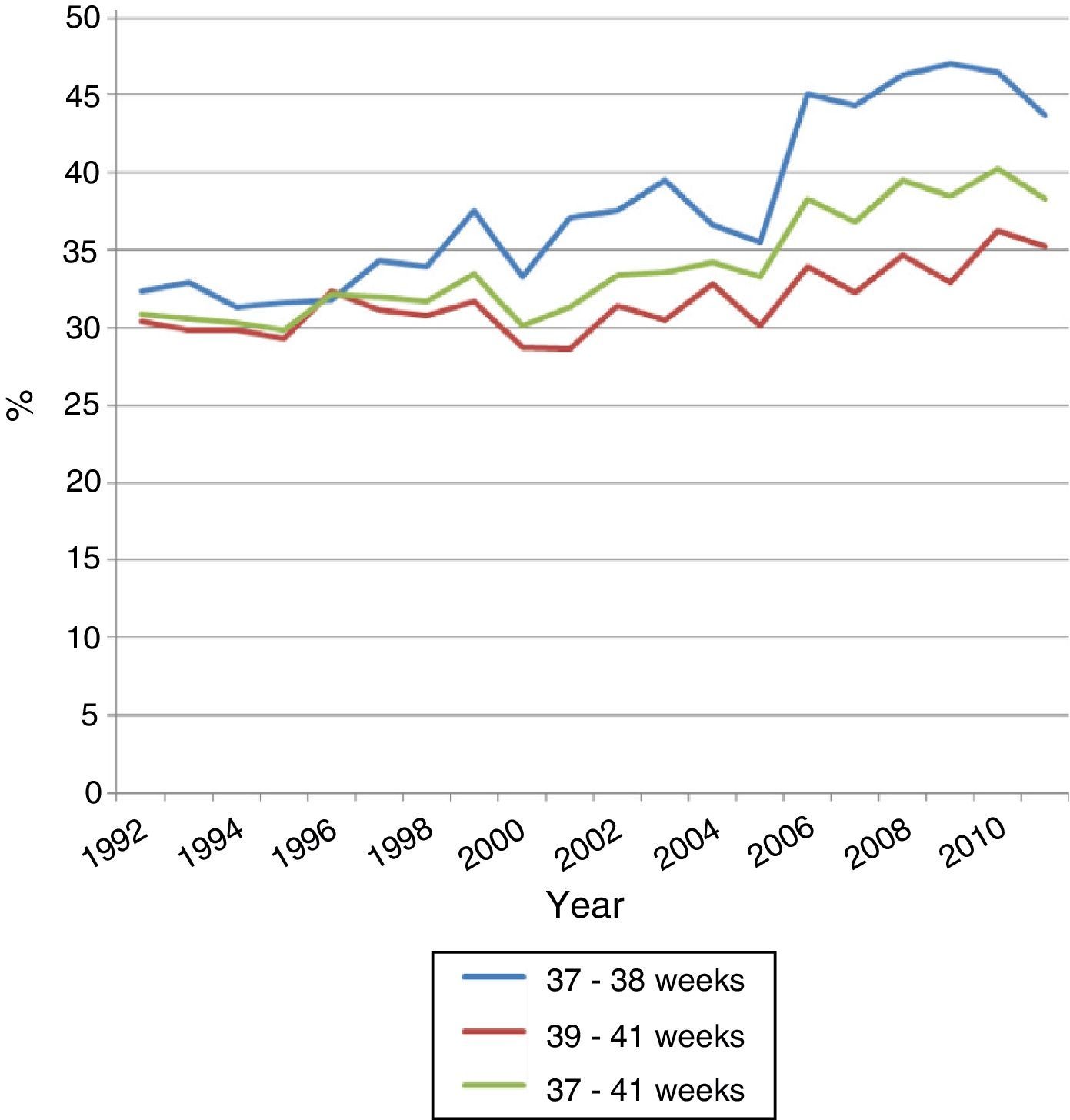
In the last decades neonatal morbidity has increased significantly. The birth of children from 37 to 38 weeks of gestation, a period called early term, has significantly increased in the past twenty years or so, parallel to the increase in induced deliveries and the caesarean rate.
