Self-poisoning with suicidal intent accounts for 4.9% to 23.2% of poisoning cases managed in paediatric emergency departments in Europe.1 It frequently involves multiple drugs, and in many instances it is not known which. The mainstay of management in these patients is stabilization, monitoring and supportive care, and it is essential to seek signs that may help identify the culprit substances to try to prevent potential toxicity.
Metabolic lactic acidosis usually develops in severely ill patients, and it is a marker of tissue hypoxia and an independent predictor of mortality.2 In patients with poisoning, hyperlactatemia is also associated with poorer outcomes, although in most cases it is due to a direct toxic mechanism and may develop in patients that are clinically stable as an early marker of toxicity.2,3 The management of lactic acidosis in the context of poisoning differs from its management in severely ill patients without poisoning. In the latter, management is based on respiratory and haemodynamic stabilization, while in poisoned patients it may be necessary to use some form of renal replacement therapy.3
We present the cases of 3 paediatric patients with metabolic lactic acidosis secondary to self-poisoning with suicidal intent (Tables 1 and 2). All patients were managed with monitoring of blood gases and administration of bicarbonate and fluids, to which they responded favourably. Two patients required admission to the paediatric intensive care unit (PICU) due to renal insufficiency or depressed level of consciousness. The toxicology analyses identified the cause of the acidosis. The management included filing of a legal report and consultation with the psychiatry team.
Clinical summary of the cases.
| Case | Sex | Age (years) | Reported/suspected substances | Evaluation on arrival to PED | Treatment | Outcome | |||
|---|---|---|---|---|---|---|---|---|---|
| Hours elapse from exposure | PT | PE | VS | ||||||
| 1 | F | 15 | Metformin (42.5g) | 3 | Stable | Normal | Normal | Bicarbonate Glucose Fluid restriction Furosemide | RI and oliguria PICU admission Favourable outcome |
| 2 | F | 14 | Unknown | 1 | Unstable | GCS 9, response to painful stimuli, general pallor | Normal | Oxygen therapy. MV. Fluid therapy GL y AC. Bicarbonate | PICU admission Favourable outcome |
| 3 | M | 16 | Omeprazole, ibuprofen, prednisone, diazepam, metformin, paracetamol, robaxisal, tramadol, venlafaxine, valsartan | 3 | Stable | Malaise (dizziness, nausea) | Tachypnoea (RR 24×′) | Fluid therapy Bicarbonate. Furosemide | RI, oliguria and proteinuria. Favourable outcome |
AC, activated charcoal; F, female; GCS, Glasgow Coma Score; GL, gastric lavage; M, male; MV, mechanical ventilation; PE, physical examination; PICU, paediatric intensive care unit; PT, paediatrics triage; RI, renal insufficiency; RR, respiratory rate; VS, vital signs.
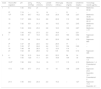
Summary of blood and toxicology tests.
| Case | Hours after ingestion | pH | pCO2 (mmHg) | HCO3− (mmol/L) | Lactate (mmol/L) | Anion gap (mEq/L) | Glucose (mg/dL) | Creatinine (mg/dL) | Toxicology results (μg/mL) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 4 | 7.30 | 44.2 | 21 | 4.1 | – | 104 | 1.22 | Metformin: 69.52 |
| 9a | 7.19 | – | 14 | 14 | – | 31 | – | – | |
| 13b | 7.30 | 30.7 | 16.2 | 12.9 | 25.9 | 128 | 2.07 | Metformin: 45.94 | |
| 16 | 7.37 | 28.8 | 16.4 | 8.8 | 22.8 | 110 | 1.95 | Metformin: 28.12 | |
| 18 | 7.42 | 33.1 | 21.3 | 4.4 | 19.2 | 121 | 2.45 | Metformin: 23.43 | |
| 21 | 7.45 | 33.9 | 23.3 | 2.8 | 18.5 | 103 | 2.87 | Metformin: 1.77 | |
| 30 | 7.43 | 42.2 | 27.5 | 2.3 | 16.6 | – | 2.51 | – | |
| 2 | 1 | 7.28 | 41 | 19.3 | 5.3 | 22.0 | 183 | 0.82 | Naproxen: 983 |
| 2b | 7.34 | 36 | 19.4 | 4.0 | 20.6 | 199 | 0.70 | Naproxen: 885 | |
| 3b | 7.37 | 38 | 22.0 | 5.3 | 28.5 | 77 | – | – | |
| 9 | 7.43 | 37 | 24.6 | 4.4 | 18.1 | 124 | 0.69 | – | |
| 16 | 7.48 | 38 | 28.3 | 1.2 | 10.0 | 114 | – | ||
| 21 | 7.52 | 35 | 28.6 | 1.2 | 9.9 | 104 | 0.72 | Naproxen: 395 | |
| 3 | 4 | 7.38 | 31.5 | 18.4 | 6.3 | 22.5 | 94 | 1.4 | |
| 10 | 7.55 | 12.8 | 11.1 | 3.4 | 18.8 | 104 | 1.8 | Metformin: 1.5 | |
| 13.5b | 7.38 | 33.2 | 19.4 | 1.9 | 17.7 | 115 | 2.15 | Metformin: 1.4 Paracetamol: 4.1 | |
| 17.5 | 7.38 | 37.7 | 21.6 | 1.9 | 18 | 108 | 2.09 | Naproxen: 23.6 Ibuprofen: 14.1 Paracetamol: 2 | |
| 27.5 | 7.45 | 34.3 | 23.4 | 2.3 | 15.2 | – | 1.27 | Naproxen: 17.2 Ibuprofen: 4.1 |
Normal ranges: pH, 7.35–7.45; anion gap, 8–16mEq/L; glucose, 70–110mg/dL; HCO3−, 23–39mmol/L; lactate, 0.5–2.2mmol/L. Therapeutic ranges: metformin, 1–2μg/mL; naproxen, 25–75μg/mL; ibuprofen, 15–30μg/mL; paracetamol, 10–20μg/mL.
