Fever without a source (FWS) in infants aged less than 90 days is a common reason for paediatric emergency department (PED) visits. At present, the clinical evaluation, complete blood count, rapid microbiological tests and specific biochemical and haematological biomarker tests (including the white blood cell count, serum C-reactive protein [CRP] and procalcitonin [PCT]) are used to guide the presumptive aetiological diagnosis and management of these patients.1
The use of flow cytometry (FC) to analyse the immune response in infectious disease is gaining relevance in clinical practice.2 Flow cytometry is used to determine the presence or absence of leukocyte surface proteins bound to a fluorophore by means of laser stimulation.3 One of the most studied proteins is CD64, an Fc receptor for immunoglobulins that is constitutively expressed on the surface of monocytes and macrophages. Its expression increases in these cells as well as in neutrophils in response to inflammatory cytokines.4
In the case of CD64, the percentage of positive neutrophils and its surface expression seem to be higher in bacterial compared to viral infections.5 Consequently, CD64 has been proposed as a potential novel biomarker of infection.3 In addition, the fact that CD64 measurement requires only a small blood sample and its high specificity makes it particularly interesting for the management of infants.5
We present the results of a pilot study evaluating the feasibility of CD64 as a biomarker of infection in infants aged less than 90 days with FWS managed in the PED setting. The primary objective was to describe leukocyte subpopulations and CD64 expression in neutrophils. We subsequently compared these findings to those in a cohort of healthy children and analysed the correlation with classical infection biomarkers.
We conducted a single-centre prospective descriptive pilot study. The study was approved by the ethics committee of the hospital (file R-0049/20). We collected clinical, laboratory and FC data after obtaining consent to participation from the parents or caregiver. Flow cytometry was carried out in 100 µL specimens of blood obtained from the remaining volume of samples collected for the complete blood count at the PED. We analysed leukocyte subpopulations and CD64 expression in neutrophils (an explanation of the methodology can be found in Appendix 1). The study included infants aged less than 3 months with FWS managed at PED between September 2020 and October 2023. We compared the collected data for the variables of interest with the findings of a previous study conducted in a sample of 183 healthy children.2
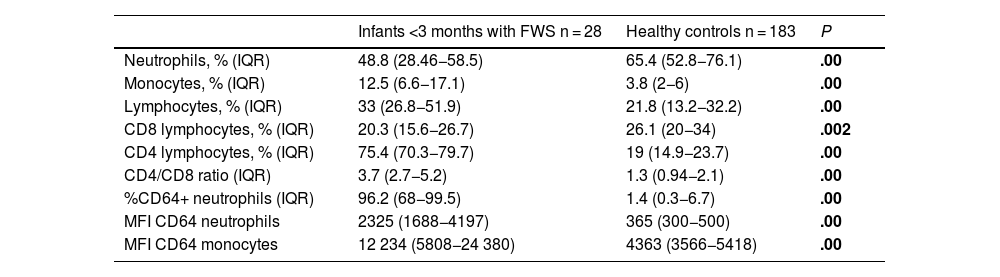
The sample included 28 patients, 20 of whom were male. The median age was 45 days (IQR, 22−68 days), and the median time elapsed from onset of fever to the visit was 4 h (IQR, 2−12 hours). The median leukocyte count was 10 600 cells/µL (IQR, 7300−15 200 cells/µL), with an absolute neutrophil count of 4760 cells/µL (IQR, 1900–8600 cells/µL), absolute lymphocyte count of 3900 cells/µL (IQR, 2400–6000 cells/µL) and an absolute monocyte count of 1200 cells/µL (IQR, 600–1900 cells/µL). Table 1 presents the leukocyte count values, CD64 expression values and their comparison with results in healthy controls.
