The aims of our study were to assess the effectiveness and safety of continuous positive airway pressure (CPAP) during the transport of infants with acute respiratory failure (ARF) and to compare the disease course and clinical outcomes of CPAP vs oxygen therapy in the PICU setting.
Materials and methodsWe conducted a retrospective observational and analytical study by reviewing the health records of infants with ARF aged 0–12 months that required interhospital transfer to the PICU.
ResultsWe included 110 patients: 71 transported with CPAP and 39 with oxygen therapy. The main cause of ARF was acute bronchiolitis (81.8%). The median level of CPAP was 7 cmH2O (interquartile range, 6–7). Controlling for the values prior to transfer in the specific multivariate models, we found that CPAP achieved a significant decrease in the Wood-Downes score (β = –1.08; 95% CI = –1.76 to –0.40; P = .002) and the heart rate ( β = –19.64; 95% CI = –28.46 to –10.81; P < .001). No patients required endotracheal intubation during transport. During the PICU stay, the intubation rate was similar in the CPAP group (7%) and the oxygen therapy group (5.1%) (P = .689). The proportion of patients that required bilevel positive airway pressure within 6 h of admission to the PICU was higher in the oxygen therapy group: 100% (11/11) vs 69.2% (18/26), P = .04.
ConclusionsEarly administration of CPAP to infants with ARF was a safe respiratory support intervention during interhospital transport. During patient transport, the use of CPAP achieved greater decreases in the Wood-Downes score and heart rate compared to oxygen therapy.
Evaluar la efectividad y seguridad de la presión continua en la vía aérea (CPAP) en lactantes trasladados por insuficiencia respiratoria aguda (IRA) y comparar el curso clínico y la evolución en la unidad de cuidados intensivos pediátricos (UCIP) de los pacientes trasladados con dicha terapia vs la oxigenoterapia convencional.
Material y métodosEstudio observacional y analítico de una cohorte retrospectiva. Se revisaron las historias de los lactantes de 0 a 12 meses con IRA que precisaron traslado interhospitalario a la UCIP.
ResultadosSe incluyeron 110 pacientes: 71 trasladados con CPAP y 39 con oxigenoterapia. La causa principal de IRA fue la bronquiolitis (81,8%). La mediana del nivel de CPAP fue 7 cmH2O (rango intercuartílico, 6-7). Controlando en análisis multivariables específicos por los valores previos, se obtuvo que la CPAP durante el traslado produjo una disminución significativa en el score de Wood-Downes (beta = -1,08; IC 95% = -1,76 - 0,40; p = 0,002 y en la frecuencia cardiaca beta = -19,64, IC 95% = - 28,46 – -10,81; p < 0,001. Ningún pacientes precisó intubación endotraqueal durante el transporte. En la UCIP, la tasa de intubación fue similar en el grupo CPAP 7% y en el de oxigenoterapia 5,1% p = 0,689. El porcentaje de pacientes que precisaron ventilación no invasiva con dos niveles de presión en las primeras 6 horas de ingreso en UCIP fue mayor en el grupo oxigenoterapia: 100% (11/11) vs 69,2% (18/26), p = 0,04.
ConclusionesLa administración precoz de CPAP en lactantes es segura durante el traslado interhospitalario. Durante el transporte, la CPAP comparada con la oxigenoterapia disminuye el score de Wood-Downes y la frecuencia cardiaca.
Paediatric transport involves delivering care to patients who require transfer to a health care facility that can provide definitive treatment. Interhospital ground transport can increase the risk associated with the patient’s current disease. Critical events can occur in up to 15% of paediatric transports.1
The safety of paediatric transport by ground ambulance varies between emergency medical services systems. It is essential to ensure the stability of the patient before transport, given the difficulty of performing procedures in transit in the ambulance setting.2 In addition, the transport of patients aged less than 1 year is further complicated due to their higher risk of instability and the narrow range of equipment and supplies available for this population.3,4
Acute respiratory failure (ARF) is a major cause of morbidity and mortality in the paediatric age group and is one of the leading causes of admission to paediatric intensive care units (PICUs). It is also a common reason for transport to tertiary health care facilities.2,3,5
Non-invasive ventilation (NIV) has emerged as a powerful tool for the emergency management of ARF in paediatric transport. A restrictive protocol, with careful selection to exclude patients with moderate to severe acute respiratory distress syndrome (ARDS), and a well-trained retrieval team are essential for correct use of NIV during transport.6 There are several studies in the literature of the use of NIV during patient transport, but none comparing different modes of ventilatory support during transport. The aim of our study was to compare the use of continuous positive airway pressure (CPAP) versus oxygen therapy during transport of infants with ARF and their disease course and outcome in the PICU.
