The aim of this study was to assess the usefulness of lung ultrasound (LUS) to estimate the endotracheal tube (ETT) depth position during the INtubation–SURfactant–Extubation (INSURE) procedure.
Material and methodsThe ETT insertion depth was estimated using the weight (insertion depth (cm)=weight (kg)+5.5). After intubation, two independent neonatologists using bilateral auscultation or LUS checked the ETT depth.
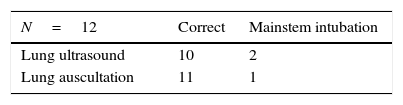
ResultsTwelve newborns with respiratory distress syndrome were included. In two cases LUS helped to correctly replace the ETT. All the patients progressed well, with normal X-ray and LUS before discharge.
ConclusionsLUS appears to be a safe and non-invasive technique and is useful in clinical situations were X-ray is not routinely performed, as it is fast and radiation free.
El objetivo del presente estudio es la valoración mediante la ecografía pulmonar de la profundidad del tubo endotraqueal (TET) durante el procedimiento de Intubation-Surfactant-Extubation (INSURE).
Material y métodosLa profundidad de inserción del TET se calculó mediante el peso del neonato (profundidad de inserción [cm]=peso [kg]+5,5). Después de la intubación, la profundidad del TET fue valorada por 2 neonatólogos independientes mediante la auscultación bilateral y la ecografía pulmonar.
ResultadosDoce neonatos con membrana hialina fueron reclutados. En 2 casos la ecografía pulmonar ayudó a posicionar correctamente el TET. Todos los pacientes presentaron una buena evolución con una radiografía y una ecografía pulmonar normal al alta.
ConclusionesLa ecografía pulmonar es una técnica segura y no invasiva útil en situaciones donde la radiografía de tórax no se usa habitualmente, siendo además rápida y libre de radiación.
Respiratory distress syndrome (RDS), also known as hyaline membrane disease, is caused by a deficiency of surfactant.1 Its management includes noninvasive or mechanical ventilation and, depending on oxygen requirements, the use of exogenous surfactant. In the past decade, early administration of surfactant over a brief period of intubation followed by rapid extubation to noninvasive ventilation (INtubation–SURfactant–Extubation [INSURE]) has become standard practice2 in neonatal units.
One of the main risks of this procedure is the inadvertent administration of surfactant to only one lung, as chest radiography is not routinely performed during the procedure.
There is evidence that lung ultrasound can be useful in the diagnosis of RDS in newborns3 and for assessing the position of endotracheal tubes (ETTs) in adults as well as children.4
This article describes the usefulness of lung ultrasound during the INSURE procedure in helping to avoid inadvertent administration of surfactant to only one lung.
Materials and methodsWe conducted a study between January and December 2014 at the Hospital Sant Joan de Déu (Esplugues de Llobregat, Barcelona), a tertiary care hospital with a volume of 3300 deliveries per year and a neonatal intensive care unit (NICU) with 700 admissions per year.
We obtained the informed consent of parents, and the study was approved by the ethics board of the hospital.
The patients included in the study were newborns with a clinical and radiographic diagnosis of RDS. The choice to carry out the INSURE procedure was made based on the judgement of the neonatologist in charge of the patient. The criteria for administration of surfactant in infants born at more than 32 weeks’ gestation with a weight of more than 1000g are requiring a FiO2 of more than 0.4, a mean alveolar pressure of more than 6cmH2O and chest radiography findings compatible with RDS. During the INSURE procedure, the position of the ETT is verified by means of bilateral auscultation and without chest radiography, as the goal is to perform rapid extubation following surfactant administration.
A consulting senior neonatologist oversaw the procedure as it was performed by a master's student in neonatology. Infants on noninvasive ventilation were sedated according to the NICU protocol prior to intubation. The insertion depth of the ETT was estimated based on the weight (insertion depth [cm]=weight [kg]+5.5), which is the method used to calculate the initial depth of ETT placement in our unit, consistent with the recommendations of the Sociedad Española de Neonatología (Spanish Society of Neonatology)5; placement was confirmed by means of bilateral lung auscultation performed by a different neonatologist blinded to the ETT insertion depth that did not modify the depth and documented whether the auscultation suggested asymmetry. Once the ETT insertion depth had been assessed, a lung ultrasound was performed by a neonatologist experienced in lung ultrasonography and blinded to the ETT placement depth and the results of lung auscultation.
