To validate the content and adequacy of the «Rescube» training material that includes adapted information from the chain of survival.
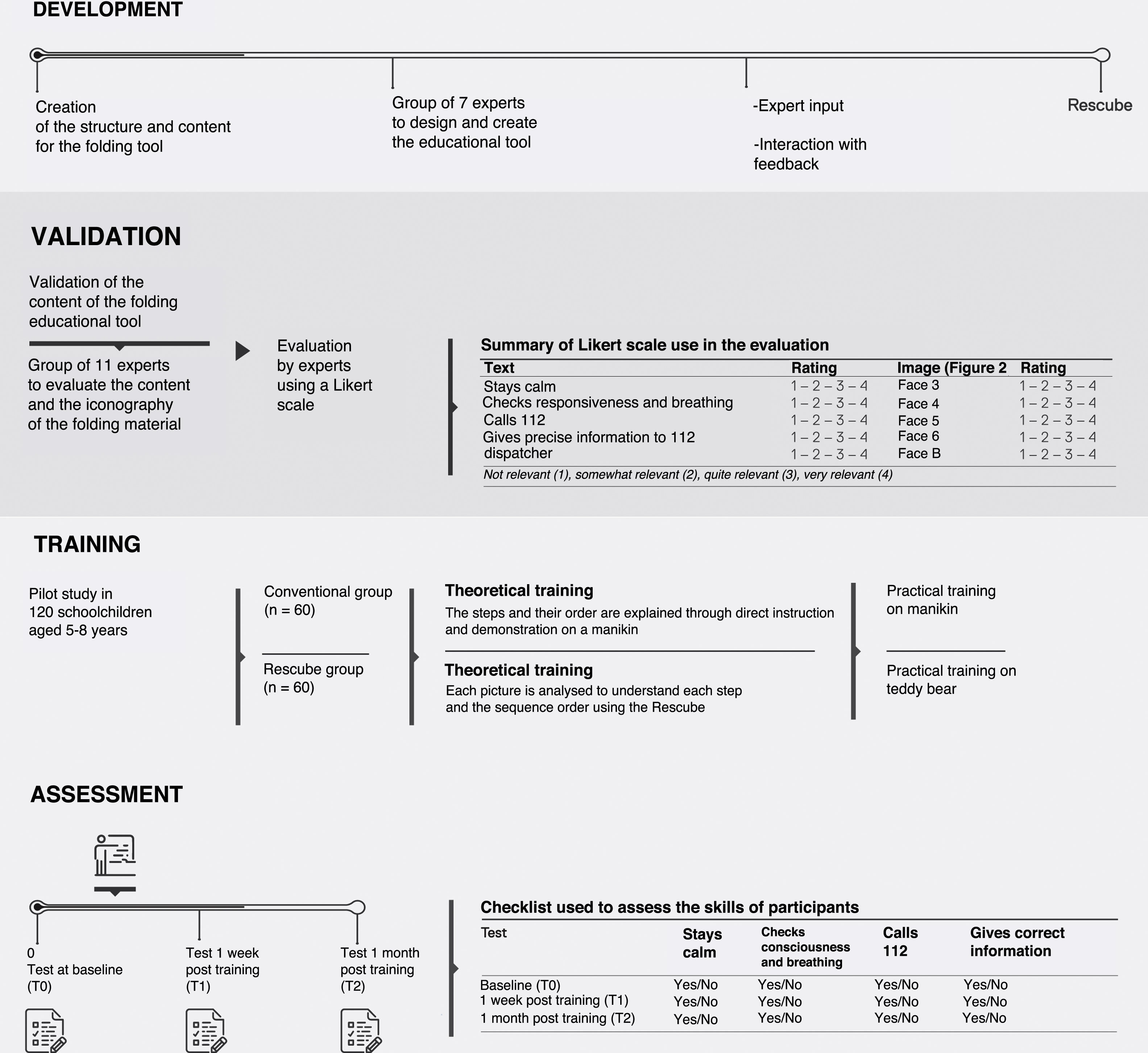
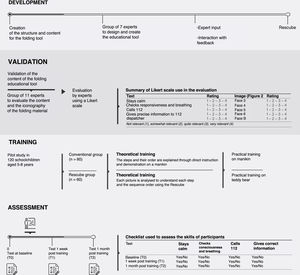
Material and methodsThe study included three steps: (i) material development by 7 experts, following Delphi method; (ii) assessment of training material by 11 experts by means of a Likert score and calculation of content validity; and (iii) pilot study in two groups of 5–8 years-old: Rescube group (GR; n=60) and Traditional group (GT; n=60). GR was trained with Rescube and a Teddy bear, while GT was traditionally trained with a pediatric manikin. Participants were individually assessed at baseline, and one week and one month after training.