Metabolic lactic acidosis can develop in the context of poisoning by metformin, nonsteroidal anti-inflammatory drugs (NSAIDs), salicylates, valproate, isoniazid, propofol or propylene glycol, among other substances, in both paediatric and adult patients.3
Metformin-associated lactic acidosis is rare and potentially severe. The underlying mechanism seems to involve the inhibition of pyruvate-dehydrogenase activity and suppression mitochondrial transport, which increases anaerobic metabolism and the production of lactate. It presents with nonspecific gastrointestinal symptoms, tachypnoea, tachycardia, arrhythmia, renal insufficiency or coma.4,5 It has been described in diabetic patients with significant comorbidities and in adult patients with acute overdose, but few cases have been described in the previously healthy paediatric population, and all such cases have occurred in the context of suicide attempts. Hypoglycaemia does not usually develop unless other drugs are combined with metformin.4 In case 1, the patient presented with lactic acidosis with renal insufficiency and hypoglycaemia.
In cases of NSAID poisoning, especially those involving ibuprofen and naproxen, metabolic acidosis results from the accumulation of the drugs themselves and of the acid metabolites derived from propionic acid, which cause an increase in the anion gap. Lactate elevation in these cases is moderate and probably secondary to hypoxia.6 The most frequent manifestations are gastrointestinal, and neurologic manifestations (seizures or altered level of consciousness) are indicative of severe poisoning, as occurred in case 2. Patients may also develop renal impairment.6 This picture has been described in paediatric patients with intentional poisoning with massive overdoses.
On the other hand, case 3 suggested that severe toxicity (lactic acidosis and renal insufficiency) may develop with the combined ingestion of metformin and a NSAID, even if the serum drug levels are not very high.
The initial management of metabolic lactic acidosis in these patients includes supportive care measures, clinical and electrocardiographic monitoring and serial arterial blood gas tests.2 In most cases, treatment is based on fluid therapy and administration of bicarbonate. Some patients may require haemodyalisis.2
There are few published data on serum drug levels in cases similar to those presented here. Metformin concentrations of 63.3 and 165μg/mL and naproxen concentrations of 1290μg/mL have been reported in the past, which are comparable to the concentrations found in cases 1 and 2 in our study.4–6 The half-life of metformin in case 1 (9.2h) was slightly longer than expected (6.5h), while the half-life of naproxen in case 2 (14.8h) was consistent with the theoretical half-life (15h). In case 3, the half-lives of naproxen and ibuprofen (21.9 and 5.6h, respectively) the elimination half-lives exceeded the theoretical values. This could be related to the development of renal insufficiency in both cases, which probably contributed to the prolongation of toxicity.
In short, metabolic lactic acidosis can serve as a clue to consider a possible metformin or NSAID intoxication.2,3 Similarly, if poisoning with any of these drugs is suspected, monitoring blood gases and renal function is a must. Although drug plasma concentrations do not always correlate to symptoms or outcomes, the identification of the involved drugs in the cases presented in this article allowed the elucidation of the cause of toxicity.
Please cite this article as: Habimana-Jordana A, López-Corominas V, Barceló-Martín B, Gomila-Muñiz I, Martínez-Sánchez L. Acidosis metabólica láctica como manifestación de intoxicación voluntaria en adolescentes. An Pediatr (Barc). 2019;90:121–123.
Previous presentations: the results of this study were presented in part at the XXI Jornadas Nacionales de Toxicología Clínica and the XI Jornadas Nacionales de Toxicovigilancia, November 2017, Santiago de Compostela, Spain.