Lung ultrasound was performed with a portable device (Siemens Acuson X300, Siemens Healthcare GmbH, Erlangen, Germany) with a 10MHz linear transducer suitable for the correct visualization of superficial structures. The transducer was placed at the suprasternal level for tracheal ultrasound, and on each hemithorax on a longitudinal plane at the level of the midaxillary line for lung ultrasound.
- –
Verification of correct placement by lung ultrasound required scanning in search of four features:
- –
Visualization of the tip of the ETT in the tracheal region.
- –
Bilateral lung sliding sign: sign that reflects the visceral pleura sliding against the parietal pleura during inspiration and expiration
- –
Bilateral diaphragmatic excursion.
- –
Lung pulse sign: sign observed in the absence of lung sliding, allowing the clear visualization of cardiac pulsations at the level of the pleural line. This sign reflects main stem intubation of the contralateral lung.
In patients in whom ultrasound revealed a unilateral absence of lung sliding and diaphragmatic excursion and/or the presence of the lung pulse sign, the ETT was retracted to the point where the sonographic signs became normal.
This was followed by administration of the surfactant Curosurf (200mg/kg) monitored by ultrasound.
Before discharge, one more confirmatory ultrasound scan was performed to assess lung appearance.
ResultsTwelve patients (Table 1) met the criteria for the INSURE procedure. In all cases, intubation was performed successfully and the tube was placed at the depth estimated based on the weight.
The mean gestational age of the patients was 33 weeks (range, 32–34), the mean weight was 1384g (range, 1100–2150), and the distribution by sex was 7 male and 5 female. Nine patients had been treated with prenatal corticosteroids and seven were born by caesarean delivery. The time elapsed between birth and surfactant administration was 90min (range, 60–120).
Lung auscultation confirmed the correct placement of the ETT in all patients, but right main stem intubation was suspected in one case.
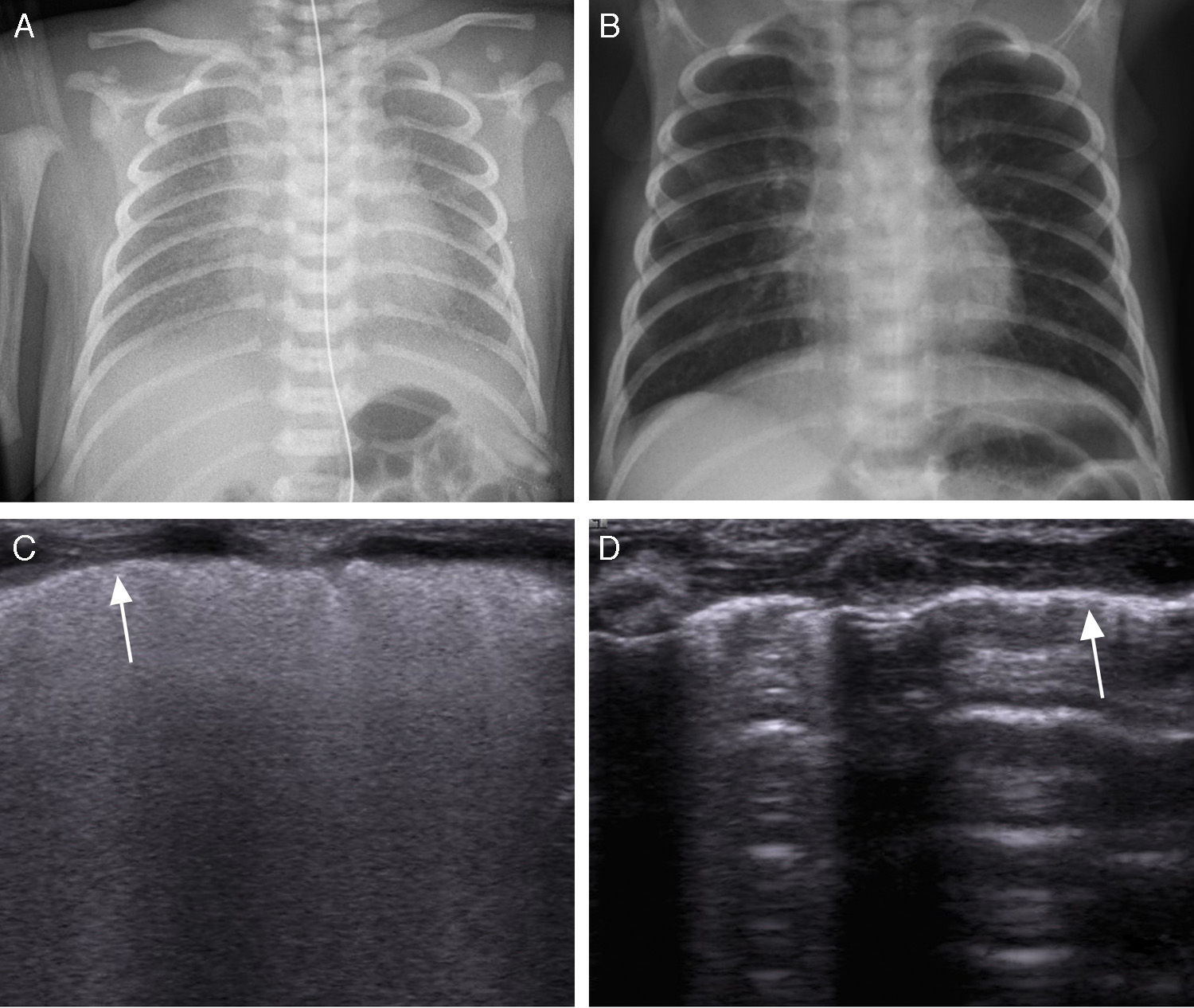