ResultsAll content validity indexes calculated are above the recommended cut-off for analysis with more than 9 experts (≥0,80). Children’s learning results were positive, with percentages equal or higher than 80% in all registered variables at the first (one week) evaluation and equal or higher than 67% when evaluated one month after training. No significant differences were detected between groups.
ConclusionThe Rescube training tool based on infantile pictures is valid and useful to train young schoolchildren in the chain of survival.
Validar el contenido y la adecuación del material desplegable «Rescube» con la información adaptada de la «cadena de supervivencia».
Material y métodosLa investigación fue realizada en tres etapas: 1) Desarrollo del material desplegable por 7 profesionales, utilizando los pasos de un método Delphi; 2) Evaluación del material desplegable por 11 expertos mediante una escala Likert y posterior cálculo de índices de validez de contenido, y 3) estudio piloto en dos grupos de niños entre 5 y 8 años: grupo Rescube (GR; n=60) y grupo Tradicional (GT; n=60). El GR recibió la formación con el Rescube y un peluche mientras que en el GT se utilizó un maniquí pediátrico. Los participantes fueron evaluados individualmente antes de la formación, y una semana y un mes después.
ResultadosTodos los índices calculados de validez de contenido superan el punto de corte aconsejado para los análisis con más de 9 expertos (≥0,80). Los resultados de aprendizaje de los niños fueron positivos, observándose porcentajes iguales o superiores al 80% en todas las variables registradas tras una semana e iguales o superiores al 67% tras un mes. No se observaron diferencias significativas entre los grupos.
ConclusiónLa herramienta docente basada en imágenes infantiles en un cubo desplegable Rescube es válida y útil para formar a los escolares más jóvenes en la «cadena de supervivencia».
Out-of-hospital cardiac arrest (OHCA) is the third leading cause of death in developed countries and a public health problem that needs to be addressed through surveillance, intervention and research.1 Immediate delivery of basic life support (BLS) by bystanders is one of the main factors that affect survival following OHCA.2 However, delivery of BLS by bystanders is generally infrequent, which has led to the development of strategies for training children and youth in BLS in the school setting, with some countries, such as Denmark, showing promising results.3
The guidelines of the European Resuscitation Council (ERC) have been recommending inclusion of BLS in the school curriculum since 1992.4,5 In Spain, school-based training in BLS and first aid is regulated by the Law on Education, although its implementation has been far from successful.6
The Kids Save Lives initiative, endorse by the ERC and the World Health Organization (WHO), seeks to promote BLS education worldwide and recommends training of children and adolescents (at least from age 12 years).7 Despite the potential physical limitations of younger children in delivering quality basic cardiopulmonary resuscitation (CPR),8,9 there is evidence that they can recognise victims of cardiac arrest and alert emergency services.9,10 Thus, from a very young age, children are capable of performing the first step to activate the “chain of survival” and contribute to saving lives,11 and therefore should be trained in pursuit of this objective.12
Since there is still no conclusive evidence on which educational strategies are most suitable, the BLS education section of the ERC proposes researching innovative educational strategies.5 Departing from the classic formats conceived for adult education and including appealing images and educational materials adapted to children could facilitate school-based learning, providing a resource for teachers that could be added to all other educational materials. Thus, the objective of this research project was the develop and validate a visual educational tool for children to help identify OHCA and based on the “chain of survival”.
Material and methodsDesignThe study was carried out in 3 phases:
- 1)
Development of a foldable educational tool by a group of professionals.
- 2)
Testing of the foldable tool by a group of experts by means of a Likert scale.
- 3)
Pilot study in 120 schoolchildren, with 1 experimental and 1 control group (Fig. 1). The study adhered to the principles of the Declaration of Helsinki and was approved by the Ethics Committee of the School of Education and Sports Science of the Universidad de Vigo, Spain (code 14-2802-18).
