−55.7%) | 3014.1% (9.7−19.5%) | 2813.1% (8.9−18.4%) | 83.8% (1.6−7.3%) | 20.9% (0.1−3.4%) | 41.9% (0.5−4.7%) | 213 |
| >15 years% (95% CI) | 623.1% (9.0−43.6%) | 623.1% (9.0−43.6%) | 1038.5% (20.2−59.4%) | 13.8% (0.1−19.6%) | 0 | 27.7% (0.9−25.1%) | 13.8% (0.1−19.6%) | 26 |
| Total% (95% CI) | 28934.7% (31.5−38.0%) | 28634.3% (31.1−37.7%) | 9911.9% (9.8−14.3%) | 10412.5% (10.3−14.9%) | 212.5% (1.6−3.8%) | 344.1% (2.8−5.7%) | 232.7% (1.7−4.0%) | 856* |
Values expressed as absolute frequency (n) and percentage (%) over the total patients in the age group with the corresponding 95% confidence interval (CI).
Injuries occurred most frequently in the context of play (54.8%), which was the most frequent cause of ocular trauma in nearly every age group, especially through age 9 years. Ocular trauma secondary to household accidents (defined as an injury occurring at home unrelated to play) was most frequent in patients aged 1–4 years (61.2%) (Table 3).
Distribution of the cause of injury by age group.
| [0,1–10]Cause | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Sports | Physical fight | Play | Household accident | Outdoors | Person | Other accidents | Unknown | Total | |
| <1 year% (95% CI) | 12.9% (0.1−15.3%) | 0 | 1955.9% (37.9−72.8%) | 25.9% (0.7−19.7%) | 12.9% (0.1−15.3%) | 25.9% (0.7−19.7%) | 411.8% (3.3−27.5%) | 514.7% (5.0−31.1%) | 34 |
| 1−4 years% (95% CI) | 31.1% (0.2−3.2%) | 31.1% (0.2−3.2%) | 16560.2% (54.2−66.1%) | 3010.9% (7.5−15.3%) | 145.1% (2.8−8.4%) | 103.6% (1.8−6.6%) | 3512.8% (9.1−17.3%) | 145.1% (2.8−8.4%) | 274 |
| 5−9 years% (95% CI) | 185.8% (3.5−9.1%) | 20.6% (0.1−2.3%) | 19061.5% (55.8−66.9%) | 103.2% (1.6−5.9%) | 3511.3% (8.0−15.4%) | 82.6% (1.1−5.0%) | 3511.3% (8.0−15.4%) | 113.6% (1.8−6.3%) | 309 |
| 10−14 years% (95% CI) | 5425.4% (19.7−31.7%) | 94.2% (1.9−7.9%) | 9142.7% (36.0−49.7%) | 31.4% (0.3−4.1%) | 178.0% (4.7−12.5%) | 52.3% (0.8−5.4%) | 178.0% (4.7−12.5%) | 178.0% (4.7−12.5%) | 213 |
| >15 years% (95% CI) | 623.1% (9.0−43.6%) | 311.5% (2.4−30.2%) | 415.4% (4.4−34.9%) | 415.4% (4.4−34.9%) | 27.7% (0.9−25.1%) | 0 | 311.5% (2.4−30.2%) | 415.4% (4.4−34.9%) | 26 |
| Total% (95% CI) | 829.6% (7.7−11.8%) | 172.0% (1.2−3.2%) | 46954.8% (51.4−58.2%) | 495.7% (4.3−7.5%) | 698.1% (6.3−10.1%) | 252.9% (1.9−4.3%) | 9411.0% (9.0−13.3%) | 516.0% (4.5−7.8%) | 856* |
Values expressed as absolute frequency (n) and percentage (%) over the total patients in the age group with the corresponding 95% confidence interval (CI).
Blunt objects (toys, projectiles, furniture…) were the most frequent causative agent in every age group. Sharp objects caused injury mainly in children aged 1–9 years, while acid or alkaline substances and thermal devices that could cause burns caused the most injuries between 1 and 4 years of age (Table 4).
