To identify socio-cultural, obstetric and perinatal characteristics associated with complete breastfeeding (CBF) during the first 4 months of life, depending on maternal origin.
Materials and methodsSocio-cultural, obstetric and perinatal aspects associated with breastfeeding depending on maternal origin were evaluated in a longitudinal study in a representative infant population from Aragon (n=1452).
ResultsThe prevalence of CBF was higher in immigrant mothers than in those from Spain. CBF was maintained in 37.2% of the mothers from Spain at 4 months, compared with 43% of the immigrants (p=0.039) (RR Spanish/immigrants=0.76; 95% CI: 0.58–0.99); at 6 months this occurred in 13.9% vs. 23.8%, respectively (p<0.001) (RR Spanish/immigrants=0.52; 95% CI: 0.37–0.72). The factors associated with CBF at 4 months are different between both groups. Mothers born in Spain are older (p=0.002), have higher academic level (p=0.001), greater parity (p=0.003), and a higher probability of vaginal delivery (p=0.005), and their children have the highest anthropometric values at birth. However, in immigrant mothers, the maintenance of CBF was associated with a higher maternal body mass index and with working at home. In both groups, CBF remains more frequently in those mothers who do not smoke (p=0.001).
ConclusionsThe prevalence of CBF during the first months of life is higher in immigrant mothers than in those from Spain, and socio-cultural, obstetric and perinatal factors are different, depending on maternal origin.
Identificar las características socioculturales, obstétricas y perinatales asociadas con la lactancia materna completa (LMC) durante 4 meses, en dependencia del origen materno.
Material y métodosEstudio de una cohorte representativa de la población de lactantes aragoneses (n = 1.452). Se han evaluado las variables socioculturales, obstétricas y perinatológicas asociadas a la modalidad de lactancia materna, en dependencia del origen de la madre.
ResultadosLa prevalencia de LMC en nuestro medio es más alta en las madres inmigrantes que en las de origen español. El 37,2% de las de origen español mantienen la LMC a los 4 meses frente al 43% de las inmigrantes (p=0,039) (RR españolas/inmigrantes=0,76; IC del 95%, 0,58-0,99); a los 6 meses, esto ocurre en un 13,9% vs. 23,8%, respectivamente (p<0,001) (RR españolas/inmigrantes=0,52; IC del 95%, 0,37-0,72). Los factores que se asocian a la LMC a los 4 meses son diferentes entre ambos grupos. Las madres de origen español tienen más edad (p=0,002), nivel educativo (p=0,001), paridad (p=0,003) y mayor probabilidad de parto vaginal (p=0,005), y sus hijos presentan mayores valores antropométricos al nacimiento. Sin embargo, en las madres inmigrantes, el mantenimiento de LMC se asocia a un mayor índice de masa corporal materno y a no trabajar fuera del domicilio. En ambos grupos, la LMC se mantiene con más frecuencia en aquellas madres que no fuman (p=0,001).
ConclusionesLa prevalencia de LMC durante los primeros meses de edad es más alta en las madres inmigrantes que en las madres de origen español y los factores socioculturales, obstétricos y perinatales que se asocian a la misma son distintos en función del origen materno.
Environmental and nutritional factors in the early months of life (pre- and postnatal) can affect the health of the newborn (NB) and infant, modulating phenotypic outcomes in the short and the long term in predisposed subjects.1,2 The mechanism by which such factors influence gene expression is not clear as many of them interact, even across generations (epigenetically).3 Breastfeeding (BF) is the ideal nourishment for infants, due to the nutritional composition of the milk and its many health benefits. It is one of the nutrition milestones that can lower several illness risks in early childhood and later in life.4,5 Exclusive BF (EBF) for at least 3 months lowers the risk for otitis, lower respiratory tract infection, development of asthma, atopic dermatitis, or acute gastroenteritis, and in general BF has been shown to have a preventive effect on obesity, cardiovascular disease risk, diabetes mellitus, atopic disease, cancer, and cognitive development.6,7
Scientific and health institutions in Spain and abroad recommend EBF in the first 6 months of life and continued BF with adequate complementary feeding until two years of age or beyond.5–11 It is recommended that complementary feeding is introduced starting at 6 months so the diet provides adequate nutrition, meeting the needs of the developing child.11–13 The recently published data reveal an increasing trend in BF rates in some areas of Spain14; yet the prevalence and duration of BF are still low compared to other European Union countries.14–19 Promoting BF is a public health priority.
