The impact of maternal SARS-CoV-2 infection and its risk of vertical transmission is still not well known. Recommendations from scientific societies seek to provide safety for newborns without compromising the benefits of early contact. The aim of the study is to describe characteristics and evolution of newborns born to mothers with SARS-CoV-2 infection, as well as the implemented measures following recommendations from the Sociedad Española de Neonatología.
MethodsObservational, prospective and single-center cohort study. A specific circuit was designed for mothers with SARS-CoV-2 infection and their newborns. Epidemiological and clinical data were collected. PCR were performed in newborns at delivery and at 14 days of age.
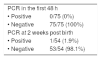
Results73 mothers and 75 newborns were included in the study. 95.9% of maternal infections were diagnosed during the third trimester of pregnancy, 43.8% were asymptomatic. Median gestational age was 38 weeks (IQR: 37–40), 25.9% of newborns required admission to Neonatology. Skin-to-skin mother care was performed in 68% of newborns, 80% received exclusive maternal or donated breast milk during hospital stay. No positive PCR results were observed in newborns at delivery, one case of positive PCR was observed in an asymptomatic neonate at 14 days of age.
ConclusionsRisk of SARS-CoV-2 transmission is low when complying to the recommendations issued by Sociedad Española de Neonatología, allowing rooming-in and promoting breastfeeding.
La repercusión de la infección materna por SARS-Cov-2 y su riesgo de transmisión vertical es aún poco conocido. Las recomendaciones de las sociedades científicas buscan proporcionar seguridad para el recién nacido sin comprometer los beneficios del contacto precoz. El objetivo del estudio es describir las características y evolución de recién nacidos de madres infectadas por SARS-CoV2, así como las medidas implementadas siguiendo las recomendaciones de la Sociedad Española de Neonatología.
Material y métodosEstudio observacional, prospectivo y unicentro de cohortes. Se diseñó un circuito específico para madres con infección por SARS-CoV2 y sus hijos. Se recogieron datos epidemiológicos y clínicos de las madres y sus recién nacidos. Se realizó PCR al nacer y a los 14 días.
ResultadosSe incluyeron 73 madres y 75 neonatos. El 95.9% de infecciones maternas fueron diagnosticadas durante el tercer trimestre, el 43.8% fueron asintomáticas. La mediana de edad gestacional fue 38 semanas (RIC:37–40), el 25.9% de los neonatos requirió ingreso. En el 68% se realizó contacto piel con piel en paritorio y el 80% recibieron lactancia materna o donada exclusiva durante su estancia. No se objetivaron resultados positivos de PCR en la primera muestra obtenida nada más nacer, se objetivó 1 caso de PCR positiva en un neonato asintomático a los 14 días.
ConclusionesEl riesgo de transmisión de la infección por SARS-CoV2 es bajo cumpliendo los protocolos de la Sociedad Española de Neonatología, permitiendo el alojamiento conjunto de madre e hijo, el contacto precoz y el establecimiento eficaz de la lactancia materna.
The discovery of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) as the causative agent of coronavirus disease 2019 (COVID-19)1 and the global pandemic that emerged in late 2019 have raised significant concerns regarding infection in vulnerable populations, such as pregnant women and newborn infants. The impact of maternal infection during pregnancy, the probability of vertical transmission in utero, during childbirth or through breastfeeding and the impact of infection in affected neonates in the medium and long term continue to be poorly understood.
Several authors have suggested the possibility of in utero transmission,2–7 and while most diagnostic tests performed in infants born to infected mothers have been negative,8–11 the virus has been found in the placenta, amniotic fluid and occasionally breastmilk in the absence of clear evidence of neonatal infection.4,12,13 Most of the evidence on neonatal infection consists of single case reports, case series and some articles that review them,14–16 in addition to expert consensus recommendations developed by different scientific societies,17–20 with substantial differences between them.
Due to the scarcity of evidence from large case series, a cautious approach must be adopted in the management of at-risk neonates, although always taking into account the negative impact of separating mother and child. Practices such as skin-to-skin contact and the establishment of breastfeeding offer considerable and proven benefits to the mother-child dyad, both in the short and the long term,21,22 so emphasis must be placed on developing recommendations on safety measures for the newborn infant without compromising these benefits.23
The aim of our study was to describe the characteristics and outcomes of neonates born to mothers with SARS-CoV-2 infection delivered in a hospital with a level IIIC neonatal intensive care unit (NICU) and the approach to the care of these patients in adherence with the recommendations of the Sociedad Española de Neonatología (Spanish Society of Neonatology, SENeo).