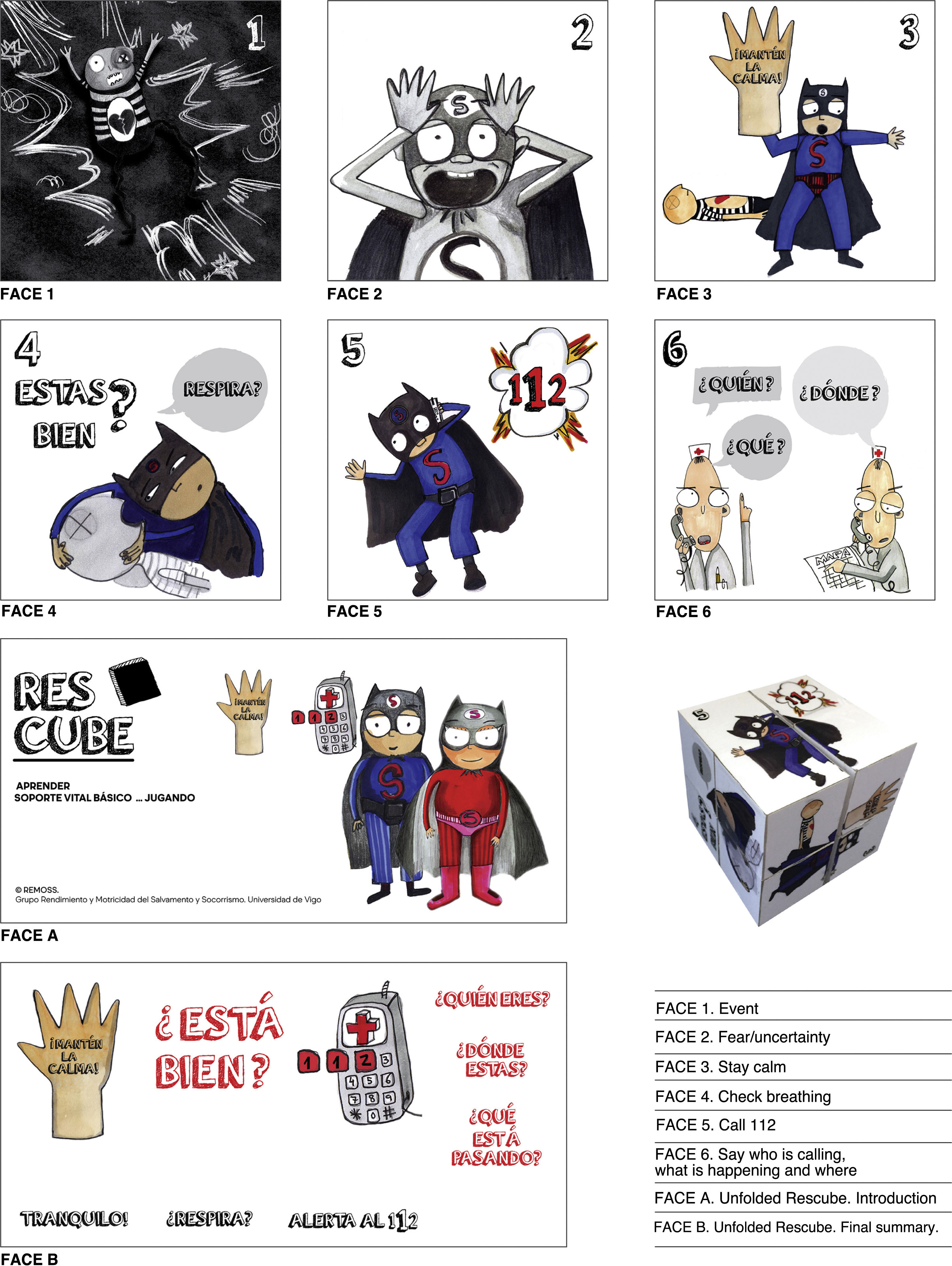
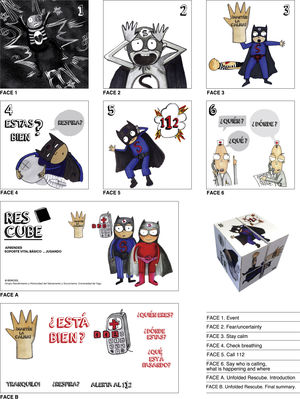
A team of 7 professionals in the fields of education, art, paediatrics and nursing worked together to design the learning aid for use in the school setting, which was based on character drawings. The content was developed taking into account international CPR guidelines and based on the links of the “chain of survival”.11 The development process followed the Delphi method, which is a systematic approach to obtain expert opinions with 4 key characteristics: expert input, interaction with feedback, statistical group responses and confidentiality.13,14 In the study presented here, we used the first 2, and defined the experts as “specialists in their fields” and “individuals with experience in BLS education”. The resulting tool was a folding picture cube with 6 faces that can completely unfold into 2 rectangular mini-posters (Fig. 2).
