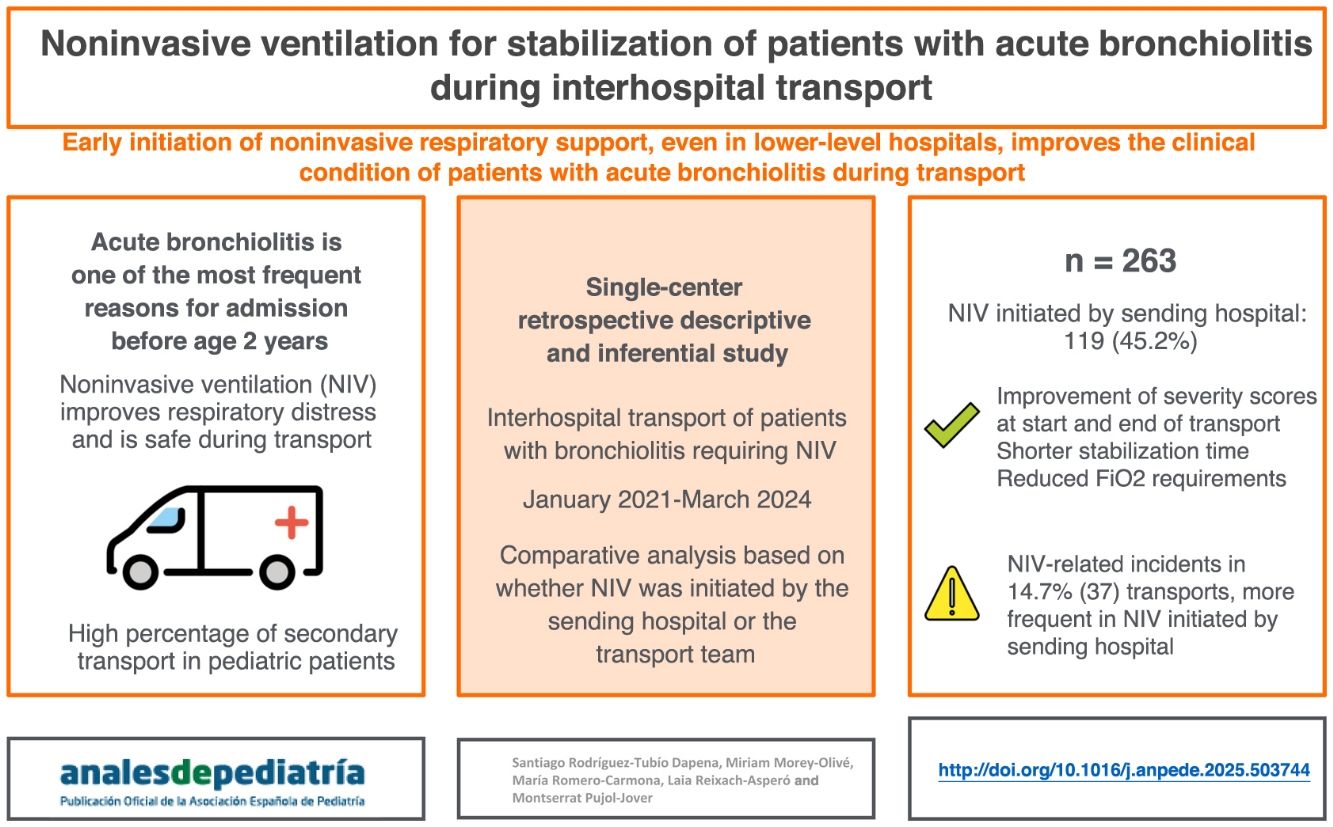
To describe and compare the characteristics of patients with acute bronchiolitis (AB) transported between hospitals with noninvasive ventilation (NIV), initiated either by the paediatric transport team (PTT) or by the sending hospital (SH).
MethodsRetrospective, observational, single-centre study conducted by one PTT. We included all transports between 2 hospitals of patients with AB in which NIV was used between January 2021 and March 2024.
ResultsThe sample included 263 transports with NIV, with initiation of NIV by the SH in 119 (45.2%) and by the PTT in 144 (54.8%). Initiation of NIV by the SH was associated with a shorter stabilization time, with a median of 40min (IQR: 33.3–47) compared to initiation by the PTT group, with a median of 47min (IQR: 40–56). The scores in the BROSJOD severity scale and the oxygen requirements were lower, both at the beginning and at the end of transport, in the group of patients in whom NIV was initiated at the SH. Incidents were documented in 14.1% (n=37) of transports, with a higher frequency of minor complications in the SH-initiated group, chiefly leaks and patient-ventilator asynchrony.
ConclusionsPatients with bronchiolitis who required transport with NIV benefited from early initiation of support in RH, as they were in better clinical condition during transport. Training SH staff in the use of NIV could decrease the incidence of the potential complications associated with this technique.
Describir y comparar las características de los pacientes con bronquiolitis aguda (BA) trasladados entre hospitales con ventilación no invasiva (VNI), iniciada bien por el equipo de transporte pediátrico (ETP) o por el hospital emisor (HE).
MétodosEstudio retrospectivo, observacional y unicéntrico realizado por un ETP. Se incluyeron todos los pacientes con BA trasladados con VNI entre dos hospitales entre enero de 2021 y marzo de 2024.