MethodsThe study was approved by the Clinical Research Ethics Committee of the Health Care Area of the main hospital in the study.
Study designWe conducted an observational and analytical retrospective cohort study comparing the use of CPAP versus oxygen therapy in transported infants with ARF.
SampleObtained by consecutive sampling between January 2006 and December 2015. We included all patients aged 0–12 months with ARF that required interhospital ground transport to the PICU. The criteria used to define ARF were:
- •
Clinical criteria: symptoms and signs of respiratory distress (moderate or severe dyspnoea, increased respiratory rate, use of accessory respiratory muscles , paradoxical breathing and/or apnoea).
- •
Blood gases criteria: hypercapnia or hypoxaemia (transcutaneous oxygen saturation <94% and inspiratory fraction of oxygen [FiO2] > 0.4).
We excluded patients with contraindications for NIV,7 with neonatal diseases (hyaline membrane disease, transient tachypnoea, meconium aspiration syndrome and apnoea of prematurity) transported to the PICU without respiratory support.
The infants were transferred from 2 first-level hospitals to the PICUs of 2 tertiary care referral hospitals. Table 1 shows the differences in the distance and duration of transport between hospitals and the type of respiratory support used during transport. The level of respiratory support given to the infant was not decreased prior to transfer. During the first period of the study, oxygen therapy was the mode of respiratory support used routinely, which changed to CPAP once the necessary resources became available. Before the introduction of NIV, the paediatricians responsible for stabilising patients received accredited training in this technique and then delivered courses to the nursing staff and non-specialist retrieval teams.
Differences in distance, transport time and respiratory support between hospitals.
| Health care area 1 | Health care area 2 | |
|---|---|---|
| Distance (km) | 28 | 80 |
| Approximate transport time (minutes) | 30 | 75 |
| Oxygen therapy | January 2006–November 2013 (29 patients) | December 2007–November 2011 (10 patients) |
| CPAP | November 2013–December 2015 (39 patients) | November 2011–December 2015 (32 patients) |
We collected data retrospectively through the review of health records, and analysed it using the software SPSS version 20.0.
The primary outcome was the reduction in the severity of respiratory failure, assessed by means of the modified Wood-Downes score.8 We collected data on the following variables for each patient: sex, age, underlying disease, referring hospital, length of stay at the referring hospital before transfer, main diagnosis, use of respiratory support, sedation and nasogastric tube during transport, and the pressure setting of CPAP. In addition, we collected data on clinical and blood gas parameters, transcutaneous oxygen saturation, FiO2 and the SF ratio (oxygen saturation measured by pulse oximetry [SpO2]/FiO2) before transport and arrival to the PICU. We estimated the FiO2 delivered with nasal prongs and oxygen masks by extrapolating data from studies conducted in adults.9,10 We excluded transcutaneous oxygen saturation values higher than 97% in the calculation of the SF ratio.11 We collected data on the following variables related to the PICU stay: highest level of respiratory support given to patients, duration of mechanical ventilation (MV) (invasive and non-invasive) and length of stay in the PICU. We defined pneumonia as the presence of fever and/or respiratory symptoms with evidence of parenchymal infiltrates on the chest radiograph.12
MaterialsThe only mode of NIV used during transport was CPAP, delivered with the following equipment:
- •
Ventilators: Boussignac® (Vygon, Écouen, France), Oxylog 3000 plus® (Dräger, Germany), Elisée 150® (ResMed, Australia) and Vivo 40® (Breas, Sweden).
