Intestinal epithelial dysplasia (IED) is a rare cause of untreatable diarrhoea.1 It usually has onset in the neonatal period with severe secretory diarrhoea resulting in irreversible intestinal failure and indefinite dependence on parenteral nutrition (PN). Although cases with a favourable outcome have been described,2 most of these patients depend on NP, so bowel transplantation is a treatment option that may help achieve enteral autonomy.3
We made a retrospective review of 3 patients with an epithelial dysplasia diagnosis. We analysed epidemiologic, clinical, diagnostic, treatment and outcome variables.
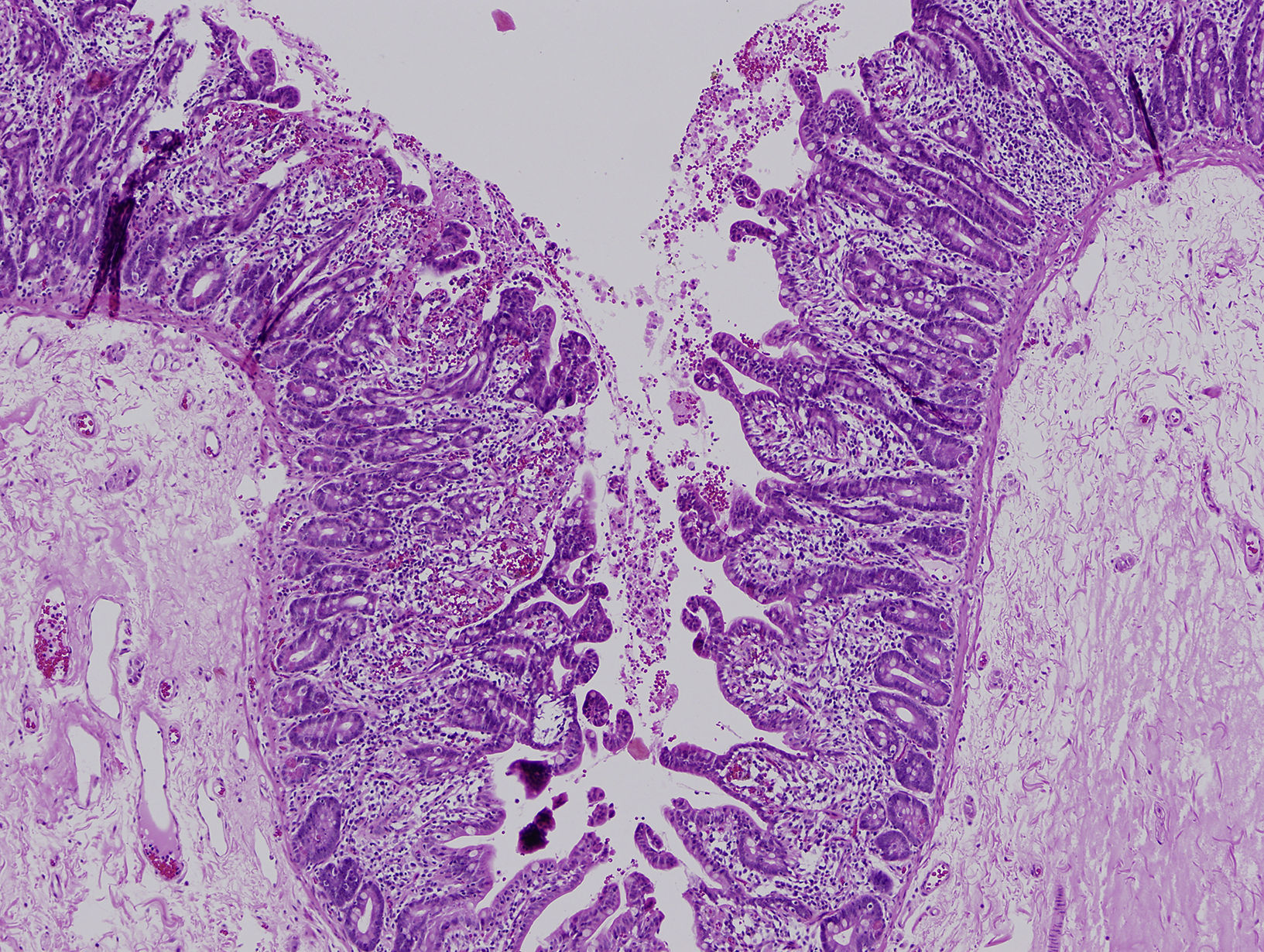
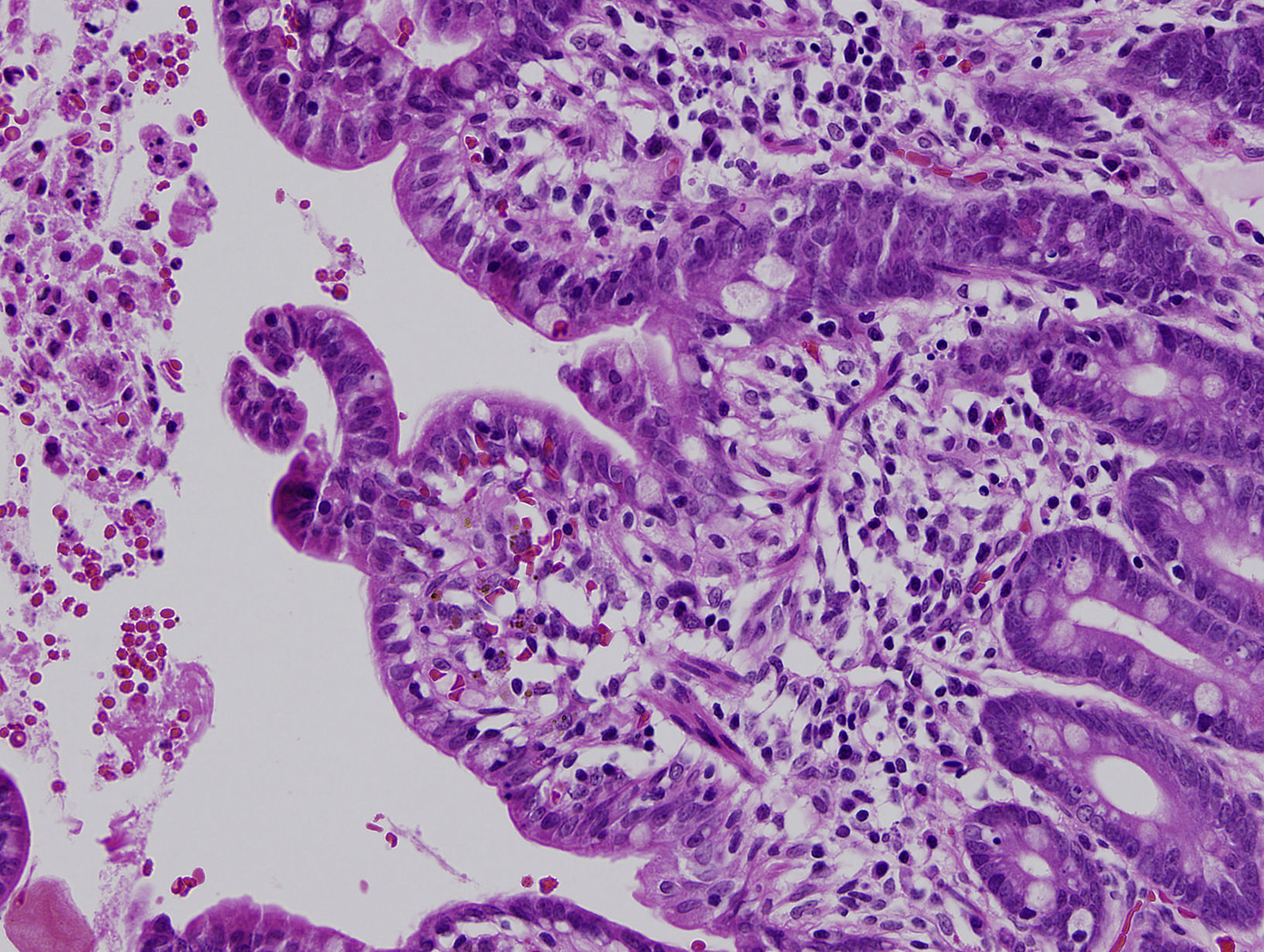
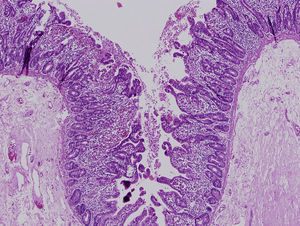
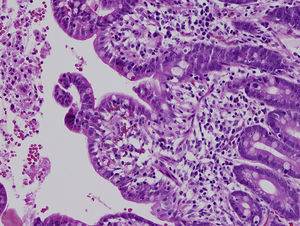
Secretory diarrhoea developed in the first month of life in all 3 patients. One patient was female and the other 2 were male. The former patient was of Ecuadorean descent and the other 2 were brothers of Moroccan descent born to consanguineous parents. All had been born to term and had adequate birth weights. The prenatal ultrasound examinations had been normal. None of the patients presented with atresia or punctuated keratitis. The immunological study was unremarkable. Histological examination of the intestinal mucosa revealed villous shortening and focal crowding of enterocytes resembling tufts (Figs. 1 and 2). The presence of a homozygous mutation in the EpCAM gene was confirmed in patients 2 and 3, with detection of a 17-base pair intragenic deletion (c.352_368del, NM_002354,2). The first patient did not undergo genetic testing.