ResultadosSe incluyeron en el estudio 263 pacientes trasladados con VNI; en 119 (45,2%) el soporte fue iniciado por el HE y en 144 (54,8%), por el ETP. El inicio de VNI por el HE se asoció a un menor tiempo de estabilización, mediana de 40minutos, rango intercuartílico (RIQ) de 33,3-47minutos, en comparación con los del grupo ETP, con 47 (RIQ: 40-56)minutos. Se objetivó una menor puntuación en la escala de gravedad BROSJOD y de las necesidades de oxígeno en el grupo de pacientes de VNI en HE tanto al inicio como al final del traslado. Se registraron incidencias en un 14,1% (37) de los traslados, que fueron más frecuentes en el grupo de HE, siendo en su mayoría fugas y desadaptación.
ConclusionesLos pacientes con BA que precisaron traslado con VNI se beneficiaron de un inicio precoz del soporte, trasladándose en mejores condiciones clínicas. Formar al personal de los HE en el uso de la VNI podría disminuir las complicaciones relacionadas con su uso.
Acute bronchiolitis (AB) is a form of lower respiratory tract infection of viral etiology characteristic of the pediatric age group. This disease is one of the leading reasons for hospital admission in infants and young children, and up to 10% of these patients require admission to the pediatric intensive care unit (PICU).1 In out-of-hospital settings, it is associated with a high frequency of transport of critically ill pediatric patients, with wide variation in severity.2 At present, there is no specific treatment for AB, and its management is based on providing respiratory support adapted to the severity of disease.
In patients with severe AB, the use of noninvasive ventilation (NIV) in the PICU has been found to improve respiratory distress and reduce the need of invasive mechanical ventilation, so it has become widespread.3,4 A similar trend has been observed in pediatric interhospital transport, and several studies suggest that its use is safe and feasible in this context.5,6 Moreover, there is evidence that early initiation of NIV is associated with a decrease in severity scores and an improvement in vital signs during interhospital transport7 without an increase in the rate of emergency intubation during transport.8,9
The aim of our study was to describe and compare the characteristics of patients with AB undergoing interhospital transport with NIV, initiated by either the pediatric transport team (PTT) or the sending hospital (SH).
MethodsWe conducted a single-center retrospective and observational study in a tertiary care hospital that has a specialized pediatric ground transport team comprised of an emergency medical technician, a pediatric nurse and an intensive care pediatrician. In addition, the medical emergency response coordinating center has an intensive care pediatrician on staff that communicates with both the SH and the PTT and can provide guidance to both during transport.
The study was conducted between January 2021 and March 2024. We included all patients aged less than 24 months with a diagnosis of AB transported from one hospital to another by the PTT in whom NIV was initiated at some point during stabilization or transport and who received NIV during transport. The transports originated in one of 37 possible sending hospitals and ended at one of the 8 tertiary care hospitals that have a PICU in Catalonia.
We defined AB as the first episode of lower respiratory tract infection of viral etiology in a patient aged less than 24 months preceded by a viral upper respiratory prodrome.10
During transport, NIV was delivered with the Hamilton T1 respirator (Hamilton Medical AG, Switzerland) to both pediatric and neonatal patients. The interfaces were face masks or, in some neonates, nasal masks, depending on the fit on the patient.
We excluded patients with a personal history of AB, a diagnosis of respiratory disease in the neonatal period or other respiratory diseases that did not meet the criteria for AB. We also excluded transports ending but not starting in a hospital (from primary care centers), that were cancelled or in which NIV was not the modality used for respiratory support.
The study was approved by the Ethics Committee of the hospital where it was conducted.
Geographical contextOur PTT serves the autonomous community of Catalonia as well as Andorra.
The sending hospitals requesting patient transport are usually local secondary care hospitals or hospitals that offer pediatric care but do not have a PICU. Most pediatricians in these hospitals are not intensive care specialists, but some centers have the necessary resources to initiate respiratory support with NIV and for the basic management of this technique. The receiving hospital (RH) to which patients are transported is usually the referral hospital in the catchment area that has a PICU.
Study variablesWe retrieved data on clinical and transport characteristics from the Research Electronic Data Capture (REDCap) database. We followed up on the patients by calling the receiving hospital 72h after transport. The data collection and follow-up telephone call are performed routinely in every transport conducted by the PTT.
We retrieved data for the following variables: demographic characteristics (age, sex and weight), clinical characteristics during transport (data concerning the transport, severity scores, respiratory support and ventilation parameters) and clinical characteristics at follow-up (need of orotracheal intubation [OTI] at the RH, microbial isolation, death). All the clinical variables were documented at each of the transport stages (arrival to SH, departure from SH, transport and arrival to RH). The stabilization time was defined as the time elapsed from arrival of the transport team to the SH to the departure from the SH. We identified 4 epidemic seasons associated with peaks in AB incidence in the period under study: 2021, 2021–2022, 2022–2023 and 2023–2024. We divided each year into two semesters, starting with the first semester of 2021, and following without interruption until the end of the study period.
We reviewed the NIV-related incidents documented in the records for each transport, classifying them into the following categories: ventilator malfunction, incorrect interface/circuit setup, incorrect ventilator parameters, significant leak, patient-ventilator asynchrony, desaturation during transport (peripheral oxygen saturation<90%) and pneumothorax. We categorized incidents that had a significant impact on the patient as “serious” (pneumothorax, severe hypotension, bronchial aspiration, cardiac arrest) and those without a significant impact on the patient as “minor” (patient-ventilator asynchrony, significant leaks [>50%], incorrect ventilator parameters, incorrect interface/circuit setup without clinical impact, transient desaturations during transport). We assigned NIV-related incidents identified by the PTT in the time spent at the SH to the group of patients with NIV initiation by the SH.