Leukocyte populations and CD64 expression, comparison with Mann–Whitney U test.
| Infants <3 months with FWS n = 28 | Healthy controls n = 183 | P | |
|---|---|---|---|
| Neutrophils, % (IQR) | 48.8 (28.46−58.5) | 65.4 (52.8−76.1) | .00 |
| Monocytes, % (IQR) | 12.5 (6.6−17.1) | 3.8 (2−6) | .00 |
| Lymphocytes, % (IQR) | 33 (26.8−51.9) | 21.8 (13.2−32.2) | .00 |
| CD8 lymphocytes, % (IQR) | 20.3 (15.6−26.7) | 26.1 (20−34) | .002 |
| CD4 lymphocytes, % (IQR) | 75.4 (70.3−79.7) | 19 (14.9−23.7) | .00 |
| CD4/CD8 ratio (IQR) | 3.7 (2.7−5.2) | 1.3 (0.94−2.1) | .00 |
| %CD64+ neutrophils (IQR) | 96.2 (68−99.5) | 1.4 (0.3−6.7) | .00 |
| MFI CD64 neutrophils | 2325 (1688−4197) | 365 (300−500) | .00 |
| MFI CD64 monocytes | 12 234 (5808−24 380) | 4363 (3566−5418) | .00 |
FWS, fever without source; IQR, interquartile range; MFI, mean fluorescence intensity.
Significant values are presented in boldface.
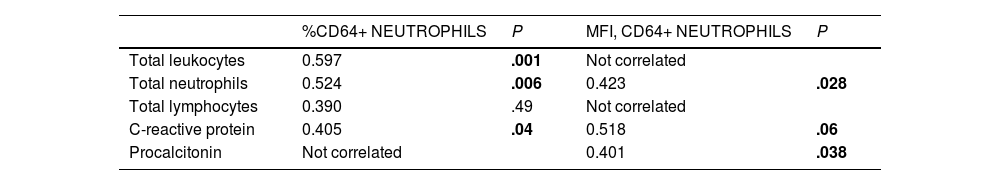
In the cohort under study there were 11 cases of urinary tract infections and 3 viral infections confirmed by polymerase chain reaction. In the rest of infants, microbiological tests were negative. We found no significant differences between groups. Table 2 presents the correlations with classical biomarkers.
Correlation to classical biomarkers (Spearman).
| %CD64+ NEUTROPHILS | P | MFI, CD64+ NEUTROPHILS | P | |
|---|---|---|---|---|
| Total leukocytes | 0.597 | .001 | Not correlated | |
| Total neutrophils | 0.524 | .006 | 0.423 | .028 |
| Total lymphocytes | 0.390 | .49 | Not correlated | |
| C-reactive protein | 0.405 | .04 | 0.518 | .06 |
| Procalcitonin | Not correlated | 0.401 | .038 |
Leukocytes, neutrophils and lymphocytes were identified in the flow cytometry (FC) dot-plot profile and gated. We assessed the correlation with the biomarker values obtained from the samples used in the FC analysis. The intensity of CD64 surface expression was measured as mean fluorescence intensity (MFI) in arbitrary units. We expressed the frequency of expression as percentage of neutrophils positive for CD64 over the total. Significant P values are presented in boldface.
In our study, CD64 expression in infants aged less than 90 days with FWS was higher compared to the expression reported in healthy controls. Furthermore, CD64 expression exhibited an adequate correlation with classical biomarkers.
As noted above, there is a dearth of evidence on the use of FC as a diagnostic test for FWS in the PED setting.1 Based on our pilot study, the potential role of CD64 as a biomarker is of great interest. It is known that CD64 is a component of innate immunity,6 which is crucial in infections in infants under 3 months.2 In addition, its levels do not correlate to age. We observed an elevation in CD64 expression, which was likely due to an underlying inflammatory response. The correlation with other classical biomarkers supports this hypothesis.
The analysis of CD64, combined to other biomarkers, could allow the description of bacterial versus non-bacterial patterns in infants aged less than 3 months with FWS.3,4 This fact, described in other contexts, could facilitate the presumptive diagnosis and treatment.5 We were not able to describe differences between urinary tract infections and viral infections. This was not an objective of this pilot study, but is an aspect that needs to be studied. There is evidence that CD64 expression may not increase in localized infections.1
There are important limitations to our study related to its design, such as its having been conducted in a single centre nature and the small sample size. In addition, the application of FC requires specific skills, which may limit its implementation in other centres.
In conclusion, the use of FC and CD64 analysis in infants aged less than 90 days with FWS appears to be feasible in the PED. We observed an increase in CD64 expression in neutrophils that was correlated to classical infection biomarkers, a finding that has not been previously reported. However, studies in larger samples are needed to confirm our findings.