In recent years there has been a significant demographic shift in Spain, largely due to the arrival of immigrant population.20 In relation with infant nutrition, one of the major changes in Spain and also in other countries has been the higher BF initiation and prevalence rates in immigrant mothers.14,21
In addition to the obstetric and NB factors that affect BF initiation, the main socio-cultural and family aspects that have been shown to influence its initiation and continuation are the educational level of family members, the mother's age, tobacco use, adiposity, and parity.22–26 These factors are often interrelated or appear together.
A better knowledge of the factors associated to BF will help us identify nutritional risk situations and plan efficacious strategies to promote it. The objective of this study was to identify within our population the socio-cultural, obstetric, and perinatal characteristics associated with exclusive or predominant (complete) breastfeeding (CBF) in the first 4 months of life according to the mother's origin.
Materials and methodsThe CALINA27 (Crecimiento y Alimentación durante la Lactancia y la primera Infancia en Niños Aragoneses/Growth and Feeding during Infancy and Early Childhood in Children from Aragón) project is a longitudinal observational study on a cohort of children from Aragón from birth to 24 months of age. Its main goal is to assess the current growth pattern, body composition, feeding guidelines, and prenatal, postnatal, and psychosocial factors that determine the health and development of the infant.
The study was performed in a random sample of healthcare centres (HCCs) representative of the Autonomous Community of Aragón, which met the following inclusion criteria: to have paediatrics and nursing staff conducting the Programa de Salud Infantil (Health Child Programme), for a minimum of at least two years, and having fulfilled the goals and coverage rates for the programme for over 80% of the population served by the centre. The subjects included in the study were all children born in one natural year (from March 2009 to February 2010, both included) who attended the first routine check-up scheduled by the selected HCC, and whose parents signed the informed consent form.
The CALINA cohort included 1602 subjects (1156 from Zaragoza, 278 from Huesca, and 168 from Teruel, the three provinces of Aragón) and is representative of the population of children in Aragón.27 Out of this initial sample, we selected all NBs born to term (≥37 weeks; n=1452) and divided them into two groups according to their mothers’ origin: children of immigrant mothers (n=334) and children of Spanish mothers (n=1104). The CALINA project was approved by CEICA (Comité Ético de Investigación Clínica de Aragón/Clinical Research Ethics Board of Aragón).
We recorded the following variables for all children: (a) demographic data: parents’ country of origin, number of siblings, parents’ occupation and educational level; (b) obstetric and perinatal history: maternal anthropometrics before and after pregnancy, pregnancy complications, mother's tobacco use during pregnancy (we considered the mother a smoker if she smoked until the end of the pregnancy, regardless of amount), date of birth, sex, gestational age, delivery mode, perinatal complications, history that contraindicated or complicated BF; (c) BF: CBF duration, age BF was discontinued and reason for it, and (d) NB anthropometrics and nutrition following birth. The paediatrics and nursing staff of the selected centres collected the data for the variables during the routine check-up visits (15 days and months 1, 2, 3, 4, and 6) scheduled for the child in Primary Care.27
We defined EBF as feeding the infant breast milk alone with no additional liquids or solids, except for vitamin or mineral supplements. We defined predominant BF (PBF) as giving the child limited amounts of water or water-based liquids in addition to human milk. CBF comprehends both EBF and PBF.
