In developed countries, acute bronchiolitis (AB) is the most frequent reason for hospital admission in infants aged less than 1 year. Between 3% and 11% of the infants hospitalised with AB are transferred to the paediatric intensive care unit (PICU). The management of AB is based on supportive care, and in patients with moderate-to-severe AB, non-invasive ventilation (NIV) has become the first choice of respiratory support.1 This is a technique whose use is generally restricted to PICUs, which, due to the seasonal pattern of AB, get overwhelmed during incidence peaks. Due to the need to find alternative solutions during the epidemic season, we started to use NIV in patients with moderate AB at the ward level, with the option to transfer them to a PICU if necessary, an approach that was already being practised in some European hospitals.2,3 In this article, we describe our experience with this strategy and the observed clinical outcomes.
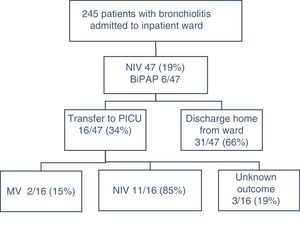
We conducted the study in a secondary care level hospital in the Community of Madrid. Of a total of 245 infants aged less than 6 months admitted with a diagnosis of AB between January 2013 and March 31 of 2017, 47 (19%) received NIV (Fig. 1). Our hospital does not have a PICU, and the nearest PICU is 15min away by ambulance. We set up an area in the paediatric ward that included 2 beds (of the total of 18 available) that could be seen fully through a glass panel and accessed quickly, equipped for comprehensive monitoring (heart rate, respiratory rate, oxygen saturation [SatO2]) and with air and oxygen outlets and the necessary equipment for intubation and invasive mechanical ventilation (IMV). The nursing staffing in the ward was as follows: 3 nurses/2 nurse assistants in the morning and evening shifts, and 2 nurses/1 nurse assistant in the night shift. Staffing was not increased for the purpose of the study. After a period of 6 months during which the protocol was developed and all doctors, nurses and aides were trained in it, we introduced the use of NIV in patients with AB in January 2013. Patients with hypoxaemia (SatO2 <90% with the ambient oxygen concentration) and mild respiratory distress (Respiratory Distress Assessment Instrument [RDAI] ≤5 or the Wood-Downes score modified by Ferres [mWDS] ≤3, depending on the physician in charge) received high-flow oxygen therapy (HFOT). The term non-invasive ventilation includes nCPAP (nasal continuous positive airway pressure) with a single level of air pressure and BiPAP (bilevel positive airway pressure) with two level pressures. The use of NIV was indicated in infants aged less than 3 months (limit imposed by the available material resources) with a diagnosis of AB presenting with hypercapnia (capillary PCO2≥60mmHg) and/or apnoea and/or moderate to severe respiratory distress (RDAI, 6–7; mWDS, 4–7). We excluded patients with underlying respiratory disease or altered level of consciousness. Table 1 summarises epidemiological and respiratory data. All patients tolerated NIV well, and none developed complications.
Epidemiological data and NIV settings used in the sample.
| Epidemiologic data | N=47 |
|---|---|
| Male sex (%) | 21 (44.7) |
| Birth <37 weeks (%) | 11 (23.4) |
| Median age in days (p25–p75) | 33 (18–51) |
| Aetiological agent (%) | |
| RSV | 28 (59.6) |
| Other | 19 (40.4) |
| HFOT (%) | 17 (34) |
| Days elapsed from onset of NIV (mean, 95% CI) | 4.5 (3.6–5.4) |
| Indication for NIV (%) | |
| Hypercapnia | 17 (36.2) |
| Respiratory distress | 8 (17) |
| Hypercapnia+distress | 19 (40.4) |
| Apnoea | 3 (6.4) |
| BiPAP (%) | 6 (36.2) |
| Duration of NIV (%) | |
| <24h | 13 (27.7) |
| 24–36h | 5 (10.6) |
| 36–48h | 10 (21.3) |
| >48h | 19 (40.4) |
| Length of stay (mean, 95% CI) | 5.9 (4.7–7.13) |
| Transfers to PICU (%) | 16 (34) |
| Reason for transfer (%) | |
| Hypercapnia | 9 (56) |
| Respiratory distress | 4 (25) |
| Hypercapnia+distress | 1 (6.2) |
| Apnoea | 1 (6.2) |
| Other | 1 (6.2) |
| NIV settings (mean, 95% CI) | |
| Max flow rate (L/min) | 8.86 (8.5–9.31) |
| Max PEEP (cmH2O) | 6.11 (5.57–6.3) |
| Max FiO2 (%) | 32.5 (27.9–38.1) |
| Max PCO2 (mmHg) | 59.2 (56.4–62.4) |
BiPAP, bilevel positive airway pressure; FiO2, fraction of inspired oxygen; HFOT, high-flow oxygen therapy; IMV, invasive mechanical ventilation; NIV, non-invasive mechanical ventilation; PEEP: positive end-expiratory pressure; PICU, paediatric intensive care unit; RSV, respiratory syncytial virus.
In the management of moderate to severe AB, respiratory support starts with administration of HFOT with warmed and humidified oxygen and can be escalated to NIV and then IMV. It is believed that both NIV and HFOT can improve work of breathing and oxygenation. The magnitude of these effects varies widely between studies, and the current evidence in this regard is weak.4 In recent years, HFOT has emerged as an alternative to NIV for respiratory support that is perceived as being easier to implement. Its use at the ward level has been proposed in patients with moderate to severe AB that meet the criteria for initiation of NIV, and there have been positive reports of its effectiveness in preventing the use of more aggressive modalities.5 In the same way that this application of HFOT is considered useful, we believe that patients could benefit from NIV, which is both safe and efficacious, without in and of itself requiring admission to the PICU. The possibility of administering NIV at an early stage offers an added clinical benefit, as it may prevent progression of disease, thus reducing the mean length of stay of these patients.6 We ought to note that the degree to which this technique was available in our hospital allowed a greater flexibility in its use, which may have contributed to NIV being prescribed in a greater proportion of the total admitted patients (19%) compared to other case series,3 which in turn would have contributed to reducing the number of transfers.
The delivery of NIV in the inpatient ward is a feasible option that could help alleviate the problems that emerge every year during the AB season. The elements that we consider essential for its implementation are adequate training of the staff, the establishment of specific care protocols and the capacity to provide a safe environment and adequate care in case of clinical worsening until patients can be transferred to a PICU.
Please cite this article as: Paredes González E, Bueno Campaña M, Salomón Moreno B, Rupérez Lucas M, de la Morena Martínez R. Non-invasive ventilation in acute bronchiolitis on the ward. A viable option. An Pediatr (Barc). 2019;90:119–121.