Material and methodsStudy design and data collectionWe conducted an observational cohort study in a single centre in the department of neonatology of a tertiary care hospital that manages approximately 5500 deliveries a year. We included pregnant women with SARS-CoV-2 infection confirmed by a polymerase chain reaction (PCR) test in a nasal swab sample between March 1 and August 17, 2020. In adherence with the recommendations of the SENeo, following delivery, neonates that did not require hospital admission were roomed with their mothers while implementing the recommended mother-child isolation measures (use of surgical masks and hand hygiene).
In March and April, pregnant women with symptoms suggestive of SARS-CoV-2 infection underwent a PCR test and from May 6, we screened all pregnant women admitted to the maternity ward with or without symptoms. The diagnosis of SARS-CoV-2 infection was made through viral PCR testing of nasal swab samples (TaqPath™ Multiplex, ThermoFisher). Pregnant women with a positive PCR test that did not give birth within a week from the test and pregnant women with previous evidence of infection during pregnancy underwent a second PCR at the time of delivery. Every neonate underwent collection of a nasal swab sample at birth for performance of the SARS-CoV-2 PCR test. After discharge, the follow-up was conducted by telephone, and families were offered an optional in-person visit at 15 days with repetition of the viral PCR test, and we included the PCR test results at this time point (15 days) for those infants for which they were available.
The data collection was prospective for mothers and infants. We collected data for epidemiological, clinical and laboratory variables. We considered the presentation mild if it was limited to upper respiratory symptoms, fever or anosmia. The statistical analysis was performed with the software SPSS version 23. The study was approved by the research ethics committee of the hospital. We adhered to the principles of the Declaration of Helsinki at all times.
Care circuit. Rooming-in in isolationWe established a specific care circuit in the department of gynaecology, obstetrics and neonatology of the hospital for mothers that tested positive for SARS-CoV-2, reserving up to 16 beds in individual rooms in the high-risk maternity unit for pregnant women or mothers at 22 or more weeks of gestation or greater, and another 19 beds in the high-risk maternity unit for pregnant women and mothers at less than 22 weeks of gestation. A multidisciplinary team of obstetricians, gynaecologists, paediatricians and neonatologists was in charge of the management of these mothers and neonates, with the additional support of paediatric intensivists, internists and anaesthesiologists if the mother experienced moderate to severe respiratory failure.
Induction of labour was performed in the ward, and we allocated 3 delivery rooms and 1 operating room for performance of caesarean deliveries to this care circuit. After delivery, in the first 24 h of the hospital stay, we collected nasopharyngeal swab samples for performance of PCR from every infant born to a mother with a positive SARS-CoV-2 test, and, if the clinical condition of both mother and child allowed it, the infant roomed in with the mother while adhering to applicable isolation measures.
In case of vaginal delivery, we transferred the mother directly from the delivery room to her room in the maternity ward, and in case of caesarean delivery, the mother remained in the operating room for the immediate postoperative period, after which she was admitted to the maternity ward if her clinical condition allowed it. The hospital allowed a companion, usually the father, to stay along during the period of isolation in the maternity ward. We provided breastfeeding education and support to the mothers, explaining the benefits and potential risks known to date, and recommending maternal milk over formula based on the recommendations of the SENeo and the most recent evidence.
If the neonate required hospital admission, the patient stayed in an individual negative pressure room in the NICU while awaiting the results of the PCR test of the nasopharyngeal swab sample. The indications for neonatal admission due to potential SARS-CoV-2 infection were respiratory symptoms or severe illness in the mother in the absence of an alternative caregiver for the child.
In infants that did not require admission to the neonatal unit, the time of discharge was selected on a case-by-case basis depending on the clinical stability of the patient and presence or absence of other risk factors. Some infants were discharged early, defined as discharge before 48 h post birth. In case of early discharge, we scheduled an outpatient follow-up visit in the department of neonatology at 48 h post birth to collect the heel prick blood sample for newborn metabolic screening and perform a clinical evaluation of both mother and child.
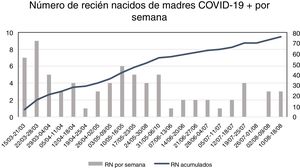
ResultsWe included a total of 73 mothers with evidence of infection by SARS-CoV-2 between March 15 and August 17, 2020. The median maternal age was 34 years (interquartile range [IQR], 27–37), 71 had singleton pregnancies and 2 had twin pregnancies. Maternal infection was diagnosed in the third trimester in 95.9% of cases and in the second trimester in 4.1% of cases. Twenty-six mothers that were given a diagnosis of SARS-CoV-2 infection more than 2 weeks before delivery underwent a second PCR test in a nasopharyngeal swab sample, with negative results in 11 (15.1% of the total). Table 1 summarizes the epidemiological and clinical characteristics of the mothers, and Fig. 1 presents the number of infants born per week.
