Cardio-respiratory arrest (CPA) is infrequent in children, but it can occur in any place and at any time. This fact means that every health care facility must always have the staff and material ready to resuscitate a child. These recommendations are the consensus of experts of the Spanish Paediatric and Neonatal Resuscitation Group on the material and medication for paediatric and neonatal resuscitation and their distribution and use.
CPR trolleys and backpacks must include the essential material to quickly and efficiently perform a paediatric CPR. At least one CPR trolley must be available in every Primary Care facility, Paediatric Intensive Care Unit, Emergency Department, and Pre-hospital Emergency Areas, as well as in paediatric wards, paediatric ambulatory areas, and radiology suites. This trolley must be easily accessible and exclusively include the essential items to perform a CPR and to assist children (from newborns to adolescents) who present with a life-threatening event. Such material must be familiar to all healthcare staff and also include the needed spare parts, as well as enough drug doses. It must also be re-checked periodically.
The standardisation and unification of the material and medication of paediatric CPR carts, trolleys, and backpacks, as well as the training of the personnel in their use are an essential part of the paediatric CPR.
La parada cardiorrespiratoria (PCR) se puede presentar en cualquier lugar y en cualquier momento y por ello todos los centros sanitarios y los servicios de urgencias extrahospitalarias deben disponer de personal y material adecuado para realizar una reanimación cardiopulmonar (RCP). Estas recomendaciones son el consenso de expertos del Grupo Español de Reanimación Cardiopulmonar Pediátrica y Neonatal sobre el material y medicación de RCP pediátrica y neonatal y su distribución y utilización.
Los carros y mochilas de RCP deben tener el material y la medicación para llevar a cabo de forma rápida y eficiente una RCP pediátrica. Debe existir al menos un carro de RCP accesible en cada centro de atención primaria, unidad de cuidados intensivos pediátricos, unidad de cuidados intensivos neonatales, servicio de urgencias, servicio de urgencias extrahospitalarias, planta de pediatría, área de consultas y zona de radiología. El carro de RCP debe contener solo el material y la medicación imprescindibles para realizar una RCP y atender a las urgencias vitales. El material debe ser conocido por el personal, incluir los repuestos necesarios y ser revisado y repuesto periódicamente.
La estandarización y unificación del contenido (material y medicación) de los carros y mochilas de RCP pediátrica, así como el entrenamiento del personal en su utilización, son una parte esencial de la organización asistencial de la RCP pediátrica.
Cardiopulmonary arrest (CPA) in children, and thus the need to perform paediatric cardiopulmonary resuscitation (CPR), may arise anywhere, in or out of the hospital. The same is true of life-threatening emergencies, where immediate intervention can prevent CPA. On the other hand, errors involving equipment and medication during CPR are not infrequent and may have significant repercussions.1 For this reason, all health care settings—be they hospitals, primary care centres or out-of-hospital urgent care and transport services—must be prepared to identify children whose life is immediately at risk in order to perform paediatric CPR and manage other life-threatening emergencies. For this to happen, the necessary material resources must be available, and health care professionals must know how to use them appropriately.
The so-called resuscitation and emergency trolleys or backpacks are an essential health care resource both in health care facilities and emergency ambulances, although the contents that need to be stocked vary depending on the setting and the expected type of CPR.2,3
However, few studies have investigated this topic, and there are no international recommendations on the equipment and medication that should be included in resuscitation trolleys, the way the trolley should be organised, or how to train health care staff on their contents and appropriate use.4
A few basic principles must be taken into account to choose the materials to be included in a resuscitation trolley:
- -
It should only contain equipment and medication required for CPR and management of life-threatening emergencies, and its contents should only be used for these purposes.
- -
It should include materials suitable for children of all ages and sizes.
- -
It should be organised so that equipment and medication can be found easily and intuitively.
We proceed to present the recommendations on the equipment and medication for CPR made by an expert group selected by the Spanish Group on Paediatric and Neonatal CPR.
Contents of cardiopulmonary resuscitation trolleys and backpacksWe now describe the contents recommended for 3 types of CPR trolleys used in neonatal and paediatric care.
- 1.
