Since Russia launched the military offensive against Ukraine on February 24, 2022, more than 4.5 million Ukrainians have fled their country.1 In Spain, more than 100 000 refugees have sought asylum since March 1,2 and based on data from the centres of reception, welfare and referral of Madrid, Alicante, Barcelona and Malaga, 38% are children aged 0–17 years.3
We present the results of a retrospective observational study in 2 tertiary care hospitals of the Community of Madrid between March and July 2022. The primary objective was to describe the care received by refugee children from Ukraine in emergency departments 5 months after the war started. We performed a descriptive analysis of categorical variables by calculating absolute and relative frequencies and of quantitative variables calculating the median and interquartile range (IQR). The study was approved by the research ethics committees of the two participating hospitals (ref. PI-5281).
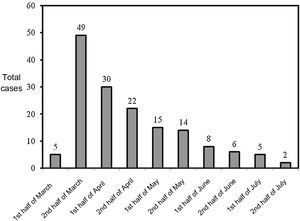
We analysed 156 emergency department visits made by refugee children from Ukraine in the period under study. The median age was 4.2 years (IQR, 2.1–8.9), and 52.6% of the patients were female. The number of emergency visits peaked in the second half of March (49/156; 31.4%), followed by a gradual decrease (Fig. 1).
The most frequent presenting complaint was fever (46.7%), followed by gastrointestinal symptoms (23.1%). In 4 cases (2.5%) the visit was related to anxiety symptoms. Chronic diseases were present in 21.1% (33 patients), corresponding to haematological or oncological diseases in 7.7% of the total sample. In the subset of patients with chronic diseases, 21.2% sought care for complications of the underlying disease (Table 1).
Characteristics of the patients (N=156).
| n (%) | |
|---|---|
| Age distribution | |
| < 6 months | 9 (5.8%) |
| 6−12 months | 8 (5.1%) |
| 1−3 years | 45 (28.8%) |
| 3−6 years | 39 (25%) |
| 6−12 years | 45 (28.8%) |
| 12−16 years | 10 (6.4%) |
| Sex distribution | |
| Female | 82 (52.6%) |
| Male | 74 (47.4%) |
| Personal history | |
| Unremarkable | 123 (78.8%) |
| Chronic disease | 33 (21.1%) |
| Haematological/oncological | 12 (7.7%) |
| Neurologic | 5 (3.2%) |
| Gastrointestinal | 4 (2.6%) |
| Cardiological | 2 (1.3%) |
| Rheumatological | 2 (1.3%) |
| Renal/urological | 1 (0.6%) |
| Other | 7 (4.5%) |
| Reason for visit | |
| Fever | 73 (46.7%) |
| Isolated | 32 (20.5%) |
| Fever and respiratory symptoms | 24 (15.4%) |
| Fever and gastrointestinal symptoms | 17 (10.9%) |
| Gastrointestinal symptoms | 36 (23.1%) |
| Cutaneous lesions | 10 (6.4%) |
| Respiratory symptoms | 8 (5.1%) |
| Complications of underlying chronic disease | 7 (4.5%) |
| Head trauma | 4 (2.6%) |
| Other | 18 (11.5%) |
| Diagnostic tests ordered in emergency department | |
| None | 93 (59.6%) |
| Blood tests | 42 (26.9%) |
| Urine tests | 17 (10.8%) |
| Imaging tests | 24 (15.3%) |
| Plain radiograph | 16 (10.2%) |
| Ultrasound | 7 (4.4%) |
| CT | 3 (1.9%) |
| Electrocardiogram | 2 (1.3%) |
In 40.3% of the visits, diagnostic tests were ordered in the emergency department, most frequently blood tests (26.9%). In the subset of children whose presenting complaint was with fever (73/156), 32.8% underwent blood tests; a percentage that rose to 75% (12/73) in the group with underlying chronic disease and fever. Ninety-one percent (142/156) were discharged from the emergency department, in one case by the patient’s request. Thirteen (8.3%) were admitted to hospital, with a median length of stay of 4 days (IQR, 3–9). None required admission to the paediatric intensive care unit. One patient, who had congenital hydrocephalus, required urgent neurosurgery. Lastly, one patient was admitted to hospital at home services for a total of 15 days.
Refugee children are a particularly vulnerable collective, and the impact of both war and displacement can be devastating to their health. Exposure to traumatic and stressful events promotes the development of mental health problems, and it is estimated that 1 in 5 of those affected by the war will develop a psychiatric disorder.4 In this case series, emergency visits related to mental health amounted to 2.5% of the total, perhaps because these type of disorders could be assessed directly in primary care and/or other care settings rather than emergency departments, which could account for the low proportion found in this series.
In the context of an armed conflict, crowding may cause disruptions in the continuity of care and difficulty adhering to treatment, resulting in decompensation in patients with chronic diseases.5 Approximately 1 in 4 of the refugee children managed in the emergency department had underlying chronic diseases, chiefly blood tumours. In this regard, both the Sociedad Española de Hematología y Oncología Pediátrica (Spanish Society of Paediatric Haematology and Oncology) and multiple private associations have joined efforts in Spain to collaborate in welcome and welfare projects that target Ukrainian children with cancer.
The assessment of febrile patients in the emergency care setting depends on several factors, such as age, associated symptoms, personal history and vaccination status. In the context under study, one of the main limitations in the assessment of immigrant children with fever was that in many cases the vaccination history was unknown. The current immunization schedule of Ukraine, last updated in 2018, does not cover vaccination against pneumococcal or meningococcal disease, varicella or human papillomavirus, unlike the immunization schedule in Spain. According to data from the European Centre for Disease Prevention and Control, vaccination coverage in Ukraine ranges from 50% to 80%, so that Ukrainian children constitute a risk group for infrequent but potentially severe viral and bacterial infectious diseases,6 such as tuberculosis, infection by human immunodeficiency virus, viral hepatitis, measles, mumps and rubella. These circumstances were taken into account in the approach taken in our emergency departments, with frequent performance of blood tests in children presenting with fever (1:3 cases), especially if they had a chronic disease (3:4 cases).