Epidemiological characteristics of mothers with SARS-CoV-2 infection.
| Underlying disease in the mother | |
|---|---|
| • Obesity | 8/73 (10.9%) |
| • Respiratory disease | 2/73 (2.7%) |
| • Cardiovascular disease | 1/73 (1.4%) |
| • Autoimmune disease | 1/73 (1.4%) |
| • Primary thrombophilia | 1/73 (1.4%) |
| • Thyroid disease | 1/73 (1.4%) |
| Symptom severity | |
| • Asymptomatic | 32/73 (43.8%) |
| • Mild symptoms | 22/73 (30.1%) |
| • Required admission | 17/73 (23.3%) |
| • Required intensive care | 2/73 (2.7%) |
| Symptoms | |
| • Cough | 29/41 (70.7%) |
| • Fever | 27/41 (65.9%) |
| • Breathing difficulty | 17/41 (41.5%) |
| • Anosmia/ageusia | 7/41 (17.1%) |
| • Myalgia | 6/41 (14.6%) |
| Type of pregnancy | |
| • Singleton | 71/73 (96.4%) |
| • Twin | 2/73 (3.6%) |
| Pregnancy complications | |
| • Gestational diabetes | 3/73 (4.1%) |
| • Preeclampsia | 1/73 (1.4%) |
| Antenatal corticosteroids | 6/73 (8.2%) |
| Type of delivery | |
| • Spontaneous vaginal | 38/73 (52.1%) |
| • Instrumental delivery | 9/73 (12.3%) |
| • Elective caesarean | 20/73 (27.4%) |
| • Emergency caesarean | 6/73 (8.2%) |
| Lymphopenia (WBC < 1000) | 26/73 (35.6%) |
| C-reactive protein, median (IQR) | 3.5 (0.95−7.12) |
Maternal clinical and epidemiological characteristics. The frequency of specific symptoms is reported relative to the total of pregnant women with symptoms.
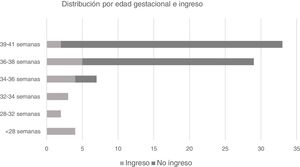
As for the neonates, the median birth weight was 3050 g (IQR, 2780–3450) and the median gestational age 38 weeks (IQR, 37–40), and 20% of infants were born preterm (15/75). Fig. 2 presents the distribution of births and admissions to the neonatal unit by gestational age. The median Apgar score at 1 min was 9 points and the median 5-min score was 10 points. Twelve patients (16%) required resuscitation, of who 1, born at 24 weeks’ gestational age, required intubation in the delivery room. A total of 19 infants (25.3%) required admission, most frequently due to prematurity; Table 2 presents the reasons for admission to the neonatal unit. Two infants died (2/75; 2.7%), one from necrotising enterocolitis associated with preterm birth (24 weeks) and one from severe hypoxic-ischaemic encephalopathy. Skin-to-skin contact was provided in the delivery or operating room in 51 cases (68%), and delayed cord clamping was practised in 43/75 (57.3%). The feeding modality during the hospital stay was exclusive breastfeeding with maternal milk in 48 neonates (64%) and with a combination of maternal and donor human milk in 12 (16%), mixed breastfeeding in 7 (9.3%) and formula feeding in 8 (10.7%). In every case in which neither the mother or the newborn required admission, newborns roomed in with their mothers in the maternity ward (56/75; 74.7%). The median chronological age at the time of the first PCR test was 8 h (IQR, 0–19). Table 3 presents the results of the viral PCR tests performed at birth and 2 weeks post birth.
The first sample for PCR (median age at time of collection, 8 h; IQR, 0–18) was negative in the 75 cases included in the study. The median age at discharge, including both patients admitted to hospital and those discharged from the maternity ward, was 48 h (IQR, 48−48). We collected an additional sample for PCR at 14 days post birth in 54 neonates (72%), all of who were asymptomatic at the time of the checkup. The results were negative in 53, and the test was positive in 1 patient that underwent 2 more tests until a negative result was obtained 2 weeks later, a neonate that remained asymptomatic throughout the follow-up.