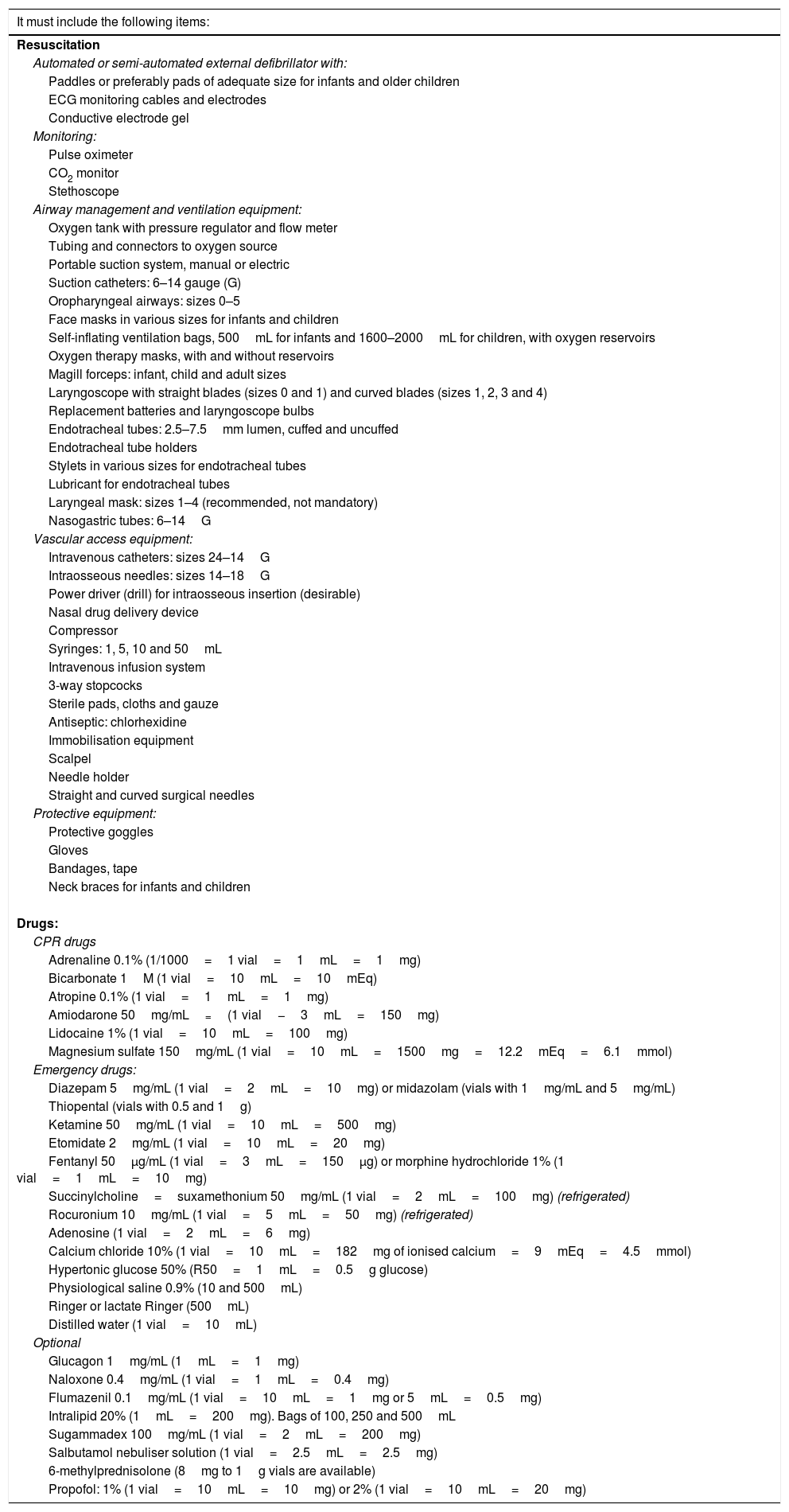
The intermediate life support paediatric resuscitation trolley, suitable for primary care clinics, after-hours care facilities, paediatric wards, paediatric outpatient clinics and radiology suites in hospitals that have a paediatric intensive care unit (PICU), as well as emergency departments in hospitals that do not usually manage children but may occasionally receive paediatric patients with CPA or life-threatening emergencies (Table 1).
Table 1.Intermediate life support paediatric resuscitation trolley.