Content testing and validation procedureAfter the initial design was completed, we sent the Rescube to 11 experts, none of which had participated in the development of the tool or of the study. The inclusion criteria were: (a) to be an active professional in education or health; (b) to have experience in teaching first aid and (c) to be a professor in the field of medicine, nursing or sports science at the college level. The content of each item and the suitability of each of the associated illustrations were assessed by means of a Likert scale with 4 answer options (not relevant, somewhat relevant, quite relevant, very relevant) (Fig. 1), as was done in a previous study.15 We followed the recommendations of Yusoff for the validation process.16
Pilot studyAfter validating the contents of the cube, we carried out a pilot study in 120 schoolchildren aged 5–8 years. The study had a quasi-experimental design with block randomization and a control group aimed at assessing learning and long-term retention in 2 groups of 60 children each: the experimental group (RG) was trained with the Rescube folding cube, while the control group (CG) was trained with a conventional training programme specific for children.17,18
We obtained informed consent from the parents or legal guardians of participants and from the school. The inclusion criteria were the following: (a) obtention of informed consent from parent/legal guardian; (b) lack of previous knowledge of BLS and C) absence of physical or cognitive impairment.
As described in previous studies conducted in schoolchildren,19,20 the intervention consisted of 3 tests for assessment of practical skills (T0), learning (T1) and long-term assimilation of learned contents/skills (T2).
Educational programmeTaking into account the cognitive development and attention span of children in this age group, the training had a duration of 15minutes with a 1:5 teacher-to-student ratio. A training protocol was developed so that the same information would be delivered to every group, focused on the first step of the “chain of survival” (recognition of cardiac arrest and activation of emergency response system). The training followed the sequence explanation-demonstration-practice.
In the CG, the explanation part consisted of direct instruction by the teacher using the manikin, after which children practiced on the same manikin. In the RG, the explanation part involved going over each of the illustrations in the Rescube (Fig. 2) with a guided discovery approach (to engage students mentally), after which children practiced on the teddy bear.
Testing: materials, directions and timeline- •
Materials. In the CG, practical skills were tested using a paediatric manikin (Prestan® professional child manikin, Ohio, USA) and a toy cell phone. The materials used in the RG were the Rescube, a large teddy bear and a toy cell phone.
- •
Directions. For every test, children were given the same directions (previously tested in another pilot sample to ensure comprehension) by the same individual (a teacher in the school, trained in first aid and with experience in experimental research): “Imagine that you find someone laying on the ground like this manikin/teddy bear, and does not seem to be moving or breathing. What would you do?”
- •
Testing timeline. T0 was administered before the training, T1 a week after the training and T2 one month after the training.
Each participant was assessed individually under the supervision of an expert using a checklist that included each of the variables with a dichotomous yes/no answer format (Fig. 1).
Statistical analysisWe performed the statistical analysis with the software IBM SPSS Statistics version 20 for Windows.
To calculate content validity indices, we followed the recommendations published by Yussof.16 First we dichotomised the evaluation data, transforming “very relevant” and “quite relevant” choices in the Likert scale to “1” and the “somewhat relevant” and “not relevant” choices as “0”.21 Afterward, for each item, we counted the number of experts that agreed with the content and the images, and we documented the items for which the experts reached full consensus. With the resulting data, we calculated the following indices for the written content and images of the folding cube:
- •
Item-level content validity index (I-CVI): proportion of experts that considered the item relevant out of the total experts.
- •
Scale-level content validity index (S-CVI): the proportion of all items considered relevant out of all items in the instrument.
- •
Scale-level content validity index based on the universal agreement (S-CVI/UA): proportion of items considered relevant by all experts.
The CVI values considered acceptable when more than 9 experts are evaluating an item or instrument are those of .78 or greater.22
We expressed demographic variables (sex and age) by means of absolute and relative frequencies. To assess learning in participants, we first described the variables under study as relative frequencies. We calculated frequencies for each group under study (Rescube vs conventional) and for each of the administered tests (T0, T1 and T2). We also graphed the assessment data by study group, time point and age group (5–6 years and 7–8 years). Subsequently, we compared the distributions of each study group at different time points. We did the same for each age group. To compare results at different time points we used the McNemar test for paired data. To compare the results in different groups we used the chi square test if the conditions for its application were met (at least 80% of the expected counts in the contingency table equal to or greater than 5) and otherwise the Fisher exact test. We measured the effect size (ES) by means of Cramer’s V. For all tests, we defined statistical significance as a p-value of .05 or less.