We did the statistical analysis with the SPSS package version 19.0. We have expressed qualitative variables as frequency distributions in percentages for each category. For quantitative variables, we tested the normality of the distribution using the Kolmogorov–Smirnov test, and calculated measures of central tendency (mean or median) and of dispersion (standard deviation or percentiles). In the bivariate analysis, we did hypothesis testing comparing proportions when both variables were qualitative (chi-squared test, Fisher's exact test) and comparing means when one of them was quantitative (Student's t-test, ANOVA, and for non-normal distributions, Mann–Whitney U test or Kruskall–Wallis test). We identified the variables that showed significant differences between the group of infants fed by CBF up to 4 months of age and the other infants (non-CBF). Then, for qualitative variables we calculated the relative risk (RR) for the different proportions and their confidence intervals (CI) in relation to continued CBF at 4 months of age.
ResultsThe prevalence of CBF was significantly higher in the immigrant mother group than in Spanish mothers from birth to 6 months of age. At hospital discharge, the rate was 69.5% in Spanish mothers vs. 75.4% in immigrant mothers (p=0.034) (RR Spanish/immigrant=0.74; 95% CI, 0.56–0.97). CBF rates decreased gradually in both groups. At 3 months, 44.3% of Spanish mothers continued CBF vs. 53.8% of immigrant mothers (p=0.010) (RR Spanish/immigrant=0.69; 95% CI, 0.58–0.88). CBF at 4 months was 37.2% in Spanish mothers vs. 43% in immigrant mothers (p=0.039) (RR Spanish/immigrant=0.76; 95% CI, 0.58–0.99). At 6 months, only 13.9% of Spanish mothers and 23.8% of immigrant mothers continued CBF (p<0.001) (RR Spanish/immigrant=0.52; 95% CI, 0.37–0.72).
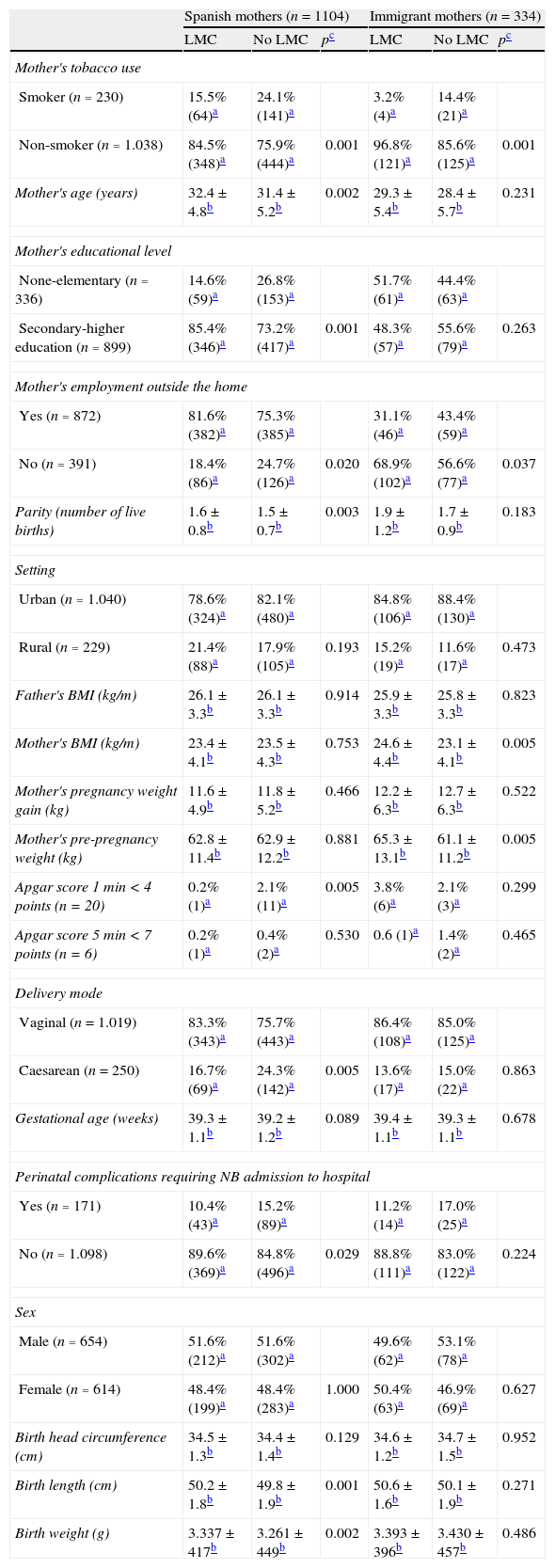
Table 1 gives the main socio-cultural, obstetric, and perinatal characteristics according to breastfeeding type. The data are presented separately for the Spanish and the immigrant mother groups.