It must include the following items: Resuscitation Automated or semi-automated external defibrillator with: Paddles or preferably pads of adequate size for infants and older children ECG monitoring cables and electrodes Conductive electrode gel Monitoring: Pulse oximeter CO2 monitor Stethoscope Airway management and ventilation equipment: Oxygen tank with pressure regulator and flow meter Tubing and connectors to oxygen source Portable suction system, manual or electric Suction catheters: 6–14 gauge (G) Oropharyngeal airways: sizes 0–5 Face masks in various sizes for infants and children Self-inflating ventilation bags, 500mL for infants and 1600–2000mL for children, with oxygen reservoirs Oxygen therapy masks, with and without reservoirs Magill forceps: infant, child and adult sizes Laryngoscope with straight blades (sizes 0 and 1) and curved blades (sizes 1, 2, 3 and 4) Replacement batteries and laryngoscope bulbs Endotracheal tubes: 2.5–7.5mm lumen, cuffed and uncuffed Endotracheal tube holders Stylets in various sizes for endotracheal tubes Lubricant for endotracheal tubes Laryngeal mask: sizes 1–4 (recommended, not mandatory) Nasogastric tubes: 6–14G Vascular access equipment: Intravenous catheters: sizes 24–14G Intraosseous needles: sizes 14–18G Power driver (drill) for intraosseous insertion (desirable) Nasal drug delivery device Compressor Syringes: 1, 5, 10 and 50mL Intravenous infusion system 3-way stopcocks Sterile pads, cloths and gauze Antiseptic: chlorhexidine Immobilisation equipment Scalpel Needle holder Straight and curved surgical needles Protective equipment: Protective goggles Gloves Bandages, tape Neck braces for infants and children Drugs: CPR drugs Adrenaline 0.1% (1/1000=1 vial=1mL=1mg) Bicarbonate 1M (1 vial=10mL=10mEq) Atropine 0.1% (1 vial=1mL=1mg) Amiodarone 50mg/mL=(1 vial−3mL=150mg) Lidocaine 1% (1 vial=10mL=100mg) Magnesium sulfate 150mg/mL (1 vial=10mL=1500mg=12.2mEq=6.1mmol) Emergency drugs: Diazepam 5mg/mL (1 vial=2mL=10mg) or midazolam (vials with 1mg/mL and 5mg/mL) Thiopental (vials with 0.5 and 1g) Ketamine 50mg/mL (1 vial=10mL=500mg) Etomidate 2mg/mL (1 vial=10mL=20mg) Fentanyl 50μg/mL (1 vial=3mL=150μg) or morphine hydrochloride 1% (1 vial=1mL=10mg) Succinylcholine=suxamethonium 50mg/mL (1 vial=2mL=100mg) (refrigerated) Rocuronium 10mg/mL (1 vial=5mL=50mg) (refrigerated) Adenosine (1 vial=2mL=6mg) Calcium chloride 10% (1 vial=10mL=182mg of ionised calcium=9mEq=4.5mmol) Hypertonic glucose 50% (R50=1mL=0.5g glucose) Physiological saline 0.9% (10 and 500mL) Ringer or lactate Ringer (500mL) Distilled water (1 vial=10mL) Optional Glucagon 1mg/mL (1mL=1mg) Naloxone 0.4mg/mL (1 vial=1mL=0.4mg) Flumazenil 0.1mg/mL (1 vial=10mL=1mg or 5mL=0.5mg) Intralipid 20% (1mL=200mg). Bags of 100, 250 and 500mL Sugammadex 100mg/mL (1 vial=2mL=200mg) Salbutamol nebuliser solution (1 vial=2.5mL=2.5mg) 6-methylprednisolone (8mg to 1g vials are available) Propofol: 1% (1 vial=10mL=10mg) or 2% (1 vial=10mL=20mg) Intubation equipment and drugs may be optional in some intermediate CPR trolleys.
- 2.
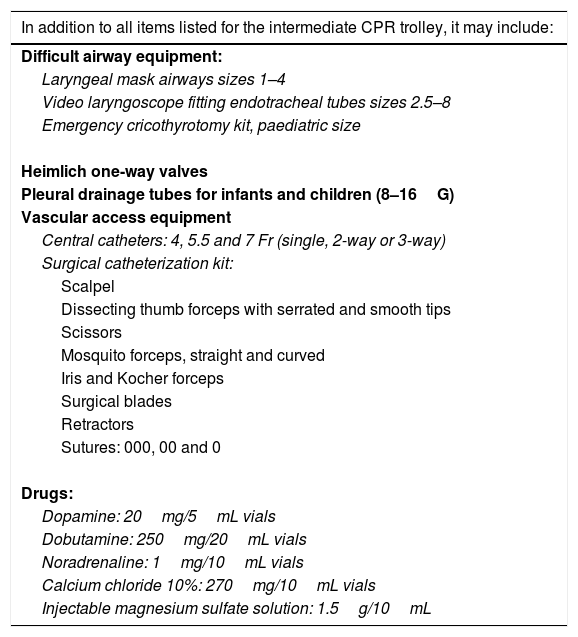
The advanced life support trolley, suitable for PICUs, adult ICUs in hospitals without a PICU, emergency departments of hospitals with a PICU, paediatric resuscitation bays and operating theatres, and pre-hospital emergency care settings. In addition to all the materials listed for the intermediate CPR trolley, it can include the materials listed in Table 2.
