Despite the increasing interest in vitamin D functions, new cases of deficiency have been reported in sunny regions where optimal levels are expected. The aim of this study was to analyze 25-hydroxivitamin D levels in children younger than 2 years admitted for acute mild diseases in a tertiary hospital in Valencia and its relationship with factors that can be associated with its deficiency.
MethodsThis one year prospective and observational study was conducted on 169 children admitted for acute mild diseases. 25-Hydroxivitamin D levels were analyzed. A standardized physical examination and structured interviews to the parents were performed. Children were classified into two groups, according to 25-hydroxivitamin D levels (cut-off 30ng/mL).
ResultsA total of 169 children were included, with a median age of 9 months, being more prevalent Caucasians (75.7%) and younger than one year old (79.3%). Almost one quarter (24.3%) of the children had 25-hydroxivitamin D levels <30ng/mL, more frequently in winter/spring, and in children with higher skin phototypes (P<.01). Levels >30ng/mL were associated with vitamin D prophylaxis during the first year, in children of a Caucasian mother, and those who did not wear a hijab. No statistical differences were found in diet characteristics (P=.65). Prophylaxis was given to 47% of the breastfed children younger than one year.
ConclusionsIn Valencia, Spain, 25-hydroxivitamin D levels lower than 30ng/mL were found in a quarter of the children younger than two years. Our results emphasize the importance of vitamin D prophylaxis during the first year of life, even in sunny Mediterranean regions.
A pesar del creciente interés por las funciones de la vitamina D, siguen documentándose casos deficitarios en regiones soleadas donde se presuponen niveles adecuados. El objetivo del estudio es determinar los niveles de 25-hidroxivitamina D en menores de 2 años ingresados en un hospital terciario de Valencia por enfermedades agudas leves y su relación con factores que puedan estar asociados con su deficiencia.
MétodosEstudio prospectivo y descriptivo de un año de duración en niños, entre uno y 24 meses, ingresados por enfermedades agudas leves. Se han estudiado los niveles de 25-hidroxivitamina D, junto con una anamnesis y exploración clínica estructuradas. Se dividió la muestra en 2 grupos, dependiendo de los niveles de vitamina D (punto de corte 30ng/ml).
ResultadosSe estudiaron 169 niños, edad media de 9 meses, predominio etnia caucásica (75,7%) y menores de un año (79,3%). El 24,3% de los niños presentaba valores <30ng/ml, agrupándose en invierno/primavera y caracterizándose por fototipos cutáneos oscuros (p<0,01). Los factores asociados con niveles >30ng/ml fueron: administración de profilaxis, ser hijo de madre caucásica y que no usara hiyab. No existieron diferencias en el tipo de lactancia recibida (p=0,65). Solamente al 47% de los menores de un año amamantados se administró profilaxis.
ConclusionesEn Valencia, a pesar de la radiación solar suficiente, un cuarto de los niños <2 años tiene niveles de 25-hidroxivitamina D <30ng/ml. Nuestros resultados deberían sensibilizar sobre la importancia de la suplementación vitamínica durante el primer año de vida, incluso en las regiones soleadas del Mediterráneo.
Vitamin D plays a crucial role in calcium and phosphorus metabolism and the mineralization of bone. In addition to this widely known function, research conducted in recent years has demonstrated its influence on various genes involved in cellular proliferation and differentiation and on the immune system.1,2 These new findings reinforce the importance of maintaining optimal vitamin D levels in adults as well as children.2–4
The main source of vitamin D is sun exposure of the skin, so vitamin D deficiency is not an expected problem in cities located in the Mediterranean basin, where there are many hours of sunlight (region of Valencia, 2789h of sunlight in 2013).5 However, cases of rickets and severe deficiency continue to be reported in these areas, albeit only in high-risk populations.6–8 Despite the recommendations made by the Spanish Association of Pediatrics (Asociación Española de Pediatría [AEP]),9 the American Academy of Pediatrics (AAP)10 and the European Society for Pediatric Gastroenterology Hepatology and Nutrition (ESPGHAN),11 this continues to be a global health challenge, and it seems that preventive measures are not being implemented correctly.12
This could be due to other factors that reduce sun exposure, such as cultural habits, racial differences in skin pigmentation, and a reduction in the time spent outdoors, as well as the excessive use of sunscreen.
To gain a better understanding of these factors, it would be convenient to determine the vitamin D levels of the healthy population for all age groups. Substantial research has been conducted in areas where vitamin D deficiency should not be expected a priori, especially on adolescents and school-aged children; however, infants have only been studied in countries with fewer hours of sunlight per year.13,14
The main objective of this study was to assess vitamin D levels in children aged less than 2 years admitted to a tertiary care hospital in Valencia with mild acute diseases. The secondary objective of this study was to determine the presence of vitamin D deficiency, describing the variables associated with it and its clinical manifestations.