Socio-cultural, obstetric, and perinatal characteristics that depend on mother's origin according to BF type at 4 months of age.
| Spanish mothers (n=1104) | Immigrant mothers (n=334) | |||||
| LMC | No LMC | pc | LMC | No LMC | pc | |
| Mother's tobacco use | ||||||
| Smoker (n=230) | 15.5% (64)a | 24.1% (141)a | 3.2% (4)a | 14.4% (21)a | ||
| Non-smoker (n=1.038) | 84.5% (348)a | 75.9% (444)a | 0.001 | 96.8% (121)a | 85.6% (125)a | 0.001 |
| Mother's age (years) | 32.4±4.8b | 31.4±5.2b | 0.002 | 29.3±5.4b | 28.4±5.7b | 0.231 |
| Mother's educational level | ||||||
| None-elementary (n=336) | 14.6% (59)a | 26.8% (153)a | 51.7% (61)a | 44.4% (63)a | ||
| Secondary-higher education (n=899) | 85.4% (346)a | 73.2% (417)a | 0.001 | 48.3% (57)a | 55.6% (79)a | 0.263 |
| Mother's employment outside the home | ||||||
| Yes (n=872) | 81.6% (382)a | 75.3% (385)a | 31.1% (46)a | 43.4% (59)a | ||
| No (n=391) | 18.4% (86)a | 24.7% (126)a | 0.020 | 68.9% (102)a | 56.6% (77)a | 0.037 |
| Parity (number of live births) | 1.6±0.8b | 1.5±0.7b | 0.003 | 1.9±1.2b | 1.7±0.9b | 0.183 |
| Setting | ||||||
| Urban (n=1.040) | 78.6% (324)a | 82.1% (480)a | 84.8% (106)a | 88.4% (130)a | ||
| Rural (n=229) | 21.4% (88)a | 17.9% (105)a | 0.193 | 15.2% (19)a | 11.6% (17)a | 0.473 |
| Father's BMI (kg/m) | 26.1±3.3b | 26.1±3.3b | 0.914 | 25.9±3.3b | 25.8±3.3b | 0.823 |
| Mother's BMI (kg/m) | 23.4±4.1b | 23.5±4.3b | 0.753 | 24.6±4.4b | 23.1±4.1b | 0.005 |
| Mother's pregnancy weight gain (kg) | 11.6±4.9b | 11.8±5.2b | 0.466 | 12.2±6.3b | 12.7±6.3b | 0.522 |
| Mother's pre-pregnancy weight (kg) | 62.8±11.4b | 62.9±12.2b | 0.881 | 65.3±13.1b | 61.1±11.2b | 0.005 |
| Apgar score 1min<4 points (n=20) | 0.2% (1)a | 2.1% (11)a | 0.005 | 3.8% (6)a | 2.1% (3)a | 0.299 |
| Apgar score 5min < 7 points (n=6) | 0.2% (1)a | 0.4% (2)a | 0.530 | 0.6 (1)a | 1.4% (2)a | 0.465 |
| Delivery mode | ||||||
| Vaginal (n=1.019) | 83.3% (343)a | 75.7% (443)a | 86.4% (108)a | 85.0% (125)a | ||
| Caesarean (n=250) | 16.7% (69)a | 24.3% (142)a | 0.005 | 13.6% (17)a | 15.0% (22)a | 0.863 |
| Gestational age (weeks) | 39.3±1.1b | 39.2±1.2b | 0.089 | 39.4±1.1b | 39.3±1.1b | 0.678 |
| Perinatal complications requiring NB admission to hospital | ||||||
| Yes (n=171) | 10.4% (43)a | 15.2% (89)a | 11.2% (14)a | 17.0% (25)a | ||
| No (n=1.098) | 89.6% (369)a | 84.8% (496)a | 0.029 | 88.8% (111)a | 83.0% (122)a | 0.224 |
| Sex | ||||||
| Male (n=654) | 51.6% (212)a | 51.6% (302)a | 49.6% (62)a | 53.1% (78)a | ||
| Female (n=614) | 48.4% (199)a | 48.4% (283)a | 1.000 | 50.4% (63)a | 46.9% (69)a | 0.627 |
| Birth head circumference (cm) | 34.5±1.3b | 34.4±1.4b | 0.129 | 34.6±1.2b | 34.7±1.5b | 0.952 |
| Birth length (cm) | 50.2±1.8b | 49.8±1.9b | 0.001 | 50.6±1.6b | 50.1±1.9b | 0.271 |
| Birth weight (g) | 3.337±417b | 3.261±449b | 0.002 | 3.393±396b | 3.430±457b | 0.486 |
CBF, complete breastfeeding; BMI, body mass index; NB, newborn.