We assessed the severity of the AB episode by means of the Bronchiolitis Score of Sant Joan de Déu (BROSJOD score)11 in the group of patients in whom it had been correctly documented by the PTT before departing the SH and on arrival to the RH.
Statistical analysisThe continuous data did not follow a normal distribution, so we summarized them as median and interquartile range (IQR). Qualitative data were summarized as absolute frequencies and proportions. We conducted an analysis to compare patients in whom NIV was initiated by the SH versus patients in whom it was initiated by the PTT. Continuous data were compared by means of the Mann–Whitney U test and qualitative data with the χ2 test. To assess the correlation between continuous variables, we used the Spearman correlation coefficient. We defined statistical significance as a P value of less than 0.05. The clinical data were collected in a database and analyzed with the software IBM SPSS Statistics for Windows, version 25.0 (IBM Corp; Armonk, NY, USA).
The clinical outcomes were the time to stabilization, BROSJOD severity score before and after transport, need of OTI at the RH in the 72h following transport, NIV-related incidents and changes in respiratory parameters.
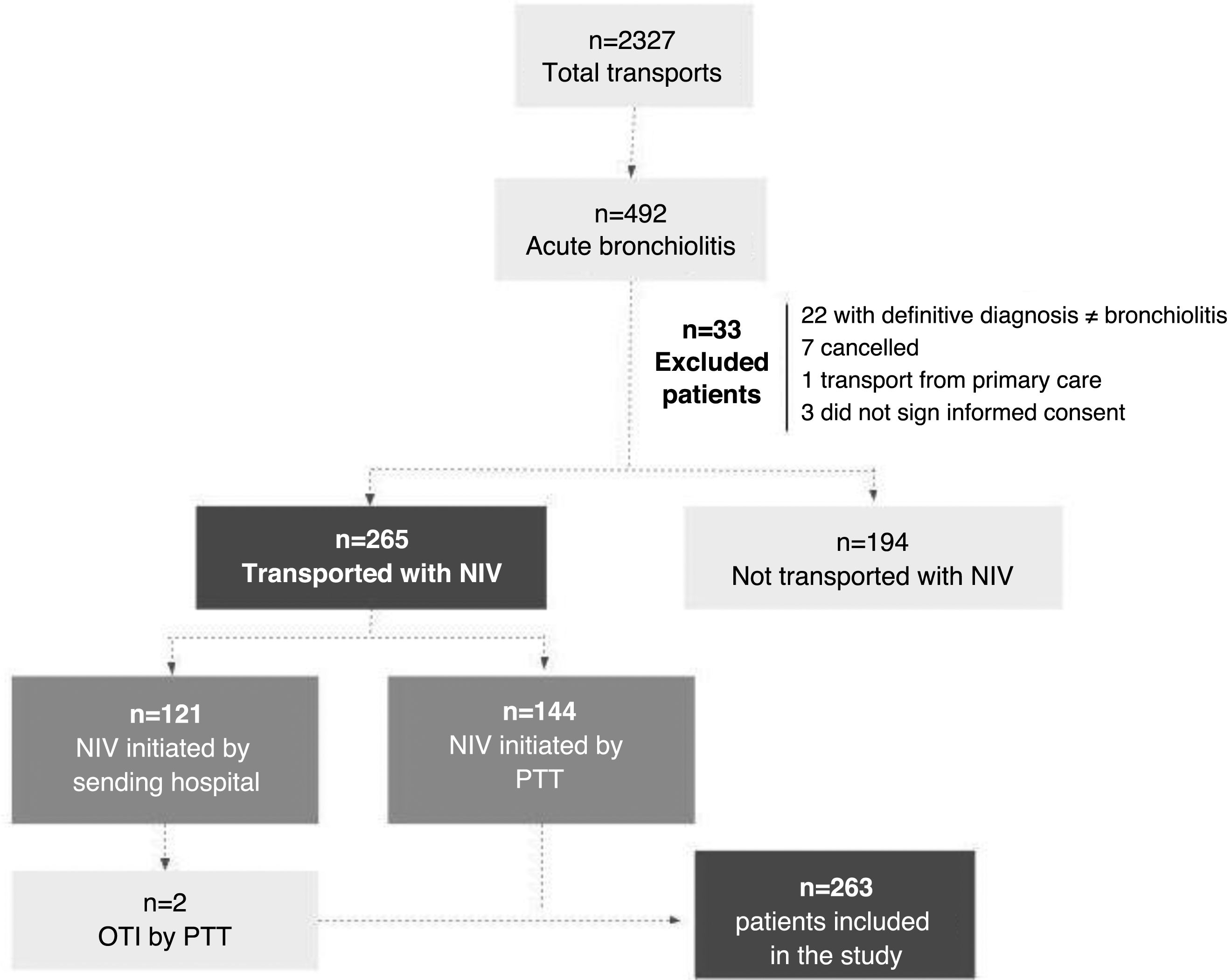
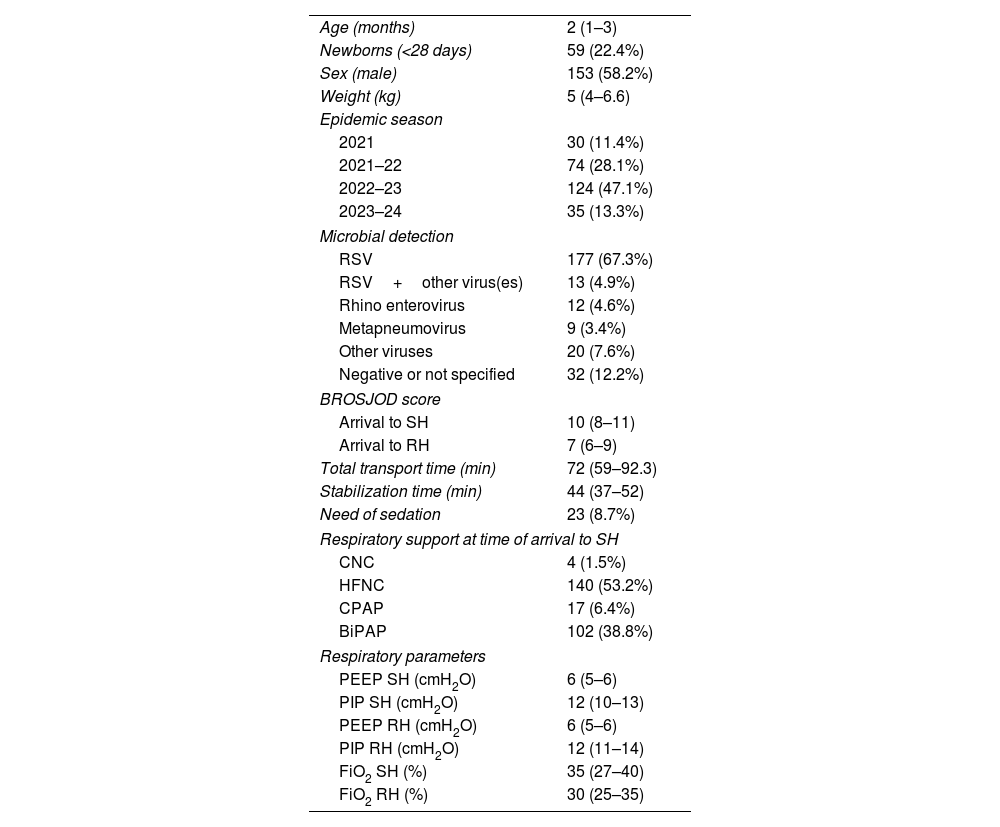
ResultsDuring the study period, 2327 patients underwent interhospital transport, of who 492 (21.1%) had a diagnosis of AB and 263 were included in the study (Fig. 1). In 119 cases (45.2%), NIV was initiated by the SH and in 144 (54.8%) it was not initiated until the arrival of the PTT. Only 2 patients in whom NIV was initiated by the SH required OTI once the PTT arrived for stabilization before transport, and they were excluded from the analysis. Table 1 presents the main clinical characteristics of the sample. The NIV modality used during transport was bilevel positive airway pressure (BiPAP) in most patients (n=259; 98.5%) and continuous positive airway pressure (CPAP) with a nasal interface in only four. When NIV was initiated by the SH, the interface was a face mask in most cases (102/119; 85.7%), and a nasal mask in only 17 (14.3%), which was switched to a face mask for transport in 13 cases.
Main characteristics of the patients that underwent interhospital transport with noninvasive ventilation.
| Age (months) | 2 (1–3) |
| Newborns (<28 days) | 59 (22.4%) |
| Sex (male) | 153 (58.2%) |
| Weight (kg) | 5 (4–6.6) |
| Epidemic season | |
| 2021 | 30 (11.4%) |
| 2021–22 | 74 (28.1%) |
| 2022–23 | 124 (47.1%) |
| 2023–24 | 35 (13.3%) |
| Microbial detection | |
| RSV | 177 (67.3%) |
| RSV+other virus(es) | 13 (4.9%) |
| Rhino enterovirus | 12 (4.6%) |
| Metapneumovirus | 9 (3.4%) |
| Other viruses | 20 (7.6%) |
| Negative or not specified | 32 (12.2%) |
| BROSJOD score | |
| Arrival to SH | 10 (8–11) |
| Arrival to RH | 7 (6–9) |
| Total transport time (min) | 72 (59–92.3) |
| Stabilization time (min) | 44 (37–52) |
| Need of sedation | 23 (8.7%) |
| Respiratory support at time of arrival to SH | |
| CNC | 4 (1.5%) |
| HFNC | 140 (53.2%) |
| CPAP | 17 (6.4%) |
| BiPAP | 102 (38.8%) |
| Respiratory parameters | |
| PEEP SH (cmH2O) | 6 (5–6) |
| PIP SH (cmH2O) | 12 (10–13) |
| PEEP RH (cmH2O) | 6 (5–6) |
| PIP RH (cmH2O) | 12 (11–14) |
| FiO2 SH (%) | 35 (27–40) |
| FiO2 RH (%) | 30 (25–35) |
Abbreviations: BiPAP, bilevel positive airway pressure; BROSJOD, Bronchiolitis Score of Sant Joan de Déu; CNC, conventional nasal cannula; CPAP, continuous positive airway pressure; HFNC, high-flow nasal cannula; FiO2, fraction of inspired oxygen; PEEP, positive end-expiratory pressure; PIP, peak inspiratory pressure; RH, receiving hospital; RSV, respiratory syncytial virus; SH, sending hospital l.
Continuous variables are expressed as median (IQR). Qualitative variables are expressed as absolute frequencies and percentages.