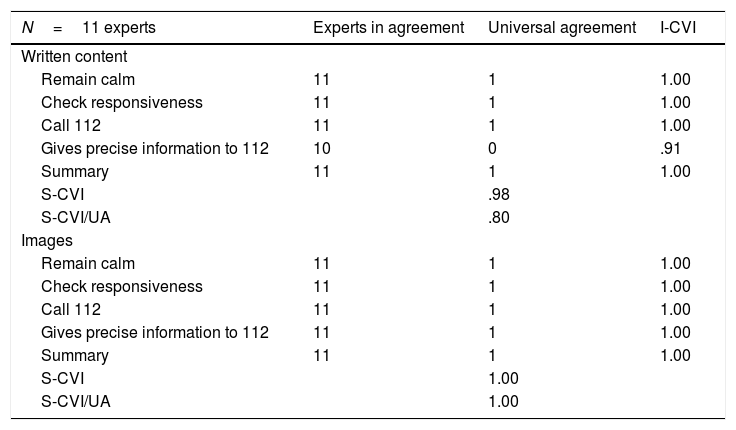
ResultsValidation of the RescubeTable 1 presents the obtained content validity indices. All experts agreed that the items were very relevant with one exception. One of the experts considered that the item referring to the step “gives precise information to 112” was not relevant, which resulted in an I-CVI of .91. There was universal agreement in the remaining content and pictographic items, resulting in I-CVIs of 1.00.
Content validity index values.
| N=11 experts | Experts in agreement | Universal agreement | I-CVI |
|---|---|---|---|
| Written content | |||
| Remain calm | 11 | 1 | 1.00 |
| Check responsiveness | 11 | 1 | 1.00 |
| Call 112 | 11 | 1 | 1.00 |
| Gives precise information to 112 | 10 | 0 | .91 |
| Summary | 11 | 1 | 1.00 |
| S-CVI | .98 | ||
| S-CVI/UA | .80 | ||
| Images | |||
| Remain calm | 11 | 1 | 1.00 |
| Check responsiveness | 11 | 1 | 1.00 |
| Call 112 | 11 | 1 | 1.00 |
| Gives precise information to 112 | 11 | 1 | 1.00 |
| Summary | 11 | 1 | 1.00 |
| S-CVI | 1.00 | ||
| S-CVI/UA | 1.00 |
I-CVI, item-level content validity index; S-CVI, scale-level content validity index; S-CVI/UA, scale-level content validity index based on the universal agreement.
In the validation of the written content of the Rescube, we obtained a S-CVI of .98 and a S-CVI/UA of .80, while in the validation of the images we obtained a S-CVI and a S-CVI/UA of 1.00. All the values exceeded the threshold recommended by Lynn for more than 9 experts.22
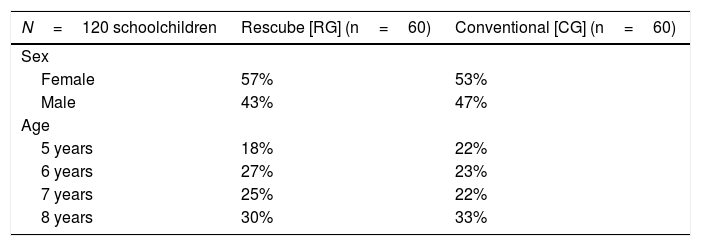
Pilot studyTable 2 presents the demographic characteristics of the participants. The age distribution was similar in the 2 groups.