- •
Helmets were the only interface used: in patients from 3 to 5 kg, DimAir Neo® (Dimar, Italy); and from 5 to 15 kg, the DimAirPed® or the CaStarInfant-high® (Starmed, Mirandola, Italy).
- •
Conventional oxygen therapy: nasal prongs, oxygen masks and Venturi masks.
We calculated absolute and relative frequencies to describe categorical variables. To summarise continuous variables, we performed the Kolmogorov-Smirnov test to assess the assumption of normality and based on the results calculated either the mean and standard deviation (SD) or the median and the interquartile range.
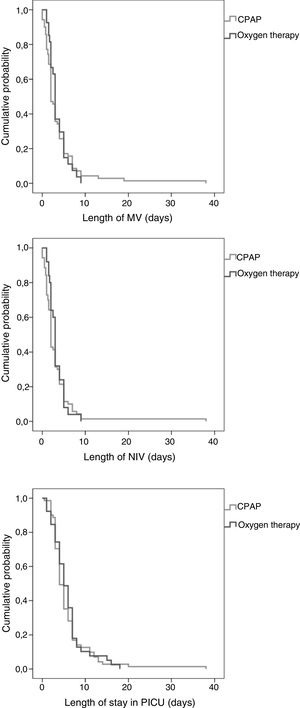
In the univariate analysis, we used the chi square test and the Fisher exact test to compare qualitative data, while for quantitative data we used the independent samples t test or Mann-Whitney U test to compare means and the ANOVA or the Kruskal-Wallis H test. We analysed the length of stay and the duration of MV by the Kaplan-Meier method and differences in this variables using the log-rank test.
In the multivariate analysis, we used the R software to fit linear regression models with the GLM procedure, checking that residuals following a normal distribution, and selecting the definitive model with the Aikaike information criterion (AIC). We calculated 95% confidence intervals for all tests, and considered p-values of less than 0.05 statistically significant.
For the purpose of sample size calculation, we considered a 2-point reduction in the Wood-Downes score clinically relevant.13–15 Assuming a ratio of sample sizes of 1 and equal variances, a SD of 2 points in the Wood-Downes score distribution and a non-response rate of 3% in each group, we calculated that we needed a rounded sample of 40 patients for a 5% probability of type 1 error (a confidence level of 95%) and a 20% probability of type 2 error (a power of 80%).
ResultsIn the 10 years under study, the total number of transported patients that met the inclusion criteria was 110:71 transported with CPAP and 39 with oxygen therapy. Table 2 compares the characteristics of these groups. Prematurity was the most frequent underlying condition (61.8%), and bronchiolitis the most frequent cause of ARF (81.8%). We found a difference in the proportion of patients that had bronchiolitis or wheezing episodes between the CPAP and the oxygen therapy groups (P = .02).
Comparison of demographic characteristics of CPAP group and oxygen therapy group.
| Total (n = 110) | CPAP (n = 71) | Oxygen therapy (n = 39) | P | |
|---|---|---|---|---|
| Sex n, (%) | ||||
| Male | 67 (60.9%) | 39 (54.9%) | 28 (71.8%) | .083 |
| Female | 43 (39.1%) | 32 (45.1%) | 11 (28.2%) | |
| Age (months) Median (interquartile range) | 2.6 (1.4–6.3) | 2.8 (1.4–7.9) | 2.5 (1.5–4.9) | .425 |
| Weight (kg) (Mean ± SD) | 5.8 ± 1.9 | 5.8 ± 1.9 | 5.8 ± 1.9 | .963 |
| Length of stay at the referral hospital before transfer (days) Median (interquartile range) | 1 (0–2) | 1 (0–2) | 0 (0–2) | .380 |
| Underlying disease n, (%) | ||||
| No | 76 (69.1%) | 48 (67.6%) | 28 (71.8%) | .649 |
| Yes | 34 (30.9%) | 23 (32.4%) | 11 (28.2%) | |
| Type of underlying disease n, (%) | (n = 34) | (n = 23) | (n = 11) | |
| Prematurity | 21 (61.8%) | 12 (52.2%) | 9 (81.8%) | .203 |
| Cardiac disease | 6 (17.6%) | 5 (21.8%) | 1 (9.1%) | |
| Wheezing episode | 4 (11.8%) | 4 (17.4%) | 0 (0%) | |
| Malformations | 2 (5.9%) | 1 (4.3%) | 1 (9.1%) | |
| SGA | 1 (2.9%) | 1 (4.3%) | 0 (0%) | |
| Diagnosis n, (%) | ||||
| Bronchiolitis | 90 (81.8%) | 54 (76.1%) | 36 (92.3%) | .020 |
| Wheezing episode | 15 (13.6%) | 14 (19.7%) | 1 (2.6%) | |
| Pneumonia | 5 (4.5%) | 3 (4.2%) | 2 (5.1%) | |
| Apnoea n, (%) | ||||
| No | 89 (80.9%) | 55 (77.5%) | 34 (87.2%) | .215 |
| Yes | 21 (19.1%) | 16 (22.5%) | 5 (12.8%) |
CPAP, continuous positive airway pressure; SD, standard deviation; SGA, small for gestational age.