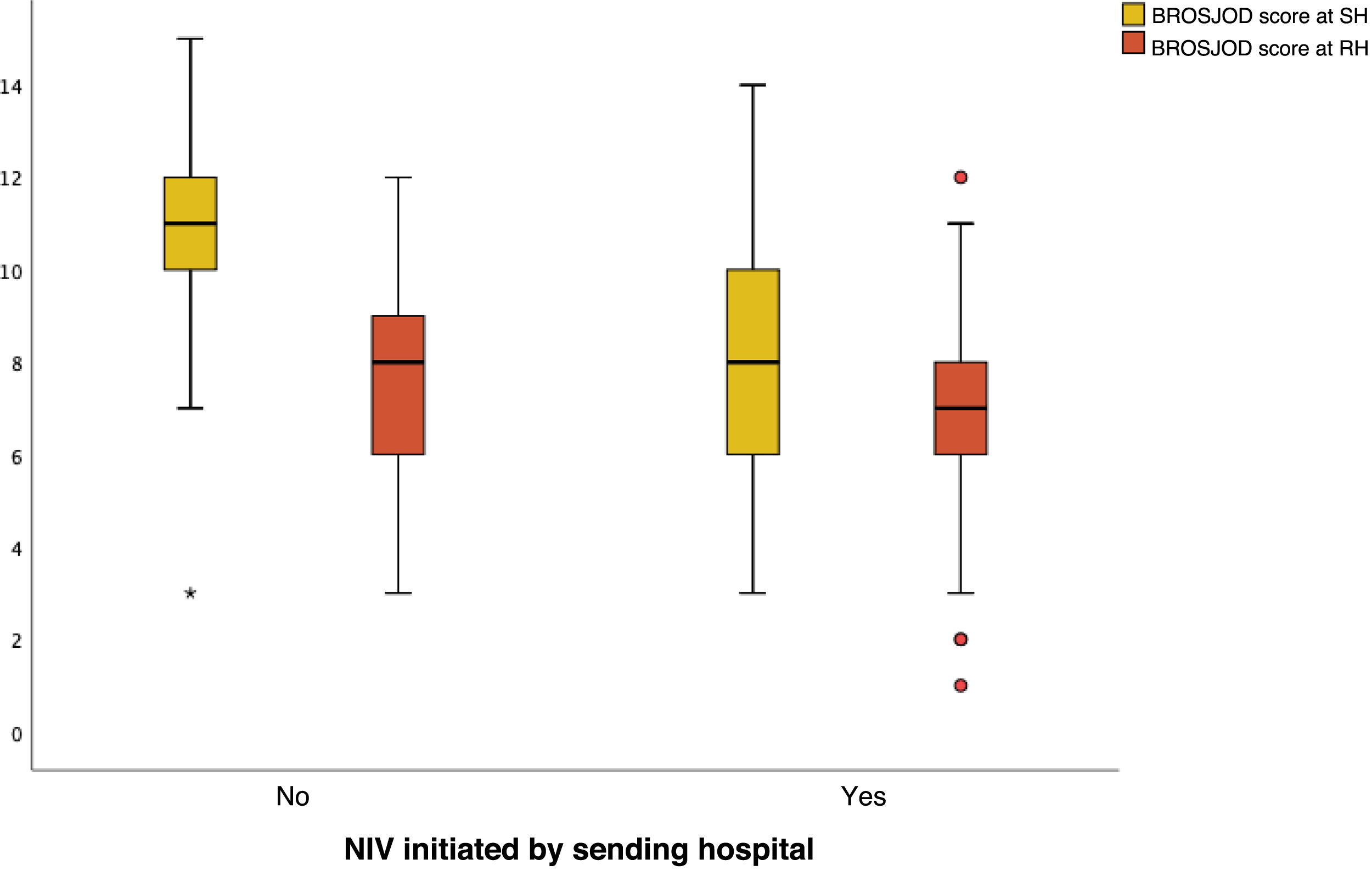
We found significant differences in the BROSJOD severity scores (Fig. 2). Initiation of NIV before activation of the PTT was associated with lower scores on arrival of the PTT to the SH, with a median score of 8 (IQR, 6–10) compared to patients in which initiation of NIV was deferred until the arrival of the PTT, with a median score of 11 (IQR, 10–12) (P<0.0001). When it came to the severity score at the end of transport, the median was 8 in the group with initiation of NIV by the SH compared to 7 (IQR, 6–8) in the other group, with a P value that neared the threshold of significance (P=0.052). The PTT was unable to record the BROSJOD score at the SH in 14 patients (5.3%) and on arrival to the RH in 15 patients (5.7%).
Comparison of severity scale in interhospital transport. The group of patients with initiation of NIV by the SH is to the right, and the group with initiation by the transport team the left. The boxes span the interquartile range (IQR) and the line in the middle of the box the median. The whiskers extend to the minimum and maximum values within 1.5 times the IQR. Values outside this range were treated as outliers.
BROSJOD, Bronchiolitis Score of Sant Joan de Déu; NIV, noninvasive ventilation; RH, receiving hospital; SH, sending hospital.