Distribution of mechanism of injury by age group.
| Mechanism | |||||
|---|---|---|---|---|---|
| Blunt object | Sharp object | Burn | Other | Total | |
| <1 year% (95% CI) | 1544.1% (27.2−62.1%) | 1235.3% (19.7−53.5%) | 12.9% (0.1−15.3%) | 617.6% (6.8−34.5%) | 34 |
| 1−4 years% (95% CI) | 11943.4% (37.5−49.5%) | 8029.2% (23.9−35.0%) | 2910.6% (7.2−14.8%) | 4616.8% (12.6−21.8%) | 274 |
| 5−9 years% (95% CI) | 14747.6% (41.9−53.3%) | 11336.6% (31.2−42.2%) | 113.6% (1.8−6.3%) | 3812.3% (8.9−16.5%) | 309 |
| 10−14 years% (95% CI) | 122*57.3% (50.3−64.0%) | 4923.0% (17.5−29.2%) | 73.3% (1.3−6.7%) | 3516.4% (11.7−22.1%) | 213 |
| >15 years% (95% CI) | 1350.0% (29.9−70.1%) | 415.4% (4.4−34.9%) | 27.7% (0.9−25.1%) | 726.9% (11.6−47.8%) | 26 |
| Total% (95% CI) | 41648.6% (45.2−52.0%) | 25830.1% (27.1−33.3%) | 505.8% (4.4−7.6%) | 13215.4% (13.1−18.0%) | 856* |
Values expressed as absolute frequency (n) and percentage (%) over the total patients in the age group with the corresponding 95% confidence interval (CI).
Up to 32.9% (n = 273) of eye injuries in children were not witnessed by an adult, and this percentage was higher in patients aged more than 10 years (n = 114; 49.4%) compared to younger patients (n = 158; 26.5%) (P < .001). We were unable to determine the age of 1 of the patients with an unwitnessed injury.
Diagnosis and management of ocular traumaWe classified cases of ocular trauma according to the Birmingham Eye Trauma Terminology (BETT)9 (Table 5), and found no statistically significant differences in the distribution of diagnoses by age group (P = .300).
Classification of ocular trauma using the Birmingham Eye Trauma Terminology (BETT)7–9 and diagnosis.
| Category | n% (CI) | BETTclassification | n% (CI) | Diagnosis | n% (CI) |
|---|---|---|---|---|---|
| Closed-globe | 73485.5% (83.0−87.8) | Contusion | 45252.7% (49.3−56.1) | Simple contusion | 20924.4% (21.5−27.4) |
| Hyphema | 101.2% (0.6−2.1) | ||||
| Vitreous haemorrhage | 30.3% (0.1−1.0) | ||||
| Commotio retinae | 70.8% (0.3−1.7) | ||||
| Superficial foreign body | 607.0% (5.4−8.9) | ||||
| Subconjunctival haemorrhage | 303.5% (2.4−5.0) | ||||
| Other | 13315.5% (13.2−18.1) | ||||
| Laceration | 316 | Conjunctival laceration | 667.7% (6.0−9.7) | ||
| Corneal laceration | 25029.1% (26.1−32.3) | ||||
| Open-globe | 182.1% (1.2−3.3) | Rupture | 0 | ||
| Penetrating injury | 141.6% (0.9−2.7) | ||||
| Perforating injury | 10.1% (0−0.6) | ||||
| Intraocular foreign body | 30.3% (0.1−1) | ||||
| Adnexa | 16719.5% (16.9−22.3) | ||||
| Periorbital | 20.2% (0−0.8) | Orbital bone fracture | 20.2% (0−0.8) | ||
| Periocular | 16619.3% (16.8−22.2) | Ecchymosis | 758.7% (6.9−10.8) | ||
| Eyelid laceration | 617.1% (5.5−9.0) | ||||
| Eyelid abrasion | 283.3% (2.2−4.7) |
Values given as absolute frequency (n) and percentage (%) with the 95% confidence interval (95% CI). Since the same traumatic event may affect different sites, more than one category may apply to a single episode.