Table 2.Advanced paediatric CPR trolley or backpack.
In addition to all items listed for the intermediate CPR trolley, it may include: Difficult airway equipment: Laryngeal mask airways sizes 1–4 Video laryngoscope fitting endotracheal tubes sizes 2.5–8 Emergency cricothyrotomy kit, paediatric size Heimlich one-way valves Pleural drainage tubes for infants and children (8–16G) Vascular access equipment Central catheters: 4, 5.5 and 7 Fr (single, 2-way or 3-way) Surgical catheterization kit: Scalpel Dissecting thumb forceps with serrated and smooth tips Scissors Mosquito forceps, straight and curved Iris and Kocher forceps Surgical blades Retractors Sutures: 000, 00 and 0 Drugs: Dopamine: 20mg/5mL vials Dobutamine: 250mg/20mL vials Noradrenaline: 1mg/10mL vials Calcium chloride 10%: 270mg/10mL vials Injectable magnesium sulfate solution: 1.5g/10mL The CPR backpack should contain the same equipment and medication as the advanced CPR trolley, even if there are fewer units of each item.
- 3.
The neonatal resuscitation trolley, which must be available in delivery rooms, neonatal intensive care units, neonatal units and emergency ambulances and transport services5–7 (Table 3).
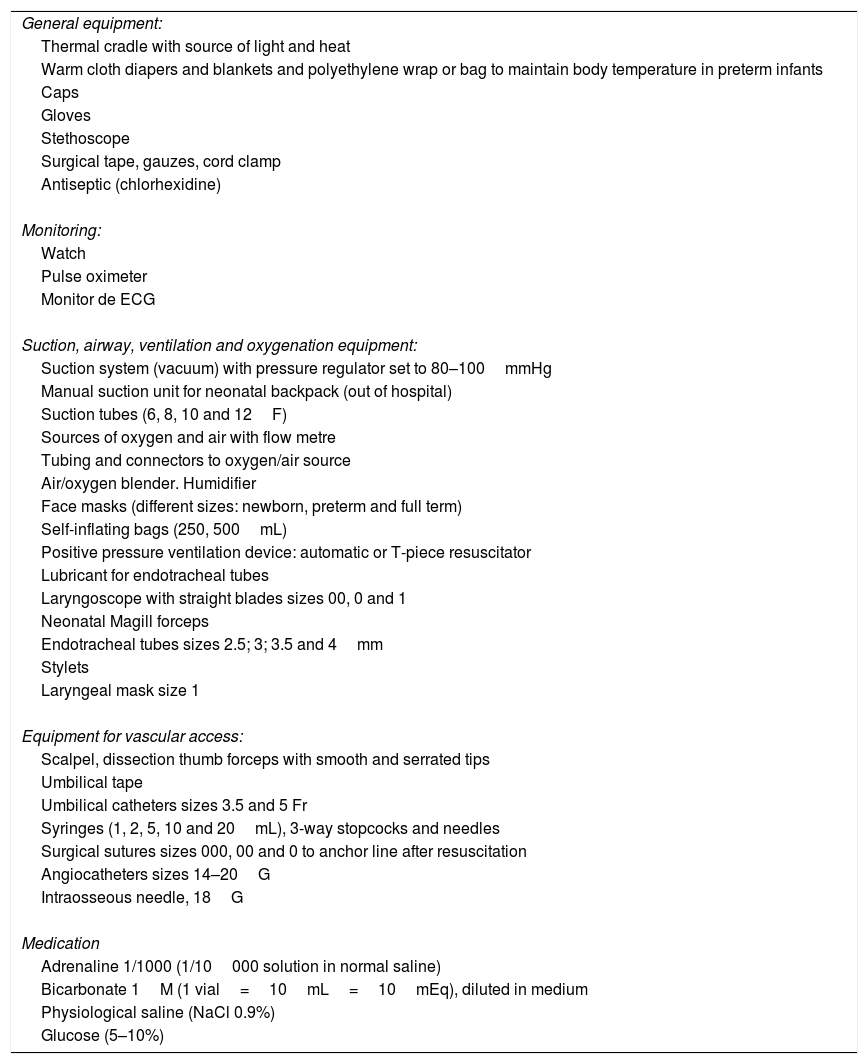
Table 3.Neonatal resuscitation trolley.