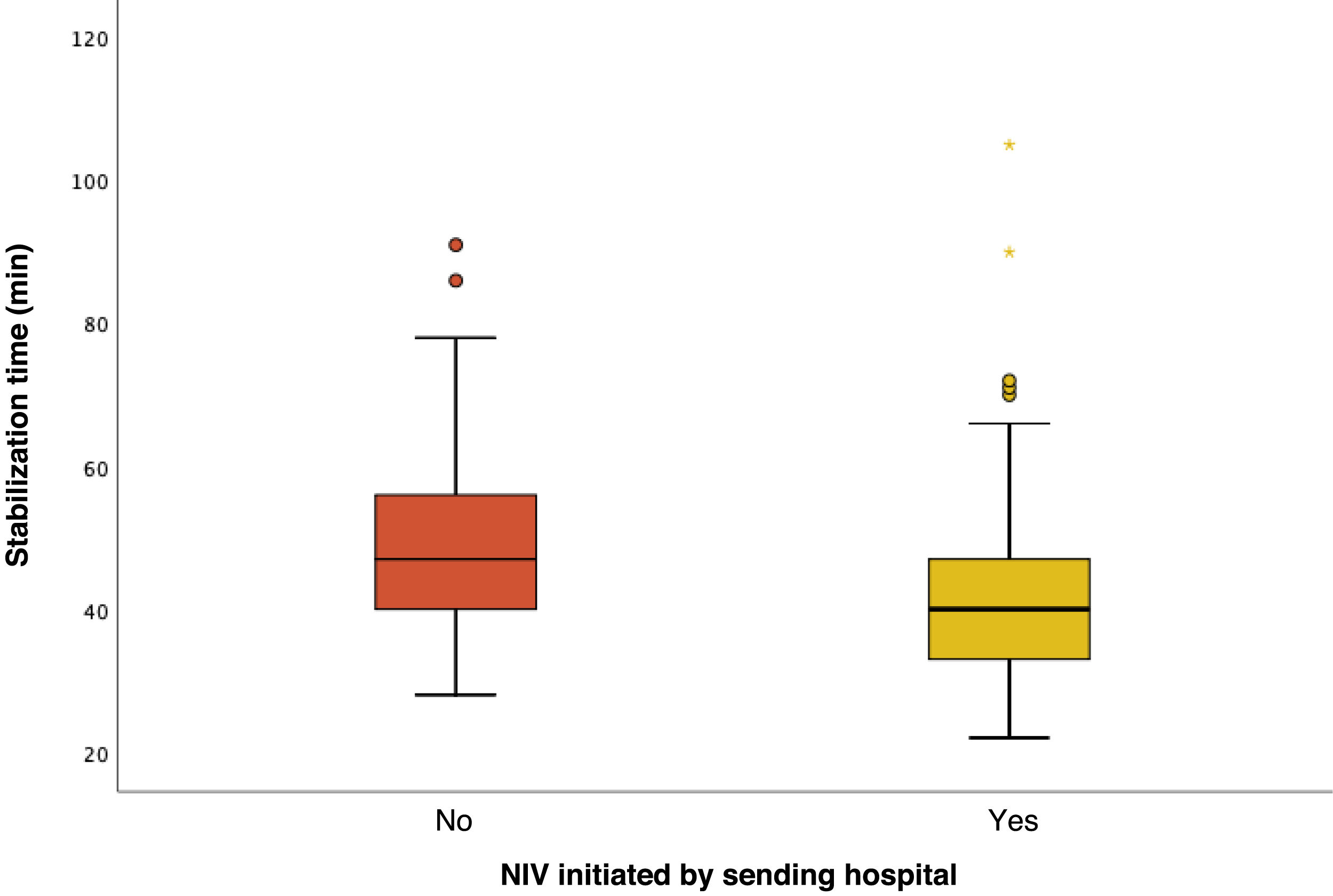
In the analysis of the stabilization time, we identified several outliers that we explored individually. In one patient in whom NIV was initiated by the SH, the stabilization time was 126min, and the delay in transport was due to waiting for the arrival of another unit to transport an additional patient. Since the reason for the delay was unrelated to the patient’s transport, this case was excluded from the analysis. Initiation of NIV by the PTT was significantly associated with a longer stabilization time, with a median of 47min (IQR, 40–56) compared to 40 (IQR, 33.3–47) in patients in whom NIV was initiated beforehand (P<0.0001) (Fig. 3). Furthermore, the stabilization time was weakly correlated to the severity score at the time of arrival of the PTT to the SH (r=0.21; P=0.001). On the other hand, the stabilization time was not associated with the need for sedation or the occurrence of incidents during transport.
Comparison of stabilization time in interhospital transport. The boxes span the interquartile range (IQR) and the line in the middle of the box the median. The whiskers extend to the minimum and maximum values within 1.5 times the IQR. Values outside this range were treated as outliers.
We found an association between the initiation of NIV by the SH and a lower fraction of inspired oxygen (FiO2), both at the beginning and at the end of transport, compared to the group with initiation of NIV by the PTT. In patients in whom NIV was initiated by the SH, the median FiO2 was 0.3 (IQR, 0.25–0.35) at the beginning of transport and 0.25 (IQR, 0.25–0.3) at the end, while in the group with initiation of NIV by the PTT the corresponding median FiO2 values were 0.35 (IQR, 0.3–0.45) and 0.3 (IQR, 0.25–0.35), respectively. These differences were statistically significant (P<0.0001 and P<0.002, respectively). When it came to respiratory parameters, we did not find differences in the peak inspiratory pressure (PIP) and positive-end expiratory pressure (PEEP) between the groups.
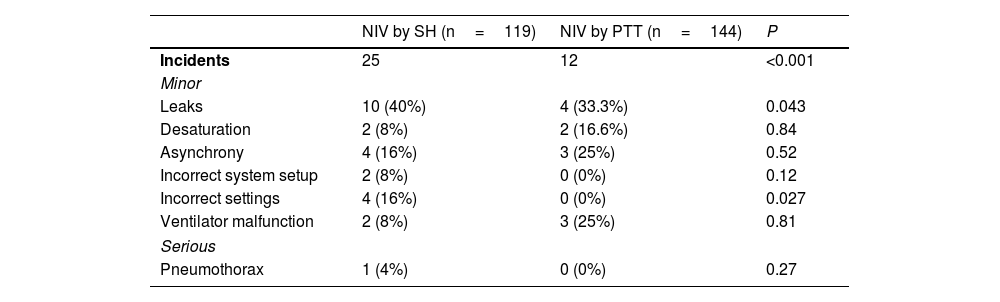
Incidents related to NIV were documented in 37 transports (14.1%), with a higher frequency in the group with NIV initiation by the SH compared to the group with initiation by the PTT (25 [21%] vs 12 [8.3%]; P=0.003). The most frequent incidents in both groups were leaks (14/37; 37.8%). Table 2 presents the distribution of incidents by type and the differences between groups. There was one case of pneumothorax recorded by the PTT on arrival to the SH that did not require pleural drainage until the second day of hospitalization in the RH.