An ophthalmologist was consulted in 559 cases (65.2%) and 24 patients required surgery (2.8%). Ten patients (1.2%) were admitted to hospital, none to the intensive care unit.
Immediate sequelaeFifty-eight patients (6.8%; 95% CI, 5.1-8.4%) had immediate sequelae: acute vision loss (n = 41; 70.7%), diplopia (n = 4; 6.9%), cosmetic abnormalities of the eyes (n = 10; 17.2%), cosmetic abnormalities of the face (n = 2; 3.5%) and pain with eye movements (n = 1; 1.7%).
We did not find an association between the presence of immediate sequelae and sex (7.7% in female patients vs 5.9% in male patients; P = .313), the time elapsed from the traumatic event to medical care (< 1 h, 5.9%; 1−24 hours, 6.9%; >24 h, 7.8%; P = .819), the time of the event (morning, 7.1%; afternoon, 7.1%; night 2.9%; P = .257) or the day of the week (weekdays, 7.2%; weekend/holidays, 5.5%; P = .387).
Table 6 presents the factors associated with the presence of immediate sequelae.
Potential risk factors for immediate sequelae of ocular trauma. Univariate and multivariate analyses.
| With sequelae | Univariate | Multivariate | ||||||
|---|---|---|---|---|---|---|---|---|
| n | % | OR | 95% CI | P | OR | 95% CI | P | |
| Age≥ 10 years< 10 years | 3622 | 15.33.6 | 4.8** | 2.8−8.4** | <.001** | 3.0** | 1.6-5.8** | .001** |
| SettingHomeSchool or sports groundsStreetParkOther outdoorsOther indoors | 112851121 | 3.89.85.210.69.52.9 | **2.71.43.02.70.8 | **1.3-5.60.5-4.01.3-7.10.5-12.80.1-6.1 | **.006.570.014.226.799 | **1.30.82.61.40.9 | **0.5-2.90.3-2.61.0-6.60.2-7.70.1-7.4 | **.580.747.046.726.918 |
| Pre-existing refractive errorYesNo | 1345 | 36.15.5 | 9.7** | 4.6−20.4** | <.001** | 3.9** | 1.6−9.4** | .003** |
| Witnessed*NoYes | 2827 | 10.34.9 | 2.2** | 1.3−3.9** | .003** | 1.8** | 1.0−3.4** | .052** |
| CauseSportsOther | 1840 | 22.05.2 | 5.1** | 2.8−9.5** | <.001** | 1.9** | 0.8−4.2** | .132** |
| MechanismBlunt objectOther | 4216 | 10.23.6 | 3.0** | 1.7−5.4** | <.001** | 2.1** | 1.1−3.9** | .030** |
| Bett classificationOpen-globeOther | 454 | 22.26.5 | 4.1** | 1.3−13.0** | .029** | 5.6** | 1.6−19.3** | .006** |
Sequelae described by means of the absolute frequency (n) and percentage (%).
BETT, Birmingham Eye Trauma Terminology; CI, confidence interval; OR, odds ratio.
The factors independently associated with the presence of sequelae in the multivariate analysis are presented in boldface.
The type of immediate sequelae produced by blunt objects (n = 42; 10.2%) were: vision loss (n = 29; 69.0%), cosmetic abnormalities in the eyes (n = 8; 19.0%), diplopia (n = 4; 9.5%) and pain with eye movement (n = 1; 2.4%). The only sequela found in patients with open-globe injuries (n = 4; 22.2%) was vision loss.
DiscussionThis is the first multicentre study of national scope describing the prevalence and characteristics of traumatic eye injuries managed in the paediatric emergency setting in Spain. In addition, none of the studies to date had analysed potential risk factors associated with the development of immediate sequelae. Given that ocular trauma is a leading cause of noncongenital blindness, identifying these risk factors is essential for the purpose of developing specific preventive measures.