The p-values refer to the comparison of the CPAP and oxygen therapy groups.
In the CPAP group, the system used for delivery of CPAP during transport was the Boussignac® in 67.6% of patients (n = 48), the Oxylog 3000 plus® in 22.5% (n = 16), the Vivo 40® in 8.5% (n = 6) and the Elisée 150® in 1.4% (n = 1). The median pressure of CPAP was 7 cmH2O (interquartile range, 6–7 cmH2O). Only two infants in the CPAP group needed sedation to facilitate the adaptation to respiratory support, for which they were given midazolam. The use of nasogastric tubes was more frequent in the CPAP group compared to the oxygen therapy group (80.3% vs 2.6%; P < .001).
Fig. 1 and Table 3 show the differences found in the univariate analysis of the clinical and blood gas variables measured before transfer and on arrival to the PICU by type of respiratory support used during transport. The SF ratio was calculated at the referring hospital in 66.4% of patients (n = 73), but only in 41.8% (n = 46) at the PICU. Blood gas tests were performed in 87.3% of patients (n = 96) at the referring hospital, compared to 53.1% (n = 59) in the PICU.
Univariate comparison of differences in clinical and blood gas variables between the CPAP and oxygen therapy groups.
| Variables | Before transfer | PICU | ||||
|---|---|---|---|---|---|---|
| CPAP | Oxygen therapy | P | CPAP | Oxygen therapy | P | |
| Wood-Downes score | 8.2 ± 2.3 | 7.3 ± 1.4 | .023 | 5.4 ± 1.7 | 6.2 ± 1.8 | .034 |
| HR (beats/min) | 165.2 ± 21.3 | 156.1 ± 24.6 | .044 | 151.5 ± 24.8 | 169.9 ± 20.7 | <.001 |
| RR (breaths/min) | 59.8 ± 13.8 | 62.9 ± 13.2 | .264 | 47.8 ± 12.9 | 52.8 ± 14.9 | .068 |
| SaO2 (%) | 94 (IQR, 90–98) | 97 (IQR, 95–99) | .06 | 98 (IQR, 96–100) | 97.5 (IQR, 94.75–100) | .827 |
| FiO2 | 0.25 (IQR, 0.21-0.45) | 0.5 (IQR, 0.28-0.8) | <.001 | 0.32 (IQR, 0.26-0.4) | 0.28 (IQR, 0.27–0.5) | .896 |
| SF | 322.4 ± 109.3 | 251.6 ± 100.7 | .014 | 300.6 ± 93.9 | 266.8 ± 113.2 | .277 |
| pCO2 (mmHg) | 49.4 ± 14.5 | 52.2 ± 11.53 | .345 | 48.9 ± 15.4 | 56.3 ± 15.7 | .078 |
FiO2, fraction of inspired oxygen; HR, heart rate; pCO2, partial pressure of carbon dioxide; PICU, Paediatric intensive care unit; RR, respiratory rate; SaO2, transcutaneous oxygen saturation; SF, (saturation measured via pulse oximetry/ FiO2).
The p-values refer to the comparison of the CPAP and oxygen therapy groups.