General equipment: Thermal cradle with source of light and heat Warm cloth diapers and blankets and polyethylene wrap or bag to maintain body temperature in preterm infants Caps Gloves Stethoscope Surgical tape, gauzes, cord clamp Antiseptic (chlorhexidine) Monitoring: Watch Pulse oximeter Monitor de ECG Suction, airway, ventilation and oxygenation equipment: Suction system (vacuum) with pressure regulator set to 80–100mmHg Manual suction unit for neonatal backpack (out of hospital) Suction tubes (6, 8, 10 and 12F) Sources of oxygen and air with flow metre Tubing and connectors to oxygen/air source Air/oxygen blender. Humidifier Face masks (different sizes: newborn, preterm and full term) Self-inflating bags (250, 500mL) Positive pressure ventilation device: automatic or T-piece resuscitator Lubricant for endotracheal tubes Laryngoscope with straight blades sizes 00, 0 and 1 Neonatal Magill forceps Endotracheal tubes sizes 2.5; 3; 3.5 and 4mm Stylets Laryngeal mask size 1 Equipment for vascular access: Scalpel, dissection thumb forceps with smooth and serrated tips Umbilical tape Umbilical catheters sizes 3.5 and 5 Fr Syringes (1, 2, 5, 10 and 20mL), 3-way stopcocks and needles Surgical sutures sizes 000, 00 and 0 to anchor line after resuscitation Angiocatheters sizes 14–20G Intraosseous needle, 18G Medication Adrenaline 1/1000 (1/10000 solution in normal saline) Bicarbonate 1M (1 vial=10mL=10mEq), diluted in medium Physiological saline (NaCl 0.9%) Glucose (5–10%)
The recommendations for the use of the resuscitation trolley or backpack are the following:
Type of trolley or backpackTrolley: the trolley must be easy to move and have clearly visible drawers and labels.
Backpack: it must be easy to carry and contain separate spaces where materials can be arranged in an organised manner.
Location of the trolleyIt is essential for trolleys or backpacks to be stored in an easily accessible and identifiable place. Their location should be marked in some way, and they should not be concealed or blocked by any other equipment.
ContentsA cardiac arrest trolley must only include the materials required for CPR and life-threatening emergencies. Overstocking can hinder access to the materials that are actually needed to manage an emergency.
All materials should be available in the sizes needed to treat children of any age.