In the United States, the annual incidence of ocular trauma is of approximately 2.4 million cases.11 A large paediatric cohort study conducted in the United States reported an average of 70 310 injuries per year,12 although it did not determine the proportion of paediatric emergency visits that they accounted for. We found that in Spain, they account for 0.42% of emergency visits, a slightly higher percentage compared to other unintentional injuries such as poisonings, which account for 0.29% of emergency visits according to the working group of the Sociedad Española de Urgencias de Pediatría.13
Most of the studies in the literature have found a predominance of male patients,14,15 with a 1.5:1 male: female ratio, which is probably related to the tendency of boys to engage in riskier activities.15,16
The setting of the traumatic event varied between age groups, with the home being the most common in children aged less than 5 years, the school or sports/recreational facilities most common in children aged 5–14 years and the street in adolescents aged more than 15 years. These findings, which were consistent with the previous literature,17–21 reflect that preschool-aged children spend more time at home and therefore are more likely to get injured there. In addition, most eye injuries caused by household accidents occurred in children aged 1–4 years, the group in which injuries associated with exposure to chemicals, most commonly found in homes, were most frequent.18,22 Some regulations are already in place for the control of these products and to prevent potential exposure of children, for example child-resistant packaging that is meant to resist tampering by a 5-year-old child for at least 5 min, giving an adult the opportunity to intervene, but parents and caregivers must still be made aware of the important of using adequate containers and store these products carefully away from children.23
Play, as was the case in other countries, was the activity involved in most traumatic eye injuries2,21,22 and in every age group, except adolescents aged more than 15 years, in which the leading activity involved in ocular trauma was sports. Still, it is possible that the number of injuries associated with sports is underestimated, as our study was conducted in public hospitals and many such cases are managed in private health facilities on account of the health insurance policies that cover these activities. Several paediatrics associations and agencies have published recommendations on protective eyewear for athletic activities,14 since there is evidence that correct utilization of protective eyewear reduces the risk of severe eye injuries by up to 90%. The development of a national strategy for the prevention of sports injuries in the paediatric population, including ocular trauma, would be beneficial, in addition to the implementation of programmes for prevention of sports-related injuries in schools and adequate training of athletic coaches and outdoor activity counsellors.
Some studies have reported causes of injury such as animal bites, firearms and fireworks2,12,20 that were not involved in any cases in our study, possibly due to cultural differences between the populations under study or to a decreasing trend in these causes in developed countries.22
Supervision continues to be an area in need of improvement. Up to one third of eye injuries in our series were not witnessed by an adult, a proportion that was higher than reported in the previous literature,20,21 although similar to the proportion observed in other types of unintentional injuries in Spain.24 This was even more frequent in children aged more than 10 years, and both of these factors (unwitnessed injury and age) were associated with a higher risk of immediate sequelae.
The initial assessment and correct management of patients with ocular trauma are essential to the prevention of severe sequalae. In many instances, adequate care requires consultation with other specialities, such as ophthalmology, to improve risk stratification and provide adequate treatment and follow-up of these injuries. In our study, we found a frequency of consultation that was similar to the frequency described by other authors,15 although only one of the participating hospitals had an ophthalmologist on site around the clock. Although the frequency of consultation could vary if continuous access to a specialist were more common, it does reflect the reality of care delivery in Spanish PEDs.
In our series, open-globe injuries (2.1% of cases, compared to 85.4% of cases of closed- globe injuries) were markedly less frequent compared to other studies, which report ratios of 1:1019 or even greater in developing countries.22
Schneider et al. reported hospital admission in up to 15% of cases,15 much higher compared to our case series. However, that figure included patients subjected to some form of procedure such as surgical repair of the injury, which would explain the greater frequency of admission compared to our sample. We did not find data in the reviewed literature on the frequency of admission in patients that seek care at the PED and do not require surgical intervention.2,3,25,26
Immediate sequelae were identified in 6.8% of patients, a proportion consistent with previous reports,6 most frequently acute vision loss. In the multivariate analysis, age more than 10 years, blunt trauma and the presence of refractory errors were independently associated with an increased frequency of immediate sequelae.
