Epidural haematoma (EDH) is a rare condition in newborns, with fewer than 80 such cases reported. The best approach to its management has not been well defined, as some cases resolve spontaneously and others are treated with craniotomy and evacuation. The management will generally depend on the clinical manifestations and the size of the haematoma.1 We describe 3 cases that were associated with complicated vaginal and caesarean deliveries. All 3 were managed with surgery and had favourable outcomes.
Case 1: boy delivered at term by caesarean section due to risk of foetal distress. Apgar 8/9. At discharge, he had a small cephalohaematoma in the right parietal region (1.5×1cm). At 23 days of life, the cephalohaematoma persisted, and a radiograph revealed right parietal depressed skull fracture. The findings of ultrasound examination suggested an extradural collection, which was confirmed by magnetic resonance imaging (MRI): subacute EDH in the right frontoparietal region, 10mm thick, with mass effect and an ipsilateral depressed fracture. The results of the laboratory workup were normal. The patient underwent surgery, which revealed a comminuted and depressed fracture and a dense subgaleal and epidural collection of blood that was evacuated. An incision was made in the dura mater to rule out subdural haematoma. Eight days after the surgery, the patient developed swelling and a subgaleal collection at the site of the surgery that was consistent with pseudomeningocoele (contained cerebrospinal fluid fistula) and required surgery. The follow-up MRI showed no haematoma.
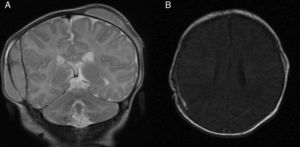
Case 2: girl born to term transferred from another hospital 10 days after birth. Due to risk of foetal distress, labour was induced and delivery by forceps was attempted, but an emergency caesarean section was performed. Apgar 8/9. Bilateral temporoparietal haematomas. At 24h, the patient had an episode with features compatible with convulsive seizure. Brain MRI: subacute extra-axial blood collection measuring 12×48×56mm in the right side, with mass effect, compatible with EDH (Fig. 1A). The findings of laboratory tests and the neurologic examination were normal. The patient underwent surgery, which revealed a non-depressed linear fracture and a dense underlying epidural collection that was evacuated. The followup MRI scan found minimal traces of EDH and improvement in the bilateral cephalohaematomas (Fig. 1B). The neurologic outcome to date is favourable, with no convulsive seizures.
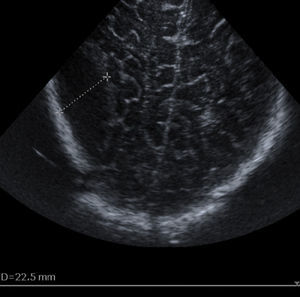
Case 3: boy born to term transferred to our hospital at age 9 days due to EDH in the right parietal region. Complicated spatula-assisted delivery. Apgar 9/10. The EDH was a chance finding of transfontanellar ultrasound examination (Fig. 2). The presence of EDH was confirmed by computed tomography (CT), with a size of 47×21×58mm, and mass effect. The results of the laboratory workup were normal. The patient underwent craniotomy with evacuation of the haematoma. The follow-up CT scan showed the postsurgical changes, and there were no postoperative complications. The patient currently has no neurologic symptoms.
Epidural haematoma in newborn infants is rare and possibly underdiagnosed, as there are limitations to transfontanellar ultrasonography.1 The source of bleeding can be venous or arterial, although in newborns, due to their anatomy and development, it is usually venous and therefore progressive.2 In many of the reported cases, as happened in our patients, there is a skull fracture through with the EDH communicates with an overlying cephalohaematoma.3
The presentation of EDH varies widely, ranging from asymptomatic to convulsive seizures or death, usually in patients with other brain lesions, asphyxia, clotting disorders etc.
This diagnosis is considered based on the risk of intracranial lesion (instrumental delivery, cephalopelvic disproportion, complicated delivery, head trauma), the physical findings (massive cephalohaematoma, skull fracture line or depression) or the clinical manifestations (convulsive seizures, lethargy, signs of raised intracranial pressure).1
At present, the gold standard for diagnosis is MRI or CT, as opposed to ultrasonography, as the former two offer more accurate information regarding the size, thickness, location, and other features of the haematoma. In our patients, transfontanellar ultrasound examination found indirect signs of EDH, subsequently confirmed by MRI or CT.
The management of EDH continues to be subject to debate, as the literature includes descriptions of cases managed with watchful waiting that resolved spontaneously (asymptomatic patients with EDH <1cm).4,5 On the other hand, it seems clear that cases with neurologic impairment and haemodynamic changes warrant an aggressive approach with craniotomy and evacuation of the haematoma.1,3
The controversy revolves around patients who are stable and asymptomatic, in whom multiple approaches have been tried: watchful waiting, needle puncture and aspiration of the cephalohaematoma, in some cases guided by ultrasound,2 or even endoscopy6 or craniotomy with evacuation. There is no evidence that any of them is associated with better outcomes compared to the rest, as most of these patients do not go on to experience severe neurologic deficits, recurrence or convulsive seizures. The level of evidence is low, as the largest series to date comprises 15 cases that occurred over a period of 24 years.1
In our patients, the chosen approach was craniotomy with evacuation of the haematoma due primarily to its sizes (thickness≥10mm with mass effect and risk of calcification in the long term) and in one case a depressed skull fracture that could lead to further cranial deformation with growth. Neurodevelopment was normal in all patients, consistent with the previous literature.1,2,5
Epidural haematoma is infrequent in newborns. It is usually associated with instrumental deliveries, although in this article we describe one case in a patient delivered by caesarean section, which is very rare. It is diagnosed based on the findings of MRI or CT. The optimal approach to treatment varies, ranging from watchful waiting to urgent surgical evacuation.
Please cite this article as: Gregorio-Hernández R, González-Valcarcel M, Escobar-Izquierdo AB, López-Lozano Y, Cabada-Del Río A. Hematoma epidural neonatal. Tres casos y revisión de la literatura. An Pediatr (Barc). 2018;88:50–51.