The specific multivariate models, which included the mode of respiratory support used during transport (CPAP vs oxygen therapy), clinical parameters, the partial pressure of carbon dioxide (pCO2), FiO2 and SF ratio in the PICU (controlled for their values prior to transfer), showed that CPAP only achieved significant decreases in the Wood-Downes score (β = –1.08; 95% CI = –1.76 to – 0.40; P = .002) and the heart rate (β = –19.64; 95% CI = –28.46 to –10.81; P < .001).
None of the patients required a change in the mode of respiratory support or endotracheal intubation during interhospital transport. Table 4 compares PICU outcomes by mode of support, and Fig. 2 presents the Kaplan–Meier curves of the duration of MV and length of stay in PICU. In our sample, the early use of CPAP prior to transfer was associated with a similar intubation rate (7.1% vs 5.1%; P = .689). However, the need for invasive MV and for BiPAP within 6 h of admission to the PICU were lower in the CPAP group: 40 % vs 100% (P = .092) and 69.2% vs 100% (P = .04), respectively. In our study, the mortality was limited to 1 patient in the oxygen therapy group that required invasive MV and died as a result of the underlying disease, a polymalformative syndrome.
Comparison of outcomes in PICU between the CPAP and oxygen therapy groups.
| Total | CPAP | Oxygen therapy | P | |
|---|---|---|---|---|
| Maximum respiratory support at PICU n, (%) | ||||
| Oxygen therapy | 12 (10.9%) | 0 (0%) | 12 (30.8%) | <.001 |
| HFNC | 1 (0.9%) | 1 (1.4%) | 0 (0%) | |
| CPAP | 53 (48.2%) | 39 (54.9%) | 14 (35.9%) | |
| BiPAP | 37 (33.6%) | 26 (36.6%) | 11 (28.2%) | |
| Invasive MV | 7 (6.4%) | 5 (7.1%) | 2 (5.1%) | |
| Log Rank test | ||||
| Length of MV (days) Median (interquartile range) | 3 (1.5–5) | 2 (2–3) | 3 (2–4) | .575 |
| Length of NIV (days) Median (interquartile range) | 2 (1,5-4) | 2 (2–3) | 3 (2–3) | .558 |
| Length of stay in PICU (days) Median (interquartile range) | 5 (3–7) | 4 (4–5) | 5 (4–6) | .727 |
BiPAP, bilevel positive airway pressure; CPAP, continuous positive airway pressure; HFNC, High flow nasal cannula; MV, mechanical ventilation (invasive or non-invasive); NIV, non-invasive ventilation.
The p-values refer to the comparison of the CPAP and oxygen therapy groups.
The causes of ARF in our sample were similar to those reported in other studies conducted in patients admitted to the PICU that required support with NIV and invasive MV.6,16 We ought to highlight a higher proportion of patients with bronchiolitis in our study, a difference that could be explained by the age of less than 1 year in our sample.17
The proportion of patients with underlying disease in the cohort (30.9%) was lower compared to other samples of patients requiring NIV in the PICU setting described in the literature: 43% (Abadesso et al.)16 and 61% (Mayordomo-Colunga et al.).18 Prematurity was the most frequent underlying condition, and its frequency was similar compared to other case series of patients with bronchiolitis requiring admission to the PICU.17,19
Initially, the use of NIV in paediatric patients was restricted to units with extensively trained staff, but in recent years it has begun to be used in settings with fewer resources for monitoring, such as in interhospital transport.6,20,21 In our case series, the helmet interface had been chosen based on published evidence on its use in infants with ARF,22–24 in addition to being more comfortable25 and easy adaption.
The mode of ventilation used in our case series was CPAP. This NIV mode is indicated for initiation of ventilatory support in infants aged less than 3 months and in patients with bronchiolitis or apnoea.26 These complaints were frequent reasons for interhospital transport in our sample. Continuous positive airway pressure is widely used because it is not as technically challenging as bilevel positive airway pressure (BiPAP) when it comes to achieving patient-ventilator synchrony. In our study, pressure delivered with CPAP was 7 cmH2O, in agreement with previous works.20,27 We ought to highlight that in patients with bronchiolitis and hypercapnic respiratory failure, a CPAP pressure of 7 cmH2O is associated with an improvement in respiratory effort and better short-term outcomes.