Patients and methodRetrospective cohorts’ population study, which included those babies born between 37 and 41 weeks of gestation in the period 1992–2011 (n=35.539). This population was divided into two cohorts, early-term newborn (RNTP) of 37–38 weeks (n=11,318), and full-term newborn (RNTC), of 39–41 weeks of gestation (n=24,221). The rates of caesarean section, neonatal unit admission, respiratory morbidity, apnea, need for assisted ventilation, hyperbilirubinemia requiring phototherapy, hypoglycemia, seizures, hypoxic-ischaemia encephalopathy, need for parenteral nutrition and early sepsis were all reviewed.
ResultsThere was a progressive increase in the number of caesarean sections throughout the period studied (from 30.9% to 40.3%). The caesarean section rate was higher in RNTP than in the RNTC (38.3% vs. 31.3%, P<.0001). On comparing the two groups, significant differences were found in: the rate of admission to neonatal unit, 9.1% vs. 3.5% (P<.0001); respiratory morbidity (hyaline membrane 0.14% vs. 0.007% [P<.0001]; transient tachypnea 1.71% vs. 0.45% [P<.0001]; mechanical ventilation 0.2% vs. 0.07% [P<.009]; continuous positive airway pressure 0.11% vs. 0.01% [P<.0001]); phototherapy 0.29% vs. 0.07% (P<.0001); hypoglycemia 0.54% vs. 0.11% (P<.0001), and parenteral nutrition 0.16% vs. 0.04% (P<.0001). There were no significant differences in the rate of early sepsis, pneumothorax, aspiration syndromes, seizures and hypoxic-ischaemic encephalopathy.
ConclusionsIn our environment there is a significant number of RNTP, which have a significantly higher morbidity than newborns RNTC registered. After individualising each case, it is essential not to end a pregnancy before 39 weeks of gestation, except for maternal, placental or foetal conditions indicating that continuing the pregnancy may increase the risk for the foetus and/or the mother.
En las últimas décadas ha aumentado de forma significativa el nacimiento de niños de 37 y 38 semanas de gestación, período denominado a término precoz, paralelamente al aumento de partos inducidos y el incremento en la tasa de cesáreas.
Pacientes y métodoEstudio retrospectivo poblacional de cohortes, en el que se incluyó a los nacidos entre las 37 y 41 semanas de gestación en el período 1992-2011 (n=35.539). Esta población se dividió en 2 cohortes, los recién nacidos a término precoz (RNTP), de 37-38 semanas (n=11.318), y los recién nacidos a término completo (RNTC), de 39-41 semanas (n=24.221). Se analizan la tasa de cesárea, el ingreso en unidad neonatal, la morbilidad respiratoria, la apnea y la necesidad de asistencia respiratoria, hiperbilirrubinemia que requiere fototerapia, hipoglucemia, convulsiones, encefalopatía hipóxico-isquémica, necesidad de nutrición parenteral y sepsis precoz.
ResultadosSe observa un aumento progresivo del número de cesáreas a lo largo del período estudiado (del 30,9% al 40,3%). En los RNTP la tasa de cesárea fue superior que en los RNTC (38,3% vs. 31,3%; p<0,0001). En la comparación de ambos grupos, se encontraron diferencias significativas en la tasa de ingreso en unidad neonatal, 9,1% vs. 3,5% (p<0,0001); la morbilidad respiratoria (membrana hialina 0,14% vs. 0,007%; [p<0,0001]); la taquipnea transitoria, 1,71% vs. 0,45% (p<0,0001), la ventilación mecánica, 0,2% vs. 0,07% (p<0,009); la presión positiva continua en la vía respiratoria, 0,11% vs. 0,01% (p<0,0001); la fototerapia, 0,29% vs. 0,07% (p<0,0001); la hipoglucemia, 0,54% vs. 0,11% (p<0,0001), y la nutrición parenteral, 0,16% vs. 0,04% (p<0,0001). No se encontraron diferencias significativas en la tasa de sepsis precoz, neumotórax, síndromes aspirativos, convulsiones y encefalopatía hipóxico-isquémica.