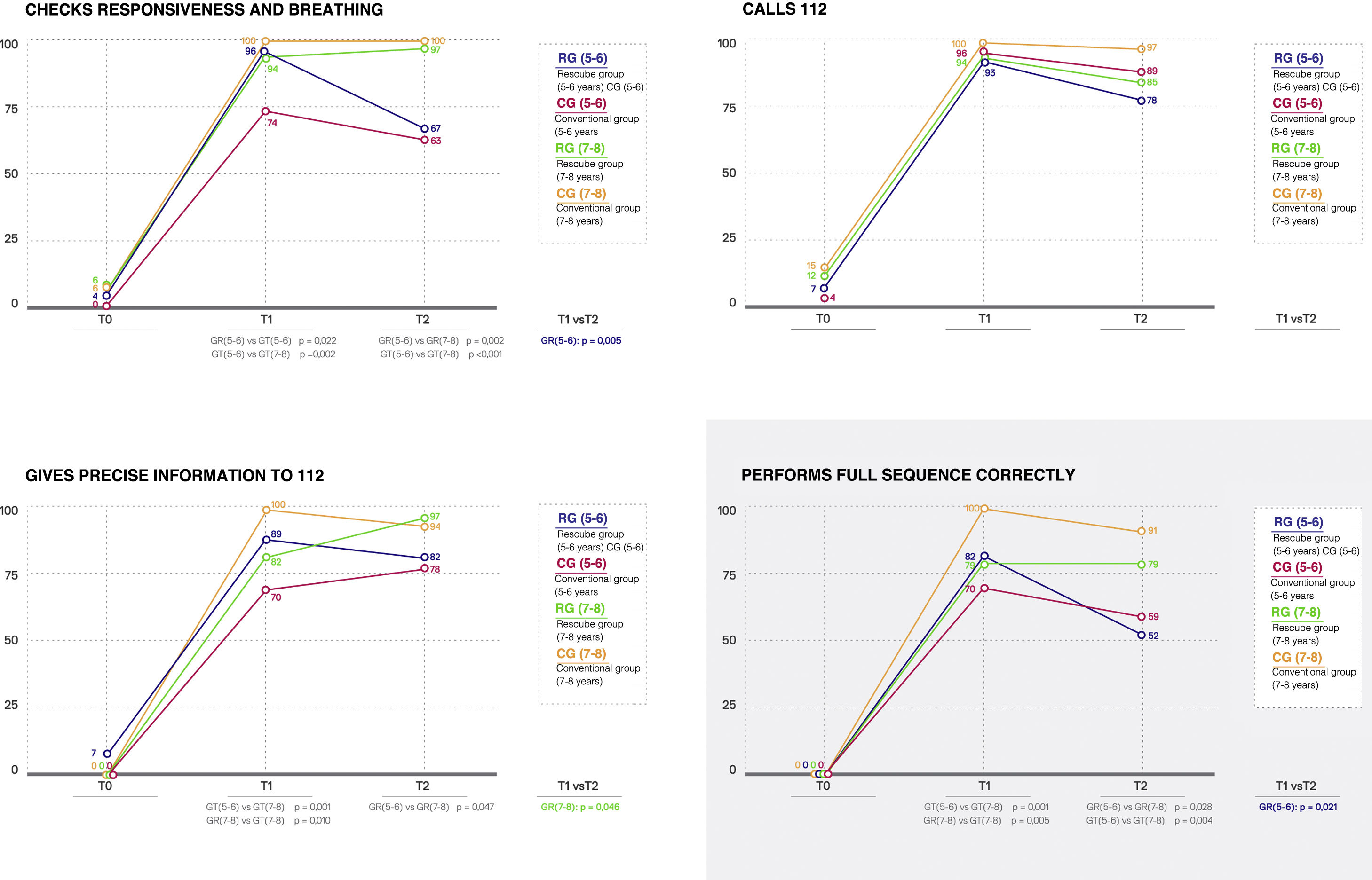
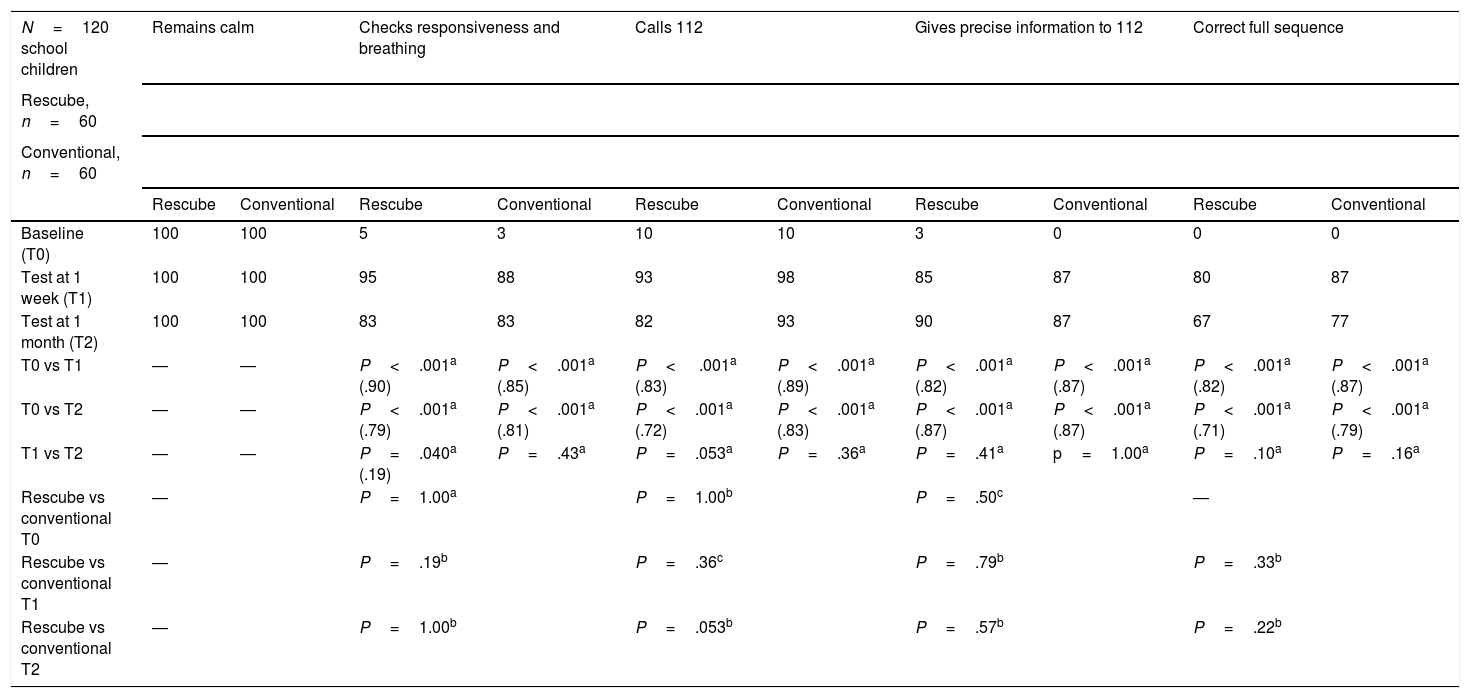
Table 3 presents the results concerning the assessment of the OHCA recognition and calling the emergency response team. We did not find statistically significant differences in any of the variables under study (P>.05). All participants remained calm during testing at all 3 time points. Both groups performed significantly better at 1 week (T1) and 1 month (T2) post training compared to baseline (T0) in every variable (P<.001; ES≥.71). A lower proportion in the RG checked the responsiveness and breathing (P=.040; ES=.19) in T2 (83%) compared to T1 (95%), a trend that did not occur on the CG, although the proportion of the CG that performed correctly in this item was somewhat lower compared to the RG at both time points (T1, 88%; T2, 83%; P=.43). When we compared the groups, we did not find significant differences between T1 and T2 in any of the variables under study:
- •
Calls 112: T1 (RG, 93%; CG, 98%); T2 (RG, 82%; CG, 93%).
- •
Gives precise information to 112: T1 (RG, 85%; CG, 87%); T2 (RG, 90%; CG, 87%).
- •
Correct full sequence: T1 (RG, 80%; CG, 87%); T2 (RG, 67%; CG, 77%).
Variables used to assess the sequence of recognition and call to emergency response system in participants in the pilot study.