Lung ultrasound revealed an appearance compatible with RDS in all patients (Fig. 1C): compact, diffuse and symmetrically distributed B lines in both lungs with a thickened and irregular pleural line. The transtracheal placement of the ETT was verified in all cases. Lung sliding and diaphragmatic excursion were observed on the right side in all patients, but in two of them lung sliding and diaphragmatic excursion were absent in the left side coinciding with the presence of the lung pulse sign in both. This had been suspected previously during lung auscultation in one of these two patients.
(A) Chest radiograph in a newborn with respiratory distress syndrome. (B) Chest radiograph of the newborn at the time of discharge. (C) Longitudinal lung ultrasound in the same patient, showing a diffuse and compact pattern of lines. The arrow points at the thickened and irregular pleura. Once the patient was intubated, lung sliding was observed bilaterally. (D) Longitudinal lung ultrasound of the patient with a normal hyperechoic pleural line. A lines are thin and parallel to one another, with discernible rib shadows confirming normal appearance without B lines or comet tail artefacts.
Once the ETT had been retracted between 0.5 and 1cm, the bilateral presence of lung sliding and diaphragmatic excursion confirmed correct tube placement, which was followed by administration of surfactant. During the procedure, lung ultrasound found no evidence of complications, such as main stem intubation, pneumothorax or accidental extubation. There were no changes in the sonographic appearance of the lungs during the administration of surfactant or immediately after, consistent with what has been reported in the literature.3 After surfactant administration, patients were extubated to noninvasive ventilation (in less than 15min) in compliance with the INSURE protocol. None of the patients required reintubation or additional doses of surfactant.
The lung ultrasound performed prior to discharge showed a normal appearance (Fig. 1D).
DiscussionIn this study, we assessed the usefulness of lung ultrasound during the INSURE procedure to avoid main stem intubation. Ultrasound confirmed correct placement of the ETT in all patients based on the bilateral presence of both lung sliding and diaphragmatic excursion. This is the first time that the use of this tool for monitoring surfactant administration has been described in this population.