ConclusionesEn nuestro medio, existe un número importante de RNTP, que presentan una morbilidad significativamente superior a los recién nacidos catalogados de RNTC. Tras individualizar cada caso, es aconsejable no finalizar un embarazo antes de las 39 semanas de gestación, salvo por condicionamientos maternos, placentarios o fetales que indiquen que continuar el embarazo comporte un mayor riesgo para el feto y/o la madre.
In the past few decades there has been an increase in the number of caesarean deliveries, especially in developed countries, with a clear predominance of elective caesarean sections, many of which are of questionable indication.1 Within full-term gestational ages, caesarean delivery rates at 37 and 38 weeks, an interval known as early term, have been increasing significantly.2–4
Different studies show that newborns delivered at early term (ETNBs) have higher rates of neonatal morbidity than full-term newborns (FTNBs) (39–41 weeks),2 even after excluding maternal morbidity and confirming foetal maturity with amniocentesis.5,6
From what we have learned about brain development in recent decades, we know that the brain maturation process speeds up in the last 4–5 weeks of gestation (increases in brain mass, number of furrows and ridges, growth of axons and dendrites, and number of interconnections between the various brain structures). Therefore, ending gestation relatively early can alter the brain maturation process in some cases, particularly those with complications. From 2006 to date, different studies have reported poorer educational outcomes and increased the need for special education in the ETNB population.7–11
Although there are numerous studies on this subject, we have not found any for this population in Spain, so we performed a retrospective cohort study to assess the risk of morbidity in ETNBs.
Patients and methodsWe did a retrospective cohort study that included newborns delivered between 37 and 41 weeks of gestation in the 1992–2011 period (n=35,539). Gestational age was calculated in completed weeks based on the date of the last menstrual period and/or obstetric ultrasound. We divided this population in two, ETNBs delivered at 37–38 weeks of gestation (n=11,318) and FTNBs delivered at 39–41 weeks of gestation (n=24,221). No patients were excluded from the study.
For each cohort, we analysed the rates of caesarean delivery, admission to neonatal intensive care unit, respiratory morbidity, apnoea, and need for respiratory support, hyperbilirubinaemia requiring phototherapy, convulsions, hypoxic-ischaemic encephalopathy, need for parenteral nutrition, and early-onset sepsis.
We performed a comparative analysis of the incidence of each of the studied parameters between the ETNB and the FTNB groups. We analysed the data with the G.STAT software version 2.0, using the chi-squared test for a 95% confidence interval (CI) and risk factor analysis for an adverse outcome (odds ratio, 95% CI).