DiscussionThis study describes the experience in the management of mothers with confirmed SARS-CoV-2 infection and their newborn infants in a tertiary care hospital. This is one of the first neonatal cohorts described in the literature, including patients managed in a tertiary care hospital with a substantial number of COVID-19 cases. We did not find any cases of confirmed vertical infection, and only one of the neonates had a positive PCR test at 15 days post birth, probably resulting from horizontal transmission in the community.
Since the pandemic started, the recommendations management of infected mothers and newborn infants at risk of vertical or horizontal transmission have undergone modifications to adapt to the evidence available at each time.24 The earliest data on newborn infants are from single case report and small case series that gave rise to the initial recommendations in China17 and the United States.18
In Spain, paediatric19 and neonatal20 guidelines have also been published. Updates to neonatal guidelines have been published on the website of the SENeo, including case definitions, data on the probability of vertical transmission and recommendations for the management of mothers or infants with confirmed infection. The recommendations prioritize avoiding the separation of the mother and child with rooming-in arrangements as long as the health of both patients allows it and maintaining appropriate precautions, such as use of masks and hand hygiene. The recommendation of preserving rooming-in is based on the importance of establishing breastfeeding and the known benefits of early mother-child contact, along with the low evidence of the risk of transmission and the low severity of the documented cases of confirmed horizontal infection in neonates. The discharge criteria for neonates with negative viral tests were the same as usual, with emphasis placed on the importance of informing families about the infection and the possibility of transmission, supporting families throughout the hospital stay and ensuring adequate follow-up thereafter.
In the cohort under study, none of the 75 infants born to mothers with SARS-CoV-2 infection tested positive for SARS-CoV-2 during the hospital stay. There are reports in the literature of identification of SARS-CoV-2 in biological specimens (including samples of placenta and amniotic fluid)3,4,12 which suggest that vertical transmission is possible, although the evidence to date shows that it is infrequent. A cohort study conducted in the United States by Salvatore et al25 that included 116 mothers found no cases of perinatal transmission, and a meta-analysis by Kotlyar et al. that includes some of these data reported a frequency of potential vertical transmission of 2.7%,16 similar to the frequency observed by Dumitriu et al. in a cohort study conducted in New York,7 although it is likely that some of these infections resulted from horizontal transmission. A meta-analysis published by Raschetti et al26 included 176 cases of neonatal infection, of which the authors attributed 70% to horizontal transmission and 30% to vertical transmission. Taking this evidence into account, the prevention of horizontal transmission should be prioritised in these neonates, as the impact of infection in this population is still poorly understood. Our findings demonstrate that adherence to the recommendations of the SENeo with an emphasis on hand hygiene and the use of masks makes rooming-in possible, promoting mother-child bonding and maintenance of breastfeeding without compromising the safety of the neonate.
The data on the medium- to long-term repercussions and risk of infection following discharge are scarce, and we did not address these aspects in this initial study. We need to continue expanding our knowledge on SARS-CoV-2 infection in the neonatal population, and the mechanisms and risk of vertical and horizontal transmission, the development of immunity to the virus, the respiratory sequelae of these infections or coinfections by other respiratory pathogens are some of the issues that concern paediatricians that will probably become better understood in upcoming months.
There are several limitations to the study. It was conducted in a single centre, which may limit its external validity. The sample was small and the follow-up finished at 15 days post birth, so we could not draw conclusions regarding the safety of the recommended measures beyond that time point or about neonatal infections in the medium to long term. Given the scarcity of the data on vertical transmission or the course of disease in neonatal patients, our findings should be interpreted with caution as we await evidence from studies with larger samples and longer durations of follow-up.
Some of the data included in this study have been added to the national COVID-19 register of the SENeo, and a report on the data of this registry is currently in press.
It seems reasonable to conclude that following the recommendations of the SENeo with adherence to established precautions, the risk of vertical or horizontal transmission of SARS-CoV-2 is low, which allows rooming-in, early mother-child contact from birth including kangaroo care and effective establishment of breastfeeding. Further research is required to increase our knowledge of the epidemiology, pathophysiology and short- and long-term impact of maternal and neonatal infections by SARS-CoV-2.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Solís-García G, Gutiérrez-Vélez A, Pescador Chamorro I, Zamora-Flores E, Vigil-Vázquez S, Rodríguez-Corrales E, et al. Epidemiología, manejo y riesgo de transmisión de SARS-CoV-2 en una cohorte de hijos de madres afectas de COVID-19. An Pediatr (Barc). 2021;94:173–178.