All patients required PN to prevent dehydration. In the first patient, bowel transplantation was indicated on account of severe malnutrition and high electrolyte requirements. In the second and third patient, it was indicated following the development of PN complications, sepsis and liver disease.
At present, the 3 patients remain alive. Patient 1 has lived with a multivisceral graft for 8 years, patient 2 has lived with a multivisceral graft for 7 years, and patient 3 is awaiting re-evaluation after losing the graft to exfoliative rejection. The first 2 patients have achieved exclusive oral nutrition, exhibit improvement in weight gain and have a good quality of life.
Intestinal epithelial dysplasia was first described in 1994 by Reifen et al.1 Its prevalence is estimated at 1 per 50 000 to 100 000 births, and is higher in Arabic countries.4 In some patients, there is a history of sibling death with severe diarrhoea in the first months of life. Several cases have been reported since the disease was first described, but none in Spain. It is characterised by severe secretory diarrhoea with onset in the first days of life.4 Patients present with manifestations of malabsorption and faltering weight.
Its diagnosis is based on the typical histological features of this disease. Examination with light microscopy reveals marked villous atrophy with crypt hyperplasia in the absence of inflammatory infiltrate in the lamina propria. The characteristic finding is the clustering of closely packed enterocytes, which results in stunted surface projections and form the “tufts” that the disease is known for.1 On examination with electron microscopy, the ultrastructural elements associated with enterocytes tufting