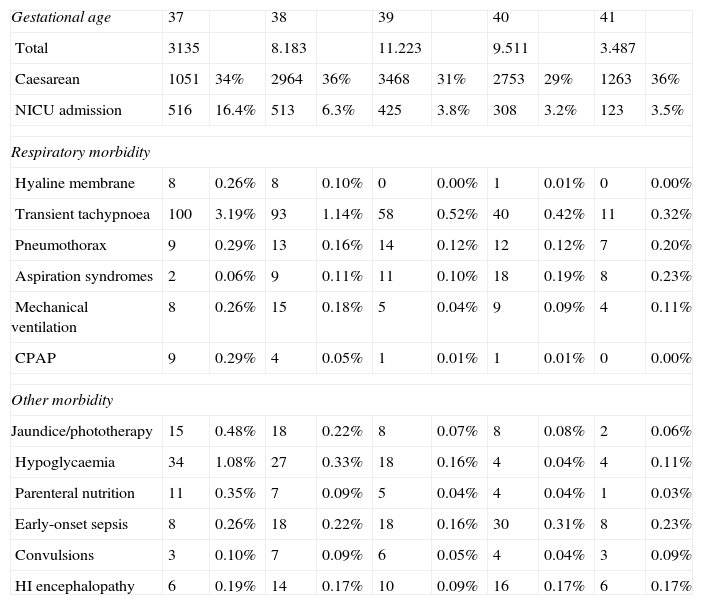
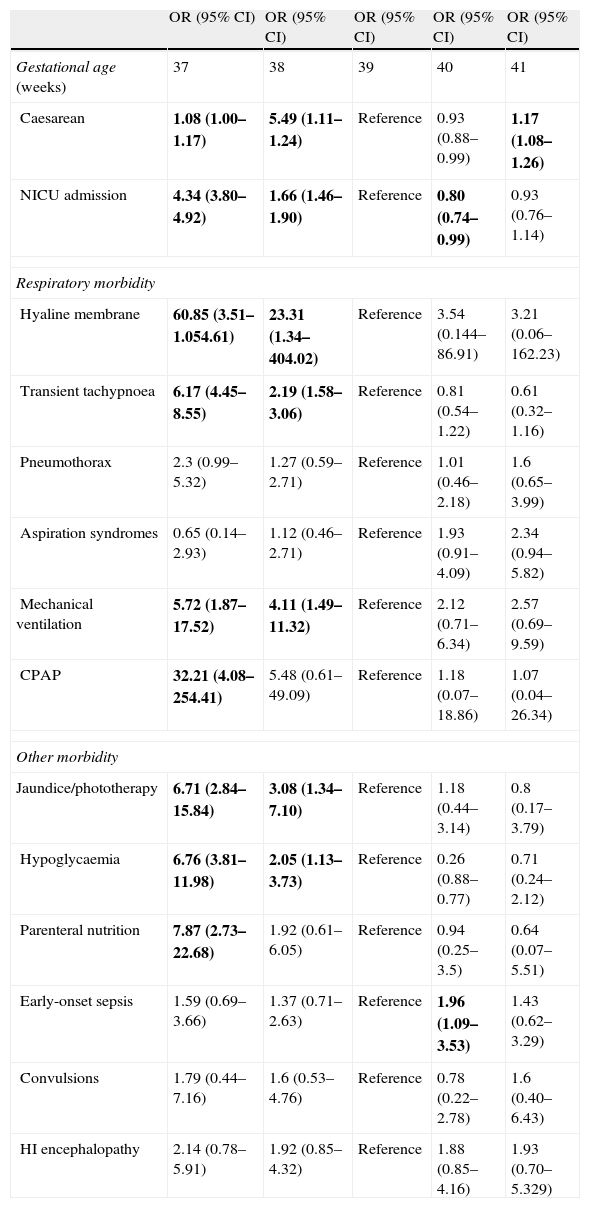
ResultsOur study showed a progressive increase in the number of caesarean deliveries throughout the studied period (Fig. 1). In ETNBs the caesarean rate was higher than in FTNBs (38.3% vs. 31.3%; p<0.0001). When we compared both groups we found significant differences in: the rates of neonatal intensive care unit admission, 9.1% vs. 3.5% (p<0.0001); respiratory morbidity (hyaline membrane 0.14% vs. 0.005% [p<0.0001]); transient tachypnoea, 1.71% vs. 0.45% (p<0.0001); mechanical ventilation, 0.2% vs. 0.07% (p<0.009); continuous positive airway pressure, 0.11% vs. 0.01% (p<0.0001); phototherapy, 0.29% vs. 0.07% (p<0.0001); hypoglycaemia, 0.54% vs. 0.11% (p<0.0001), and parenteral nutrition, 0.16% vs. 0.04% (p<0.0001). We did not find significant differences in the rates of early-onset sepsis, pneumothorax, aspiration syndromes, convulsions, and hypoxic-ischaemic encephalopathy (Tables 1 and 2).