| N=120 school children | Remains calm | Checks responsiveness and breathing | Calls 112 | Gives precise information to 112 | Correct full sequence | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Rescube, n=60 | ||||||||||
| Conventional, n=60 | ||||||||||
| Rescube | Conventional | Rescube | Conventional | Rescube | Conventional | Rescube | Conventional | Rescube | Conventional | |
| Baseline (T0) | 100 | 100 | 5 | 3 | 10 | 10 | 3 | 0 | 0 | 0 |
| Test at 1 week (T1) | 100 | 100 | 95 | 88 | 93 | 98 | 85 | 87 | 80 | 87 |
| Test at 1 month (T2) | 100 | 100 | 83 | 83 | 82 | 93 | 90 | 87 | 67 | 77 |
| T0 vs T1 | ― | ― | P<.001a (.90) | P<.001a (.85) | P< .001a (.83) | P<.001a (.89) | P<.001a (.82) | P<.001a (.87) | P<.001a (.82) | P<.001a (.87) |
| T0 vs T2 | ― | ― | P<.001a (.79) | P<.001a (.81) | P<.001a (.72) | P<.001a (.83) | P<.001a (.87) | P<.001a (.87) | P<.001a (.71) | P<.001a (.79) |
| T1 vs T2 | ― | ― | P=.040a (.19) | P=.43a | P=.053a | P=.36a | P=.41a | p=1.00a | P=.10a | P=.16a |
| Rescube vs conventional T0 | ― | P=1.00a | P=1.00b | P=.50c | ― | |||||
| Rescube vs conventional T1 | ― | P=.19b | P=.36c | P=.79b | P=.33b | |||||
| Rescube vs conventional T2 | ― | P=1.00b | P=.053b | P=.57b | P=.22b | |||||
In parentheses: effect size.