Supplies for each device and medications should be stocked in the amounts that may be required during resuscitation. Time must not be wasted going to the storage room or pharmacy to obtain the missing items.
Each trolley and backpack should have a list with all the included equipment and medication, which can also serve as a checklist.8
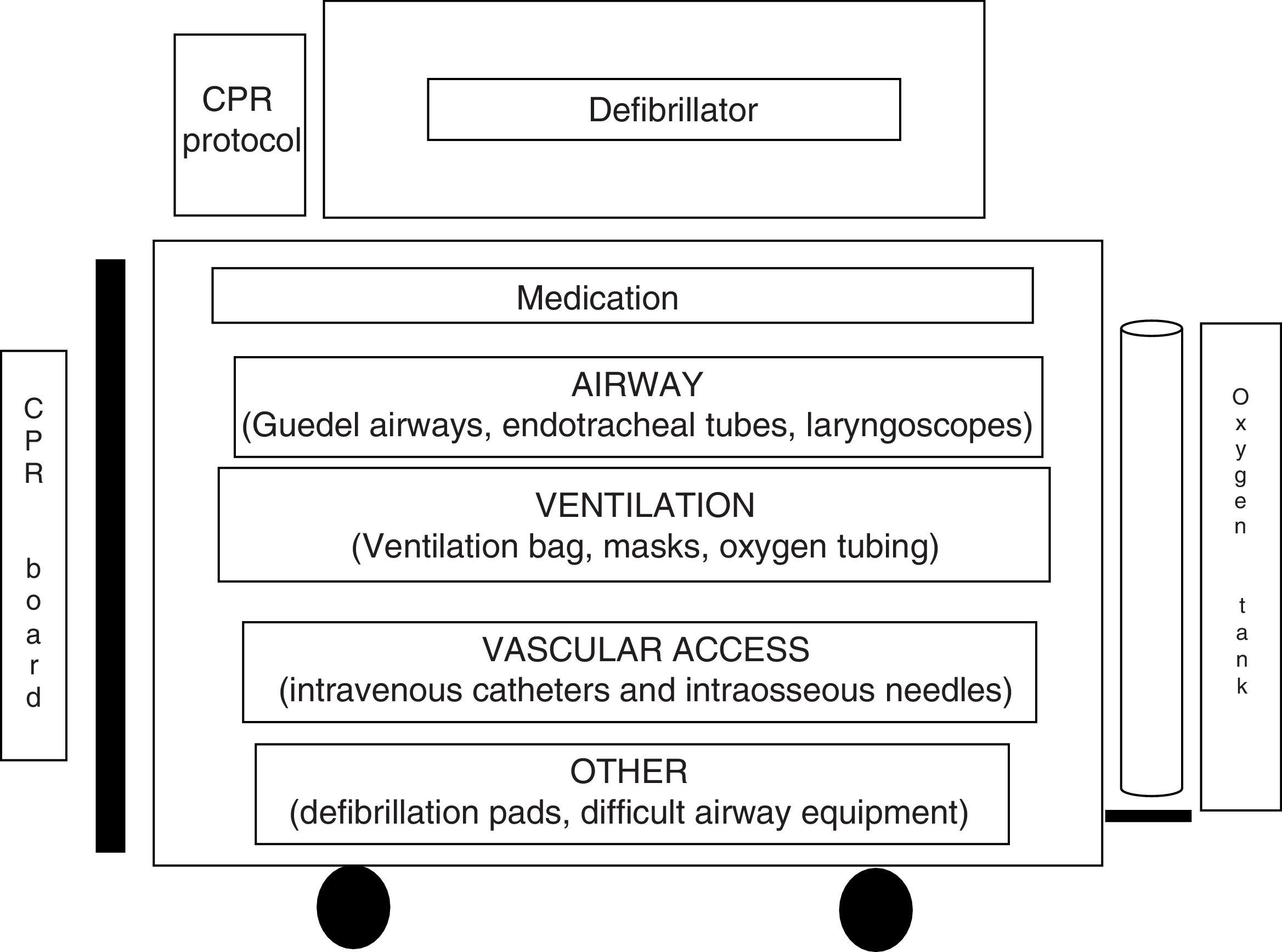
Distribution of contentsThe equipment and medication must always be organised and visible at first glance.
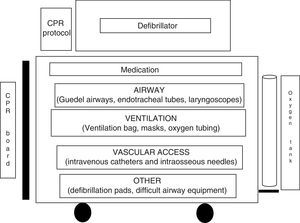
We recommend organising contents in drawers according to a colour-coding system or following the ABC sequence: A (airway), B (breathing) and C (circulation).9–12
Fig. 1 shows an example of how to distribute trolley contents in the top and side trays and the different drawers.
Medications must be sealed and bear the manufacture and expiration dates.
All physicians, nurses and health care technicians must know which equipment and medications are stocked as well as their location in the trolley.2,11,12
Checking trolley contentsA protocol must be established for checking the equipment and medications at regular intervals, assigning specific staff this responsibility, and there must be a checklist for testing the equipment and restocking materials. The equipment and medications must always be reviewed after performance of CPR.
The contents of the trolley should never be used for anything other than CPR and life-threatening emergencies.
Staff trainingAll physicians, nurses and health care technicians must be trained and updated periodically not only on paediatric and neonatal CPR techniques, but also on the equipment and drugs included the trolley and their use during CPR.
Dosage sheetsIt is recommended that the following be placed in a highly visible location with the resuscitation trolley:
- -
A sheet with the size of each equipment item and dosage of each medication recommended for each age and weight in children.
- -
A checklist of all the equipment and medication included in the trolley.
- -
A sheet or poster with the paediatric CPR algorithm (intermediate or advanced, as applicable).
The authors have no conflicts of interest to declare.
Please cite this article as: López-Herce Cid J, Rodríguez Núñez A, Carrillo Álvarez Á, Zeballos Sarrato G, Martínez Fernández-Llamazares C, Calvo Macías C, et al. Recomendaciones de expertos sobre el material del carro y mochila de reanimación cardiopulmonar pediátrica y neonatal. An Pediatr (Barc). 2018;88:173.