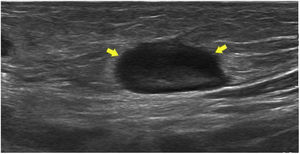
A 12-year-old patient with no medical history of interest presented to the emergency department with pain in the right inguinal region and functional impotence with lameness of 72 h’ duration following a mosquito bite on the right knee. The physical examination revealed a wound on the right knee with raised and swollen edges and a purulent exudate, as well as a warm erythematous area at the right inguinal level associated with tender enlarged lymph nodes. An ultrasound scan evinced 3 reactive lymph nodes in the right inguinal region (Fig. 1). Blood tests showed a C-reactive protein level of 18 mg/L and a white blood cell (WBC) count of 9479 cells/µL (76% neutrophils). Serology, blood culture and wound samples were obtained for microbiological identification, and the patient was admitted to start treatment with intravenous amoxicillin-clavulanic acid (2 g/200 mg).
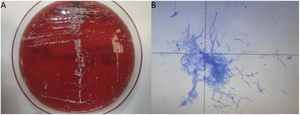
The serological tests for identification of brucellosis, Epstein-Barr virus, Lyme disease, Bartonella, Coxiella burnetii and Rickettsia were negative. The wound specimen was subcultured on agar. Gram staining showed more than 25 WBC/field but no microorganisms. After 48 h of incubation, chalky-white, dry and rough colonies grew on the agar cultures (Fig. 2A), and matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) mass spectrometry (Bruker Daltonics, Massachusetts, USA) identified Nocardia brasiliensis with a value greater than 2.00, indicative of a high-probability. Modified Ziehl-Neelsen staining with 0.5% hydrochloric acid for decolorization was performed to examine the morphology of the microorganism, but no red nor fuchsia acid-fast bacilli could be seen (Fig. 2B), probably because 1% sulfuric acid was needed, rather than hydrochloric acid, but not available. Sequencing of the 16S ribosomal RNA gene confirmed the identification.
(A) Growth of dry white colonies after 48 h of incubation at 37°C on trypticase soy agar with 5% sheep blood, subsequently identified by MALDI-TOF mass spectrometry and 16S rRNA gene sequencing. (B) Modified Ziehl-Neelsen staining using 0.5% hydrochloric acid for decolorization. The branching bacilli did not stain faintly red or fuchsia (partially acid-fast bacilli) because 1% sulfuric acid was required, but not available at the time of diagnosis.
We performed antimicrobial susceptibility testing with the Thermo Scientific Sensititre system, using the Sensititre NOCARDIA Susceptibility Testing Plate. Applying the guidelines of the Clinical & Laboratory Standards Institute, the strain was susceptible to amoxicillin-clavulanic acid, aminoglycosides, tetracyclines, linezolid and trimethoprim/sulfamethoxazole, and was resistant to cefepime, imipenem, ciprofloxacin and clarithromycin. The patient had a favourable outcome, with resolution of lymphadenopathy, and discharged after 3 days with a prescription for oral trimethoprim/sulfamethoxazole at a dose of 800 mg/160 mg every 24 h for 18 days, and completed the 3 weeks of treatment, with favourable outcomes at the 3-month follow-up.
Nocardia brasiliensis is an aerobic, Gram-positive, branched, non-motile, partially acid-alcohol-resistant, saprophytic rod-shaped actinomycete found worldwide in soil, decaying matter and water. Nocardia species are relatively slow-growing, and in some cases it may take up to 1–2 weeks to obtain a viable culture for adequate identification. Inhalation is considered the predominant route of transmission of nocardial infection, since a majority of infections involve the respiratory system. Other possible transmission routes are the gastrointestinal route, through ingestion of contaminated food, or the cutaneous route, by direct inoculation. Some of the risk factors for these infections are malignant disease, HIV infection or immunosuppressive therapy.
Cutaneous forms may present as actinomycetoma, abscesses or with lymphocutaneous involvement, among others. Another cutaneous form is sporotrichoid nocardiosis, which is usually acquired through traumatic injury and is characterized by an ulcerative lesion with painful satellite nodules along lymphatic chains.1 Skin inoculation can also occur through cat scratches or even mosquito bites.1,2 The most plausible explanation for infection following a mosquito bite is that Nocardia species had colonised the skin of the patient through injury and bite created a portal of entry. In other cases, N brasiliensis has been reported as the causative agent involved brain abscesses or meningitis, even in immunocompetent patients.3,4
Microbiological diagnosis is essential for the selection of appropriate antibiotic treatment. Previously, Nocardia spp were identified through macroscopic and microscopic direct examination (granules, morphology or aerial hyphae) and phenotypic methods, but this approach was labour-intensive and time-consuming. At any rate, at present, thanks to the introduction of techniques that have become more accessible in recent years, such as 16S rRNA gene sequencing, Nocardia is identified successfully in most cases. There is evidence of the usefulness of MALDI-TOF mass spectrometry for rapid identification of Nocardia spp, which has been found to achieve good results.5 Furthermore, in the absence of clinical suspicion, MALDI-TOF mass spectrometry allows the identification of this fastidious microorganism from culture isolates within a few minutes.
Trimethoprim-sulfamethoxazole is considered the drug of choice for Nocardia infections because most strains are sensitive to it; other possible options include linezolid, third generation cephalosporins, imipenem or amikacin. Amoxicillin-clavulanic acid can also be an alternative, and its effectiveness was demonstrated in a paediatric case of treatment failure with trimethoprim-sulfamethoxazole.6 If intravenous combination antibiotherapy regimen is used, the duration of treatment could be as short as 2–6 weeks, but the customary recommendation is prescription of a course of treatment lasting 3–6 months. In certain low-risk situations, such as immunocompetent patients or cases of cutaneous infection, it is reasonable to use shorter regimens if the clinical presentation allows it.