In both the Spanish and the immigrant mother groups, continued CBF at 4 months of age was more frequent in non-smoking mothers (p=0.001) (RR Spanish=0.58; 95% CI, 0.42–0.80) (RR immigrants=0.20; 95% CI, 0.07–0.60) (Table 1).
The Spanish mothers who continued CBF until 4 months of age were older (32.4±4.8 vs. 31.4±5.2 years; p=0.002), had a higher educational level (p=0.001) (RR non-elementary/secondary-higher education=0.47; 95% CI, 0.33–0.65), worked outside the home more frequently, and had more children than mothers who did not continue BF. Also in this group, infants who continued CBF at 4 months were more likely to have an Apgar score <4 at 1min, were delivered vaginally more frequently (p=0.005) (RR vaginal/Caesarean delivery=1.60; 95% CI, 1.16–2.20), had a lower percentage of perinatal complications requiring hospital admission (p=0.029) (RR problems/no problems=0.65; 95% CI, 0.44–0.96), and had higher birth weights and lengths (Table 1). The variables for which there were no differences in Spanish mothers between the CBF group and the non-CBF group at 4 months were: type of setting (urban/rural), body mass index (BMI) of the parents, mother's pregnancy weight gain, gestational age, and sex.
Immigrant mothers who continued CBF until 4 months post-birth were smokers less frequently and also worked less frequently out of the home, and they had a higher BMI (24.6±4.4 vs. 23.1±4.1kg/m2; p=0.005) and a higher pre-pregnancy weight (65.3±13.1 vs. 61.1±11.2kg; p=0.005) than mothers who did not continue. There were no significant differences between both groups for the remaining variables (Table 1).
DiscussionThe results of this study show a considerable increase in the prevalence of CBF in the first six months of life compared to previous studies.16–19 The reported data complement the recently published global BF prevalence results in the same sample of infants from Aragón.14,27 In that study, BF of some type was maintained in over half of the infants at 6 months of age (54.3%) and in one quarter at one year (27.8%).14 Other studies in Spain show average BF prevalence rates of about 85% after birth, 42% at 3 months, and 12% at 6 months.16–19 According to the latest data of the INE (Instituto Nacional de Estadística/National Institute of Statistics), the prevalence of BF in Spain is about 66.2% after birth, 53.6% at 3 months, and 28.5% at 6 months.15
In this study, continued CBF decreased gradually after discharge from hospital, and kept dropping at a constant rate between the first and the third month. Starting on the fourth month, the decrease was sharper in Spanish mothers than in immigrant mothers. The lack of BF support on returning to the workplace at the end of maternity leave and its short duration (4 months) are barriers to continued BF.28 At 6 months of age, only 13.9% of infants of Spanish mothers and 23.8% of infants of immigrant mothers continued CBF. As of now, we do not have up-to-date nationwide figures for CBF in Spain. Differences between immigrant mothers and other mothers have also been observed in other countries such as France,29 Switzerland,30 United Kingdom,31 or Germany.32 In some instances the figures for breastfeeding initiation and continuation in immigrant mothers are higher than those in their countries of origin.21 This phenomenon has been attributed to the “healthy migrant effect”, although more studies are needed to confirm these data in different geographical areas.