Incidents related to NIV documented in transported patients.
| NIV by SH (n=119) | NIV by PTT (n=144) | P | |
|---|---|---|---|
| Incidents | 25 | 12 | <0.001 |
| Minor | |||
| Leaks | 10 (40%) | 4 (33.3%) | 0.043 |
| Desaturation | 2 (8%) | 2 (16.6%) | 0.84 |
| Asynchrony | 4 (16%) | 3 (25%) | 0.52 |
| Incorrect system setup | 2 (8%) | 0 (0%) | 0.12 |
| Incorrect settings | 4 (16%) | 0 (0%) | 0.027 |
| Ventilator malfunction | 2 (8%) | 3 (25%) | 0.81 |
| Serious | |||
| Pneumothorax | 1 (4%) | 0 (0%) | 0.27 |
NIV, noninvasive ventilation; PTT, pediatric transport team; SH, sending hospital.
Incidents reported by group. The results are expressed as absolute frequencies and percentages.
As regards follow-up at the RH, 32 patients (12.2%) required OTI within 72h of arrival, with no differences between groups (11.8% in the group of NIV initiated by the SH vs 12.5% in the group of NIV initiated by PTT; P=0.856). There were no deaths during the management of the patient by the PTT nor reported by the RH in the telephonic follow-up 3 days after transport.
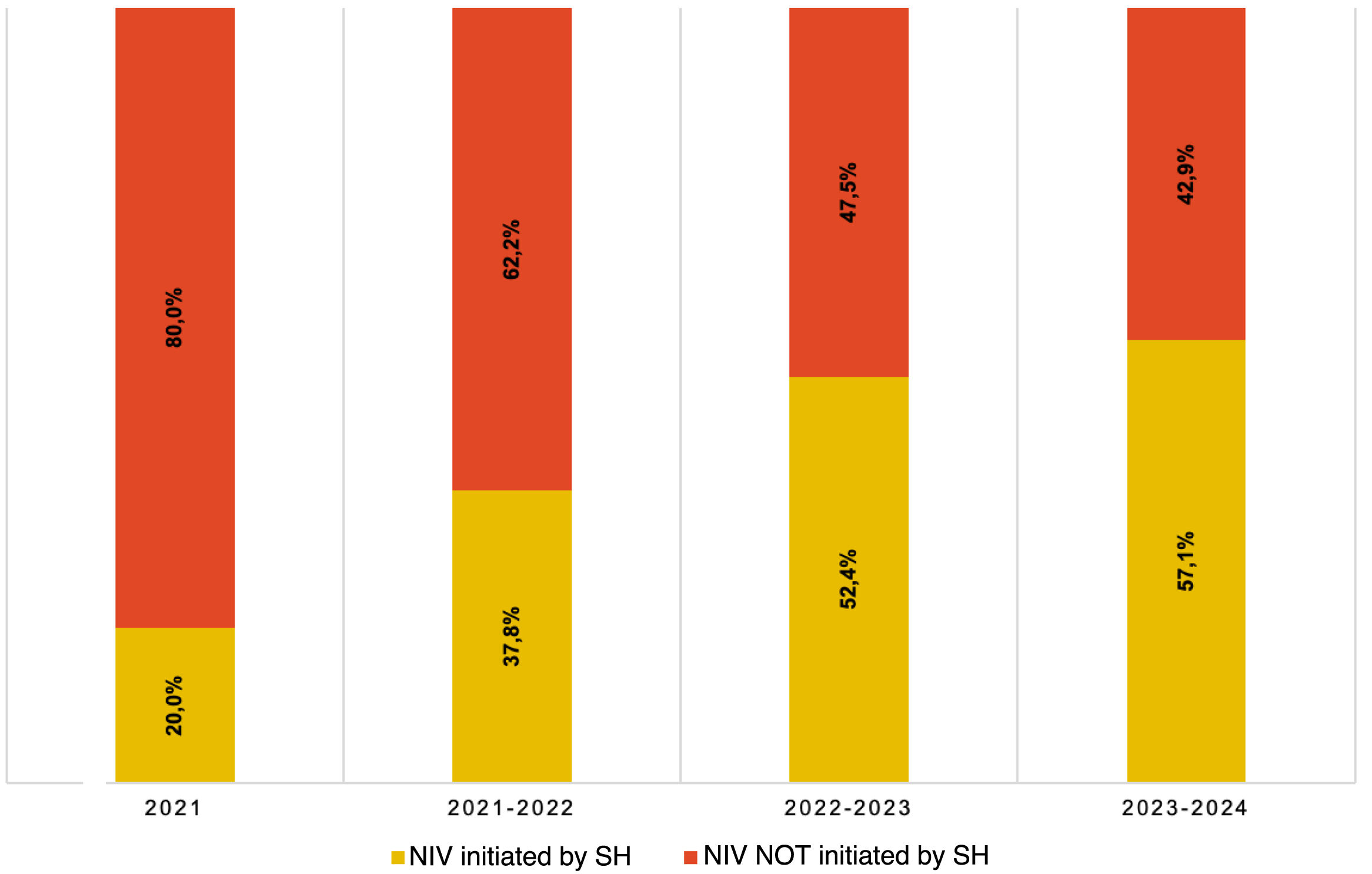
Fig. 4 reflects the progressive increase in the percentage of patients in whom NIV was initiated by the SH over the studied time intervals.