Incidence of neonatal morbidity in the population of neonates born at 37–41 weeks of gestation between 1992 and 2011.
| Gestational age | 37 | 38 | 39 | 40 | 41 | |||||
| Total | 3135 | 8.183 | 11.223 | 9.511 | 3.487 | |||||
| Caesarean | 1051 | 34% | 2964 | 36% | 3468 | 31% | 2753 | 29% | 1263 | 36% |
| NICU admission | 516 | 16.4% | 513 | 6.3% | 425 | 3.8% | 308 | 3.2% | 123 | 3.5% |
| Respiratory morbidity | ||||||||||
| Hyaline membrane | 8 | 0.26% | 8 | 0.10% | 0 | 0.00% | 1 | 0.01% | 0 | 0.00% |
| Transient tachypnoea | 100 | 3.19% | 93 | 1.14% | 58 | 0.52% | 40 | 0.42% | 11 | 0.32% |
| Pneumothorax | 9 | 0.29% | 13 | 0.16% | 14 | 0.12% | 12 | 0.12% | 7 | 0.20% |
| Aspiration syndromes | 2 | 0.06% | 9 | 0.11% | 11 | 0.10% | 18 | 0.19% | 8 | 0.23% |
| Mechanical ventilation | 8 | 0.26% | 15 | 0.18% | 5 | 0.04% | 9 | 0.09% | 4 | 0.11% |
| CPAP | 9 | 0.29% | 4 | 0.05% | 1 | 0.01% | 1 | 0.01% | 0 | 0.00% |
| Other morbidity | ||||||||||
| Jaundice/phototherapy | 15 | 0.48% | 18 | 0.22% | 8 | 0.07% | 8 | 0.08% | 2 | 0.06% |
| Hypoglycaemia | 34 | 1.08% | 27 | 0.33% | 18 | 0.16% | 4 | 0.04% | 4 | 0.11% |
| Parenteral nutrition | 11 | 0.35% | 7 | 0.09% | 5 | 0.04% | 4 | 0.04% | 1 | 0.03% |
| Early-onset sepsis | 8 | 0.26% | 18 | 0.22% | 18 | 0.16% | 30 | 0.31% | 8 | 0.23% |
| Convulsions | 3 | 0.10% | 7 | 0.09% | 6 | 0.05% | 4 | 0.04% | 3 | 0.09% |
| HI encephalopathy | 6 | 0.19% | 14 | 0.17% | 10 | 0.09% | 16 | 0.17% | 6 | 0.17% |
Adjusted odds ratio (95% CI) for neonatal morbidity among the population of neonates born at 37–41 weeks of gestation in the1992–2011 period.
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Gestational age (weeks) | 37 | 38 | 39 | 40 | 41 |
| Caesarean | 1.08 (1.00–1.17) | 5.49 (1.11–1.24) | Reference | 0.93 (0.88–0.99) | 1.17 (1.08–1.26) |
| NICU admission | 4.34 (3.80–4.92) | 1.66 (1.46–1.90) | Reference | 0.80 (0.74–0.99) | 0.93 (0.76–1.14) |
| Respiratory morbidity | |||||
| Hyaline membrane | 60.85 (3.51–1.054.61) | 23.31 (1.34–404.02) | Reference | 3.54 (0.144–86.91) | 3.21 (0.06–162.23) |
| Transient tachypnoea | 6.17 (4.45–8.55) | 2.19 (1.58–3.06) | Reference | 0.81 (0.54–1.22) | 0.61 (0.32–1.16) |
| Pneumothorax | 2.3 (0.99–5.32) | 1.27 (0.59–2.71) | Reference | 1.01 (0.46–2.18) | 1.6 (0.65–3.99) |
| Aspiration syndromes | 0.65 (0.14–2.93) | 1.12 (0.46–2.71) | Reference | 1.93 (0.91–4.09) | 2.34 (0.94–5.82) |
| Mechanical ventilation | 5.72 (1.87–17.52) | 4.11 (1.49–11.32) | Reference | 2.12 (0.71–6.34) | 2.57 (0.69–9.59) |
| CPAP | 32.21 (4.08–254.41) | 5.48 (0.61–49.09) | Reference | 1.18 (0.07–18.86) | 1.07 (0.04–26.34) |
| Other morbidity | |||||
| Jaundice/phototherapy | 6.71 (2.84–15.84) | 3.08 (1.34–7.10) | Reference | 1.18 (0.44–3.14) | 0.8 (0.17–3.79) |
| Hypoglycaemia | 6.76 (3.81–11.98) | 2.05 (1.13–3.73) | Reference | 0.26 (0.88–0.77) | 0.71 (0.24–2.12) |
| Parenteral nutrition | 7.87 (2.73–22.68) | 1.92 (0.61–6.05) | Reference | 0.94 (0.25–3.5) | 0.64 (0.07–5.51) |
| Early-onset sepsis | 1.59 (0.69–3.66) | 1.37 (0.71–2.63) | Reference | 1.96 (1.09–3.53) | 1.43 (0.62–3.29) |
| Convulsions | 1.79 (0.44–7.16) | 1.6 (0.53–4.76) | Reference | 0.78 (0.22–2.78) | 1.6 (0.40–6.43) |