One of the strengths of our study is that the data collection was integrated in the Programa de Salud Infantil performed routinely in Primary Care HCC. Before starting, the healthcare staff took a training and consensus course delivered by skilled members of the research group. The course dealt with the technique to be used and the inter- and intra-observer variability in measuring the child's anthropometric variables, and assured proper working knowledge of BF. Another strength is that the BF, socio-cultural, obstetric, and perinatal data of the sample are representative of the Autonomous Community of Aragón. The distribution of the studied social variables is similar to that found by the INE in the same year.20 CBF at 4 months of age is sufficiently prevalent in our setting to obtain a large enough sample size to perform an appropriate analysis. The immigrant population is spread out across the various participating HCCs, so during the study it was monitored by the same professionals who were assessing the non-immigrant population, preventing methodological biases. The CALINA project is a contemporary study that reflects the current socio-cultural characteristics of Aragón, which could be extrapolated to other autonomous communities in northern Spain.
In Aragón, one in three women smokes at the beginning of the pregnancy; of them, 25–50% quit smoking during gestation, and most resume smoking after delivery.14,33 The prevalence of smoking during pregnancy was higher in Spanish mothers (21.9%) than in immigrant mothers (8.7%).34 Factors such as the degree of addiction, a low perceived risk, or a low educational level are also associated to continued smoking during pregnancy and smoking during lactation.34 Our data show how in both groups CBF at 4 months of age was maintained more frequently in mothers who did not smoke during pregnancy. It would be advisable to set up intervention programmes. Pregnancy and lactation offer an opportunity to quit smoking and benefit the health of mother and child.
The parents’ educational level is an important factor that influences the variability of BF duration.14,25 In our sample, we observed that well-educated Spanish mothers had a higher prevalence of CBR at four months, but this was not an influencing factor in immigrant mothers. This may be because most immigrant mothers had a similar educational level. Mothers with higher educational levels continue BF longer in developed countries, while in developing countries the opposite is usually the case.31 In Spain today we have two societies that coexist and can show different behaviours and habits. A few decades ago BF was less prevalent in Spain in women with a high socio-economic status who worked outside the home.24 In recent years, healthy nutrition choices, such as BF, have been favoured by society.
The association between CBF and the mother's age or parity could also be related to the educational level of Spanish mothers, but not of immigrant mothers. In the group of Spanish mothers, those with higher educational levels were also older and had a greater number of children.
A higher pre-pregnancy BMI was associated to continuation of CBF at 4 months of age in immigrant mothers, but not in Spanish mothers. This finding has not been reported before and may be associated with better nutritional status in immigrant mothers who have a greater BF prevalence. In our setting, overweight in mothers is a protective factor for BF initiation and continuation, while obesity is associated with a lower prevalence.35
Other variables associated with CBF prevalence at 4 months of age are perinatal complications, type of delivery, and infant anthropometrics, but only in Spanish mothers. In our setting, the absence of perinatal complications and greater birth weight and length were associated to longer CBF duration in children of Spanish mothers. A recent study observed that infants with greater weights continue BF longer.32 It has also been reported that infants who were born small for their gestational age have a 40% lower probability to continue BF at 4 months.36 We can see that an adequate nutritional status of the NB and/or infant is associated with a higher probability of continued BF. All of the above did not apply to the group of immigrant mothers in our sample, probably because their risk for a low birth weight is much smaller, as was shown recently (9.2% in Spanish mothers vs. 3.8% in immigrants).37 Immigrant populations in some industrialised countries have obstetric, cultural, and maternal (age, habits) characteristics that result in a better overall health status in infants.21,37,38
In conclusion, the prevalence of CBF in the early months of life was greater in immigrant mothers than in Spanish mothers, and the socio-cultural, obstetric, and perinatal factors associated to it were different in each group. The negative correlation between tobacco consumption and CBF did not depend on the mother's origin. In Spanish mothers, a higher educational level, working outside the home, parity, vaginal delivery, a good perinatal evolution, and greater infant anthropometrics were associated to a higher probability of continued CBF at 4 months of age. In immigrant mothers, CBF at 4 months was associated with a greater weight and BMI of mother before the pregnancy. These findings identify the factors associated with continued CBF in our setting, as well as the differences that exist between them depending on the mother's origin. Knowledge of these factors will help develop strategies to promote BF tailored to different risk groups.