Results expressed as relative frequencies.
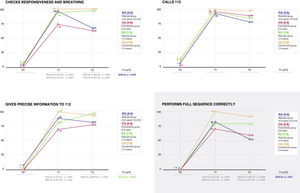
Fig. 3 presents the assessment results for the variables concerning the recognition of OHCA and the call to emergency services by age (5–6 years and 7–8 years). When we compared the participants in the RG based on age we did not find differences at 1 week (T1), although we did find improved results in the 7–8 years group at 1 month (T2) in the checking of responsiveness and breathing (P=.002), providing precise information to 112 (P=.047) and performing the full sequence correctly (P=.028). When we compared the participants in the CG, we found greater proportions of participants in the group aged 7–8 years that checked responsiveness and breathing and performed the full sequence correctly in both T1 and T2 (P≤.004). When we compared the subsets of participants aged 5–6 years in the RG versus the CG, we found a higher proportion that checked responsiveness and breathing in the 5–6 age group at T1 (P=.022), and found no differences at T2. In the group aged 7–8 years, a higher proportion of participants in the CG gave precise information to the 112 dispatcher (P=.010) and performed the full sequence correctly at T1 (P=.005), and there were no differences at T2.
DiscussionOur study validated the contents and appropriateness of the illustrations based on the chain of survival of the Rescube foldable educational tool for use in children aged 5–8 years and developed through a consensus process by professionals in the fields of paediatrics, nursing, education and art.23–25 The Rescube includes the items involved in the recognition of cardiac arrest and activating the emergency response system with their respective pictograms. Its design may be reminiscent of the Rubik cube, and meant for children to manipulate freely and use as a tool to support learning.
The ERC has been recommending school-based training in BLS for many years.4 In recent years, the Kids Save Lives initiative, also endorsed by the WHO, has sought to expand this objective worldwide with the hypothesis that if these skills are learned during the school years, there will be no need for specific training in adulthood and retention will improve, which will achieve an increase in the frequency of early initiation of CPR by bystanders.
The recognition of cardiac arrest and immediate notification to emergency services constitute the first link in the “chain of survival”, so its implementation is a key determinant of the outcome of OHCA.11 Several studies have shown that schoolchildren can learn these simple but essential concepts from an early age.10,17,26,27 Basic life support trainings should be brief5,17 and delivered by teachers, given their experience in education, their knowledge of children and the cost savings involved in this approach.17 Children aged 5–8 years do not have the physical capacity to deliver quality chest compressions, but they are able to understand the “chain of survival” and how to activate it.10,26,27 In teaching these steps, it is essential to use materials that are stimulating to schoolchildren (songs, dolls/stuffed animals, stories, etc).26,28 In the case of the Rescube, we believe that the use of pictograms as a learning tool is very appealing and has a positive effect that promotes learning and assimilation of BLS concepts.29
One of the drawbacks of BLS training programmes (whether for children or adults) is the poor retention of learned skills and contents, a problem that has yet to be resolved.9,12,20 In this regard, in our pilot study both groups exhibited good knowledge retention, with results that were comparable to those of other studies in children of similar age (5–7 years) and at least just as good as those in studies conducted in older children and adults.9,12,15
LimitationsThere are limitations to our study. We carried out the evaluations in the context of simulated scenarios, so we cannot be sure that individuals will act the same way in a real-life situation. Although calling 112 is easily done even from a phone that is not registered with a carrier or does not have a SIM card, the simulation was performed with a toy phone. Similarly, the evaluation was conducted using the training equipment. We did not assess the skills of participants in real situations or with real phones. This was a pilot study conducted in a specific sample, which precludes generalization of the results to the entire population of schoolchildren in the same age range, and further studies are required with more realistic simulations to confirm our results.
ConclusionRescube is a viable and valid educational tool that can facilitate learning the first link of the “chain of survival” by schoolchildren aged 5–8 years. It should be tested in a larger sample before recommending it as a tool to teach BLS to children in the school setting.
FundingThe study was funded by the Universidade de Vigo through the Educational Innovation Project “Diseño y desarrollo de un diccionario visual de Soporte Vital Básico para Educación Primaria” of the School of Education and Sports Science of Pontevedra in June 2016.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Otero-Agra M, Varela-Casal C, Castillo-Pereiro N, Casillas-Cabana M, San Román-Mata S, Barcala-Furelos R, et al. ¿Podemos enseñar la «cadena de supervivencia» jugando? Validación de la herramienta «Rescube». An Pediatr (Barc). 2021;94:213–222.