| HI encephalopathy | 2.14 (0.78–5.91) | 1.92 (0.85–4.32) | Reference | 1.88 (0.85–4.16) | 1.93 (0.70–5.329) |
Significant odds ratio (OR) in bold.
The progressive increase in the number of elective caesarean deliveries in the past years has been accompanied by an increase in neonatal morbidity, especially among ETNBs, bringing about various studies that have been analysing the causes for the increase in elective caesarean deliveries. Caesarean delivery after a previous caesarean section is considered the main cause for the increase in the number of these deliveries4; the study by Nir et al.12 reports additional causes, such as delivery after long-term infertility and/or older maternal age, and the belief that a caesarean section is the safest way for both mother and child to end labour. Pregnant women request this procedure for these additional reasons. However, this study shows that ending gestation at term but before 39 weeks due to provider and/or patient preference when there is no clear medical indication, even if foetal lung maturity has been confirmed, leads to increased neonatal morbidity, as was also shown by Wilmink et al.13 and Fang et al.5 The optimal time for an elective delivery remains controversial, as the ETNB population is currently considered the continuation of the late preterm population due to its high morbidity.12,14 The American College of Obstetricians and Gynecologists only finds elective deliveries before 39 weeks acceptable if foetal lung maturity has been confirmed. The results of most studies show that neonatal morbidity starts to decrease sometime between 39 and 41 weeks of gestation. Only the studies done by Yee et al.15 and Luca et al.16 reported a decrease in morbidity starting at 38 weeks and 4 days of gestational age, for the first, and between 38 and 40 weeks for the latter. Some obstetricians justify performing caesarean deliveries at term but before 39 weeks of gestation as a means to prevent a greater number of stillbirths.17 In 2007, Clark et al.18 started a study in 14 states of the United States implementing three different policies to decrease the rate of early-term deliveries. The first was a “hard stop” approach that prohibited elective induction of labour and primary and repeat caesarean sections before 39 weeks of gestation; the second was a “soft stop” approach that allowed elective deliveries if the clinician justified them; and the third was an “education only” approach in which professionals were informed of the higher morbidity found in ETNBs. After two years, all the variables under study were measured again, showing a significant decrease both in the rate of elective deliveries in that period and in the rate of admission to neonatal intensive care units, with no significant difference in the stillbirth rate. We should note that the greater decrease in the number of induced deliveries in ETNBs was observed in the centres that adopted the most stringent control measures. However, further randomised clinical trials with a sufficiently large population-based sample must be conducted to have strong evidence for these conclusions.