Evidence from multiple studies shows that the use of NIV achieves an improvement in the Wood-Downes score.14,15 Milési et al. reported a greater decrease in the m-WCAS score with the use of CPAP versus conventional oxygen therapy in infants with bronchiolitis admitted to the PICU (–2.4 ± 1.05 vs –0.5 ± 1.3; P = .03).13 In addition to a reduction in the severity score, our study found an improvement in heart rate and a decrease in the respiratory rate in the PICU when NIV was used for respiratory support during transport. Several studies comparing NIV with oxygen therapy in paediatric patients in the PICU have described improvements in clinical parameters.28,29 In a study of infants with bronchiolitis that required CPAP during transport, Fleming et al. found a lower FiO2 on arrival to PICU (0.62 vs 0.4; P < .001).20 We did not observe this trend. In a comparison of CPAP with standard treatment in patients with bronchiolitis, Thia et al. observed a greater improvement in pCO2 in the CPAP group (–1.35 vs –0.53 kPa; P < .01).30 This result was less clear in our study, possibly due to the shorter time of observation.
In our study, none of the patients required intubation during transport, which was consistent with the findings of other authors, with a reported incidence of intubation of 0%–1%.6,20,21 In our sample, 6.4% of the patients were eventually treated with invasive MV, but the rate reported in the literature in patients initially treated with NIV is of 20%–22%.6,16 This difference may be explained by the use of BiPAP in our sample, as it has been reported that the use of BiPAP reduces the intubation rate to 8%.31 In our study, BiPAP was used in 33.6% of patients. Several studies have demonstrated a reduction of intubation rates, need of MV and incidence of complications with use of NIV.29,32 The need for MV or BiPAP within 6 first hours of admission to the PICU was lower in the CPAP group. These differences could be related to the early improvement achieved with CPAP, although the outcomes of patients in the PICU cannot be attributed to this factor alone. The fact that 30.8% of patients receiving support with oxygen therapy during transport continue with this mode of support in the PICU may be due to the lower availability and development of NIV in the early years following the introduction of this technique in the PICUs of the health care areas included in the study.
The mortality of patients with ARF admitted to the PICU reported in the literature ranges between 1.3% and 1.6%,16,17 which is comparable to the mortality found in our study (0.7%).
There are several limitations to our study. One is its retrospective design. Another is the amount of missing data, which was greatest for the SF ratio, followed by blood gas parameters. The groups compared were not homogeneous. In addition, the period under study was long (10 years), and during this time there were changes in clinical protocols and improvements in the equipment used to deliver NIV. These changes may have been a source of bias in our results.
We did not analyse the FiO2 delivered during transport because most ventilators used for NIV can only provide a limited range of FiO2. It is important to be aware that this limiting factor could indirectly influence in clinical and blood gas parameters in the PICU as well as in patient outcomes.
Our study included patients referred from 2 first-level hospitals. There was variation between the corresponding health care areas as regards the material resources used and the duration of transport to the PICU. The differences in the theoretical knowledge and practical skills of the different health care teams were minimal. All interventions conformed to standardised protocols and the training offered by the Respiratory Work Group of the Sociedad Española de Cuidados Intensivos Pediátricos (Spanish Society of Paediatric Intensive Care). We believe that the results of the study are independent of the health care area and thus could be extrapolated to other areas in Spain.
Prospective multicentre studies are needed to overcome the limitations of our study.
ConclusionsEarly delivery of CPAP to infants with ARF was a safe measure of respiratory support during interhospital transport. In this framework, the use of CPAP was associated with an improvements in the modified Wood-Downes score and the heart rate compared to oxygen therapy.
Conflict of interestThe authors declare no conflicts of interest.
Please cite this article as: Manso Ruiz de la Cuesta R, del Villar Guerra P, Medina Villanueva A, Modesto Alaport V, Molinos Norniella C, Bartolomé Albistegui MJ, et al. CPAP vs oxigenoterapia convencional en lactantes trasladados por insuficiencia respiratoria. An Pediatr (Barc). 2020;93:152–160.