Respiratory distress syndrome or hyaline membrane disease is a pulmonary disorder most frequently found in extremely preterm newborns, but it is not uncommon in newborns with weights exceeding 2500g.6 Traditionally it has been diagnosed by means of chest radiography, but in recent years lung ultrasound has emerged as a useful tool in its identification.7
The need for surfactant therapy in patients with RDS, and especially in extremely preterm newborns, has motivated the search for new and minimally invasive techniques to avoid the potential complications of mechanical ventilation, such as bronchopulmonary dysplasia.8 The INSURE method is one of them. In everyday clinical practice, surfactant administration is preceded by placement of an ETT at a depth estimated on the basis of birth weight9 or gestational age,10 with the subsequent verification of correct placement by bilateral lung auscultation. However, this approach may lead to confusion, especially in extremely preterm patients with low pulmonary compliance and affected by RSD. Some articles have reported that up to 55% of main stem intubations may go undetected by auscultation.11 Another method recommended for placement confirmation is capnography, but this method cannot differentiate between endobronchial intubation and correct endotracheal intubation. Furthermore, the position of the ETT can change substantially with head movements, the administration of drugs or aspirations and result in mainstem intubation, which in turn can cause severe complications such as tension pneumothorax or atelectasis.
The literature has demonstrated the usefulness of lung ultrasound in adult patients for confirmation of endotracheal tube placement under different circumstances,12 including emergency intubation.13 Few studies have been conducted in children,14 and practically none in newborns.15 The criterion used to confirm correct ETT placement is bilateral lung sliding. The absence of sliding in the left side is suggestive of right main stem intubation.16 The fact that bilateral lung sliding may be observed if the patient is breathing spontaneously must be taken into account, and consequently adequate sedation must be ensured to preclude misdiagnosis and for the correct visualization of inspiration and expiration during mechanical ventilation.
The lung sliding sign is also absent in cases of pneumothorax, but these do not present the B lines characteristic of RDS and, unlike what happens in patients with main stem intubation, they feature a pathognomonic sonographic sign of pneumothorax, the lung point sign, which evinces the presence of air between the two pleurae and shows the visceral and parietal pleurae coming into contact during inspiration.
In our small case series we also observed the lung pulse sign,17 previously described in the literature on adults as a sign of main stem intubation.18
Diaphragmatic excursion was observed in all patients. This sign was used in addition to lung sliding for confirmation of tube placement, an approach previously described in the literature for older patients with greater weights.19
Copetti et al.3 reported that changes in the lung appearance of patients with RDS were not observed until 48h after surfactant administration. In our sample of patients, we observed a decrease in oxygen requirements along with an improvement in pulmonary compliance during surfactant administration, but we did not observe in vivo changes in the sonographic appearance during the procedure. Therefore, while lung ultrasound could be a useful tool during the INSURE procedure to avoid main stem intubation, this imaging technique could not be used to monitor other surfactant administration methods that do not involve intubation and are currently used, such as minimally-invasive surfactant therapy,20 a procedure in which surfactant is administered directly into the trachea by means of a flexible or semirigid tube as opposed to an ETT.
There are some limitations to this study. The sample is small, and while the patients included had been born preterm (gestational age <37 weeks), we did not include extremely preterm newborns (gestational age <32 weeks), which are precisely the patients that would most benefit from this tool, as inadvertent one-lung intubation is more frequent in this subset of the population.
Nevertheless, lung ultrasound helped place the ETT correctly in two patients, and since this technique is radiation-free it may be useful as a supplementary technique to confirm correct placement during the INSURE procedure.
We believe that future research on lung ultrasound should focus on its application in correct intubation in the delivery room, as it could be an extremely useful tool in neonatal resuscitation.
In conclusion, the INSURE procedure guided by ultrasound is a technique that is easy to perform at the bedside in newborns, and can allow the detection or prevention of complications such as inadvertent one-lung intubation or accidental extubation during surfactant administration.
Conflict of interestsThe authors have no conflict of interests to declare
We thank the Fundación Andres Marcio for supporting research in the field of cardiology at the Hospital Sant Joan de Déu.
Please cite this article as: Rodríguez-Fanjul J, Balcells Esponera C, Moreno Hernando J, Sarquella-Brugada G. La ecografía pulmonar como herramienta para guiar la surfactación en neonatos prematuros. An Pediatr (Barc). 2016;84:249–253.