DiscussionThe findings of our study show that patients with a diagnosis of severe AB who required interhospital transport with NIV benefitted from early initiation of noninvasive respiratory support by staff at SHs. However, we also identified a potential increase in the frequency of minor NIV-related incidents in the group of patients in whom NIV had been initiated by the SH.
Noninvasive ventilation has been found to reduce severity scores and signs of respiratory distress, both in the PICU setting4,12 and in patient transport, as observed in the study conducted by Manso Ruiz de la Cuesta et al.7 Our study yielded similar results, and we also found that early initiation of NIV by the SH was associated with significantly lower severity scores, which were in the moderate as opposed to the severe range by the time of arrival of the PTT to the SH. We found a similar trend at the time of arrival to the RH, with P values that neared the threshold of significance, although the difference may not be clinically relevant, since both groups had scores in the moderate range. This could be due to the short time that the PTT is in contact with the patient, with a median duration of less than 90min, which may be too short to appreciate improvement by the end of transport.
Early initiation of NIV by the SH was also associated with lower oxygen requirements (FiO2), both during the management of the patient by the PTT at the SH and on arrival to the RH, which was consistent with previous studies in which NIV was found to reduce oxygen requirements from 2h of its initiation in patients with bronchiolitis13 and other diseases.14,15
The stabilization time in the group in which NIV was initiated by the PTT was similar to the one reported by Millán et al.,16 although their study did not take into account the specific timing of NIV initiation during the transport process. However, we ought to highlight that in our sample, initiation of NIV by the SH was associated with a shorter stabilization time.
In a previous study, Borrows et al.17 concluded that a longer stabilization time was not associated with poorer patient outcomes in the context of interhospital transport, which was consistent with our results, as there were no deaths nor any differences in the proportion of OTI between the two groups, and we also found that longer stabilization times were not associated with poorer outcomes in terms of mortality during transport or in the 3 subsequent days. Notwithstanding, we found a reduction in stabilization time, which, combined with the fact that patients in whom NIV was initiated earlier in the SH had lower FiO2 requirements and more favorable severity scores, was associated with a better clinical condition during transport and quicker arrival to the RH.
The use of NIV during pediatric ground transport has proven safe and feasible in several previous studies.15,16,18,19 This was also the case of our study, in which we only identified a single serious incident during the transport of patients with this support modality, independently of the timing of its initiation. Furthermore, none of the patients required escalation of respiratory support during transport.
The most frequent minor incidents in both groups were leaks and patient-ventilator asynchrony, in agreement with previous studies in adult patients.20,21 These adverse events were more frequent in patients in whom NIV had been initiated in the SH.
We also observed a substantial increase in the percentage of transports in which NIV had been initiated by the SH, from 20% to nearly 60% of pediatric transports over the 3-year period. This hints at a growing trend toward initiation of NIV while patients await transport. However, we ought to note that this procedure is not free of risks, especially when performed by professionals with less experience in the set up and use of these devices.
On the other hand, we found a reduction in the number of patient transports during the recent 2023–2024 epidemic season compared to previous periods. This decrease could be related to the administration of nirsevimab, a monoclonal antibody that has contributed to reducing hospital admissions due to AB caused by respiratory syncytial virus (RSV).22
All of the above, added to the findings of other studies in relation to NIV and patient transport,8,15,18 underscores the need for more in-depth training in the health care staff of these hospitals in order to minimize incidents an optimize the use of these devices. In addition, although we did not analyze its impact in this study, we want to highlight the role of the staff pediatrician in medical emergency coordination centers, who can offer telephonic telemedicine support to SHs, a practice that has proven useful in pediatric transport.23,24
To our knowledge, few published studies have analyzed the use of NIV in transport after its initiation by the staff of lower-level SHs (below tertiary care), so the findings of this study may be very relevant to clinical practice. We found that early initiation of NIV by the SH was associated with favorable outcomes without an associated increase in serious complications related to this respiratory support modality. We also found a reduction in the stabilization time, something that would allow quicker access to intensive care at the PICU while increasing the availability of pediatric transport units, which are a limited resource in high demand during epidemic seasons.
One of the limitations of our study is that it was conducted in a single center, which may limit the external validity of our findings, even if they are significant. This is compounded by the heterogeneity of PTTs in the rest of Spain and at the international level. There is also its retrospective design, which may limit the generalizability of the results, since there was a risk of selection bias and the sample of SHs was not homogeneous. Another limitation is that there were no data on the reasons why SHs did not initiate noninvasive respiratory support before transport (whether it was a lack of technological or human resources or a lack of knowledge on the use of NIV systems), which could be another source of bias.
In the future, it would be useful to conduct studies with a prospective multicenter design and in other geographical areas to determine whether the findings of the study can be generalized.
ConclusionIn our study of patients with AB who required interhospital transport with NIV, we observed an association between early initiation of noninvasive respiratory support and better clinical condition during transport, a finding that can help optimize the use of pediatric transport team resources. Training of the staff of SHs in the use of NIV could reduce the incidence of complications and guarantee the benefits associated to this modality.
FundingThis research project did not receive specific financial support from funding agencies in the public, private or not-for-profit sectors.
Previous meeting: this study was presented as a long oral communication at the 28th Annual Meeting of the Societat Catalana de Pediatría, June 14–15, 2024, Girona.