Likewise, no decrease in maternal morbidity has been observed when mothers are delivered prior to 39 weeks. And while maternal morbidity is one of the reasons for performing caesarean deliveries, in most instances there is no significant reduction in morbidity as a result of delivering before 39 weeks. An increase in the length of hospital stay has been observed, but it is considered to be influenced by the increase in the hospital stay of the newborn.5 The increased morbidity observed repeatedly in a considerable number of studies on elective delivery prior to 39 weeks has led the Joint Commission to consider low rates of elective-term delivery a national quality indicator since 2010.18
In our study we observed a clear increase of neonatal morbidity in the ETNB population at 37 weeks of gestation that was maintained at 38 weeks with a subsequent decrease between 39 and 41 weeks (FTNB), as has been observed in most studies conducted in various countries. The main type of morbidity associated to early-term delivery is respiratory morbidity. This is explained in part by the relative immaturity involved in elective delivery, and partly by caesarean section deliveries in which fewer catecholamines and cortisol – compounds that contribute to lower production and increased clearance of lung fluid – are released during labour.4,19
Recently, Ghartey et al.3 conducted an extensive study comparing respiratory morbidity in early-term and full-term deliveries that showed clearly higher rates in the early-term population. Other authors have obtained similar results, for instance is the important study published by the Consortium on Safe Labour, which included 233,844 neonates.20 Tita et al.17 also published a study that sought evidence on the number of weeks of gestation at which it would be safe to practise repeat caesarean sections, and observed that performing them between 37 and 38 weeks resulted in an increase in neonatal morbidity, both respiratory and non-respiratory, with no apparent benefit to the mother. While in all of these studies the percentage of the different conditions that compose neonatal morbidity in these patients is not too high, it does have a considerable impact in the healthcare systems of the various countries, as the small increases in the rate of neonatal intensive care admission and length of hospital stay involve a considerable economic burden, with the study by Clark et al.18 reporting a yearly cost of nearly a billion dollars in the United States.
Lastly, we should note that morbidity in the ETNB population not only affects the neonatal period, but that this population shows lower IQ scores and increased special educational needs in children of school age compared with the FTNB population.7–11
The results of our study are consistent with those of most studies conducted to date. We observed a clear increase in respiratory morbidity in ETNBs; non-respiratory morbidity was also considerable, with significantly higher rates of hypoglycaemia and non-physiologic hyperbilirubinaemia which, on their own, can bring about neurological disease in the long term.21 The main limitation of our study was that it should have analysed whether births were spontaneous or induced, and caesarean sections elective or emergency, to better define morbidity in this population. These data would allow us to evaluate possible changes to obstetrics protocols for the benefit of neonates and their mothers. When it came to potential neurodevelopmental alterations, this study was limited because there was no follow-up of the early-term population that did not have neonatal complications. Thus, we do not know whether our ETNB population shows neurological abnormalities in the mid- or long-term. However, we ought to note that studies conducted in several universities in the United States and Chile show that children born at 37 through 41 weeks of gestation present differences in the Bayley scale at one year of age, suggesting that neurodevelopment is optimal in children born between 39 and 41 weeks of gestation.22,23
ConclusionsThis study showed that there is a significant number of ETNBs in our centre, and that they show a significantly higher morbidity than neonates categorised as FTNBs. Therefore, after taking into account the particularities of each individual case, it is paramount that no deliveries be made prior to 39 weeks of gestation except when maternal, placental or foetal conditions indicate that continuing the pregnancy would pose a higher risk for the foetus and/or the mother than ending it before the 39th week.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Martínez-Nadal S, Demestre X, Raspall F, Álvarez JA, Elizari MJ, Vila C, et al. Morbilidad neonatal en los recién nacidos a término precoz. An Pediatr (Barc). 2014;81:39–44.
Previously presented at the XIX Congreso de la Societat Catalana de Pediatria, Vilafranca del Penedès, May 11, 2013.