FundingThis work has received funding from the Instituto de Salud Carlos III of the Ministerio de Economía y Competitividad: (1) Ayuda PI080559, granted to the Instituto Aragonés de Ciencias de la Salud for the CALINA project, and (2) Red de Salud Materno Infantil y del Desarrollo (SAMID) RD08/0072.
Conflict of interestsThe authors have no conflicts of interest to declare.
Crecimiento y Alimentación durante la Lactancia y la primera Infancia en Niños Aragoneses (CALINA) Collaborative Group. Instituto de Investigación Sanitaria (Institute of Health Research), Aragón.
Coordinators: José L. Olivares López and Gerardo Rodríguez Martínez.
Collaborators: Dori Adivinación Herrero, Roberto Alijarde Lorente, M. Jesús Álvarez Otazu, M. Luisa Álvarez Sauras, Teresa Arana Navarro, Esther Atance Melendo, Ariadna Ayerza Casas, Concepción Balagué Clemos, M. Victoria Baños Ledesma, M. Lucía Bartolomé Lalanza, Teresa Bartrés Soler, M. Jesús Blasco Pérez-Aramendia, Purificación Broto Cosculluela, M. Jesús Cabañas Bravo, Rosa Cáncer Raginal, M. Inmaculada Cebrián Gimeno, Teresa Cenarro Guerrero, M. Begoña Chicote Abadía, María Cleofé Crespo Mainar, María Duplá Arenaz, Luis Carlos Elviro Mayoral, Concha Esteban Herréiz, Ángeles Falcón Polo, Jesús Feliz de Vargas Pastor, M. Teresa Fondevilla Pérez, M. Desamparados Forés Catalá, Amparo Fuertes Domínguez, Jorge Fuertes Fernández-Espinar, José Galán Rico, José Galbe Sánchez-Ventura, Matilde Gallego Pérez, Nuria García Sánchez, César García Vera, Ana-Luz Garín Moreno, M. Asunción Gila Gajón, Carmen Júdez Molina, Beatriz Kojtych Trevijano, M. Lourdes Laín Ara, M. Jesús Lalaguna Puértolas, M. Pilar Lalana Josa, Elisa Lambán Casamayor, Juan José Lasarte Velillas, M.ª Isabel Lostal Gracia, Rosa Magallón Botalla, Mónica Marco Olloqui, M. Pilar Marín Ibáñez, José Luis Martínez Bueno, Laura Martínez Espligares, José M. Mengual Gil, Isabel Moneo Hernández, Mercedes Montaner Cosa, Luis A. Moreno Aznar, Ana Isabel Muñoz Campos, Elena Muñoz Jalle, Eva María Navarro Serrano, Luis Carlos Pardos Martínez, José Antonio Pinilla Fuentes, Carmen Puig García, Pascual Puyuelo del Val, M. Victoria Redondo Cuerpo, Rafael Ruiz Pastora, Pilar Samper Villagrasa, Javier Sánchez Gimeno, Asunción Sánchez Zapater, M. Flor Sebastián Bonel, M. Teresa Solans Bascuas, Jiménez, M. Carmen Viñas Viamonte, Gregorio Zarazaga Germes.
Please cite this article as: Oves Suárez B, Escartín Madurga L, Samper Villagrasa MP, Cuadrón Andrés L, Álvarez Sauras ML, Lasarte Velillas JJ, et al. Inmigración y factores asociados con la lactancia materna. Estudio CALINA. An Pediatr (Barc). 2014;81:32–38.
The names of the members of the Grupo Colaborativo CALINA (CALINA Collaborative Group) are listed in Appendix 1.