include a slight shortening of the brush border and an increase in the desmosome length and number. Immunostaining for MOC31 normally stains the mucosal epithelium but not the lamina propria or vessels. In cases of IED, there is a complete absence of staining in the epithelial surface, crypts and tufts. Some patients present with associated dysmorphic features, oesophageal atresia or choanal or anorectal atresia.4 And up to 60% of patients have associated punctuated keratitis.4
Sivagnanam et al. identified a mutation in the EpCAM gene in chromosome 2 (2p21) in 2008.5 An association with mutations in the SPINT2 gene was discovered at a later time, although they are detected less frequently.6
At present, bowel transplantation is the only option available for these patients with irreversible intestinal failure.3 Our 3 patients have received a transplant, 2 of them have had favourable outcomes and developed enteral autonomy. The third patient is awaiting re-evaluation to decide on subsequent treatment after losing the graft to exfoliative rejection.
In conclusion, IED is one of the causes of early-onset intractable severe diarrhoea, leading to irreversible intestinal failure and indefinite dependence on PN. It is diagnosed based on clinical, histological and genetic features, but may be difficult to identify in some cases due to a patchy and variable presentation. Bowel transplantation is a treatment option that may help these patients develop enteral autonomy and lead normal lives.
Please cite this article as: Rodríguez LT, de Lucas CL, García LNM, Nodal EM-O, Boluda ER. Manejo y pronóstico de la displasia epitelial intestinal. An Pediatr. 2018;88:48–49.