Since patients aged more than 10 years are the group at highest risk of sequelae, we should focus our education and prevention strategies on this population, developing interventions to be delivered in schools or parks, which are the settings where, based on our findings, most of the injuries occur in this age group. It is also important to address sports, keeping in mind the recommendations of different paediatrics associations and agencies for the safe practice of sports,14 which should be known to parents and coaches of children that play organized sports or play sports frequently.
Open-globe injuries are rare in paediatrics but are associated with a higher risk of vision loss, as observed in our study and previous studies, and poorer vision outcomes.27
Our study demonstrates injuries caused by blunt objects, such as toys, carry a higher risk of immediate sequelae. Although there are regulations to promote home safety that apply to furniture or toys, such as the Toy Safety Directive in Europe28 and the Royal Decree on the safety of toys published in the Boletín Oficial del Estado in Spain,29 which details the regulations pertaining to the manufacturing of toys to minimise physical injuries, we must emphasise the importance of providing a safe environment for children to play.
Refractive errors are a common disorder in the paediatric population, with an estimated prevalence of 1.5% to 5.5%,30 and our analysis found that their presence was associated with an increased risk of immediate sequelae. One possible explanation is that patients with refractive errors may wear corrective lenses that could make the injury worse, although we did not collect any data on this aspect. However, Kuhn et al. suggested that wearing glasses at the time of the injury could have a protective effect.1
These authors have proposed a score to predict the final visual outcome of eye injuries (Ocular Trauma Score)31,32 that has been validated, but we could not use it in our study because the particular circumstances of the paediatric emergency setting, the characteristics of paediatric patients and the lack of continuous access to an ophthalmologist in some of the hospitals precluded the assessment of visual acuity in all patients, which may have led to underdiagnosis.
In addition to what we have already mentioned, there are several limitations to our study. It may have underestimated the actual incidence of ocular trauma due to the collection of data exclusively in the PED setting, excluding patients managed at the primary care level, in outpatient urgent care clinics or in ophthalmology clinics. Nevertheless, we believe that obtaining data from the paediatric emergency care setting is essential for the purpose of developing prevention measures. Also, although the study was conducted in several PEDs, the participating hospitals were located in only 4 of the autonomous communities of Spain, so the epidemiological findings should be extrapolated with caution to other regions that were not represented in the sample. In addition, variations in the assessment and the absence of an ophthalmologist at the hospital could have had an impact on the visual sequelae that were detected. Lastly, we did not document the reason why consent was not sought in the cases that it was not, and this may mask missing cases of critical injuries that required care urgently.
One of the strengths of the study is that we achieved the estimated sample of ocular trauma cases, and therefore we consider that the identified risk factors can be generalised to the rest of the population and guide the development of preventive strategies. As we mentioned above, we did not find any other studies in the literature that carried out a similar analysis.
To conclude, ocular trauma is an important problem in the paediatric emergency setting given its potential ophthalmological sequelae. The setting and mechanism of eye injuries vary based on age. Age greater than 10 years, pre-existing refractive errors, blunt trauma and open-globe injuries seem to be predictors of immediate ophthalmological sequelae. An awareness of these risk factors is essential for the purpose of implementing preventive measures and prevent sequelae.
Conflicts of interestThe authors have no conflicts of interest to declare.
Rafael Marañón. Hospital General Universitario Gregorio Marañón. Madrid.
Ana Isabel Romero. Hospital General Universitario Gregorio Marañón. Madrid.
Carlos Miguel Angelats. Hospital Francesc de Borja. Gandía. Valencia.
Estefanía Romero Castillo. H. Universitario Puerta del Mar. Cádiz.
María Amalia Pérez Sáez. Hospital de Zumárraga. Guipúzcoa.
Susana Hernán-Gómez Vázquez. Hospital Universitario del Tajo. Aranjuez.
Please cite this article as: Mancebo JG, García-Loygorri CF, Romero AI, López PV, García AR. Traumatismo ocular en urgencias de pediatría, características y factores de riesgo de secuelas inmediatas. An Pediatr (Barc). 2021;94:161–172.
Previous presentation: this study was presented as an oral communication at the XXIV Annual Meeting of the Sociedad Española de Urgencias Pediátricas, 2019, Murcia, Spain.