Materials and methodsPopulation under studyWe conducted a prospective observational study over a one-year period (December 2012 to November 2013) of the children admitted to the pediatric ward with mild acute diseases.
Inclusion criteria- -
Age between 1 month and 2 years.
- -
Informed consent signed by parents.
- -
Availability of an adequate blood sample collected during the venipuncture performed to assess the disease for which the patient was admitted.
- -
Having undergone a structured history taking and physical examination in the context of the study.
- -
Moderate or severe disease.
- -
Presence of any chronic disease or medical condition that may predispose to vitamin D deficiency, such as heart disease, liver failure, kidney failure, malabsorption syndrome, malformation syndrome or premature birth.
- -
Failure to meet all the inclusion criteria.
Once the child had been admitted to the ward and the parents signed the informed consent form, the blood sample was collected and taken to the laboratory to determine the level of 25-hydroxy vitamin D (25(OH)D).
After this, a structured history was taken from the parents and the child underwent physical examination, all of which was documented in the study worksheet: personal data, family and individual medical history, ethnicity, type of diet, and other aspects related to risk factors for vitamin D deficiency (mean weekly number of hours spent outdoors, maternal phototype, cultural factors, vitamin D supplementation). In addition to anthropometric measurements (weight, length, height, head circumference, body mass index [BMI] and growth rate), the physical examination of the child included an evaluation of the skin phototype and a thorough assessment of any signs suggestive of rickets.
Skin phototype, defined as an individual's capacity to adapt to sun exposure, was classified according to the Fitzpatrick scale into one of 6 categories, ranging from phototype 1 (pale white skin and red hair) to phototype 6 (dark skin and black hair).15
The authors personally took the histories and performed the physical examination (A.T., D.E.M, S.B.S, N.S.D.) in the 24h following admission, prior to obtaining the vitamin D level results.
Vitamin D levels were determined by means of chemoluminescent protein-binding assays (cobas e 411 analyzer, Roche), the results of which were available 48h after admission. We established a cut-off value of 30ng/mL (75nmol/L), as established by Hollis and other authors.3,16–19
We classified children in the sample into two groups: group 1, with vitamin D levels lower or equal to 30ng/mL, and group 2, with vitamin D levels greater than 30ng/mL.
The parents were apprised of the test results prior to discharge, and treatment was prescribed for patients with levels below 30ng/mL. Parents were also educated on dietary factors and appropriate sun exposure for the maintenance of adequate vitamin D levels.
The study was approved by the ethics committee of the Hospital Clínico de Valencia.
Statistical analysisWe performed a descriptive analysis of the collected data. We have expressed quantitative variables as mean and standard deviation, and qualitative variables as relative frequencies or percentages.
To analyze the association between variables comparing the two groups (groups 1 and 2), we used nonparametric tests (chi squared test or Mann–Whitney U test, depending on the type of variable). We set the level of statistical significance at 95%.
Study limitationsThe main limitation of our study is that there was a considerable selection bias, as participants were previously healthy infants that were hospitalised due to a mild acute disease unrelated to vitamin D deficiency. Thus, it is possible that the results are not a faithful reflection of the current situation in the general population.
We also need to consider that recent studies have proposed that 25(OH)D may act as a negative acute phase reactant, with decreased levels in individuals with inflammatory diseases.20,21 Furthermore, some of the data, such as the amount of sun exposure, the number of previous infections and diet characteristics were collected retrospectively by the parents.
ResultsOut of the total of 213 children that met the inclusion criteria, only 169 ended up participating in the study. In one case, the parents did not sign the informed consent form; in thirty-three, not enough blood was collected to determine the concentration of vitamin D; and in ten cases, either the history taking or the physical examination could not be completed due to early discharge of the patient.
The different diseases of the participants fell into the following categories: 26% (44) urinary tract infection; 20.1% (34) bronchiolitis; 17.2% (29) bacteraemia; 14.2% (24) pneumonia; 5.3% (9) acute gastroenteritis; 4.7% (8) upper respiratory tract infection; 3.6% (6) disease requiring surgical treatment; 3.6% (6) seizures; 1.8% (3) skin infection; and there was one case each of hypoglycaemia, drug intoxication, erythema multiforme, Kawasaki disease, meningitis and varicella.
The mean age of the 169 children was 9.02±7.69 months, with a predominance of children less than 1 year of age (79.3%; 134/169); 56.2% (95/169) were male and 43.8% (74/169) female. Their anthropometric measurements were within normal ranges.
The distribution by ethnicity or national origin was the following: 75.7% Caucasian (128/169), 7.7% Latin American (13/169), 7.7% Roma (13/169), 4.1% Maghrebi (7/169), 2.3% Sub-Saharan African (4/169), 1.7% Indo-Pakistani (3/169), 0.6% Chinese (1/169).
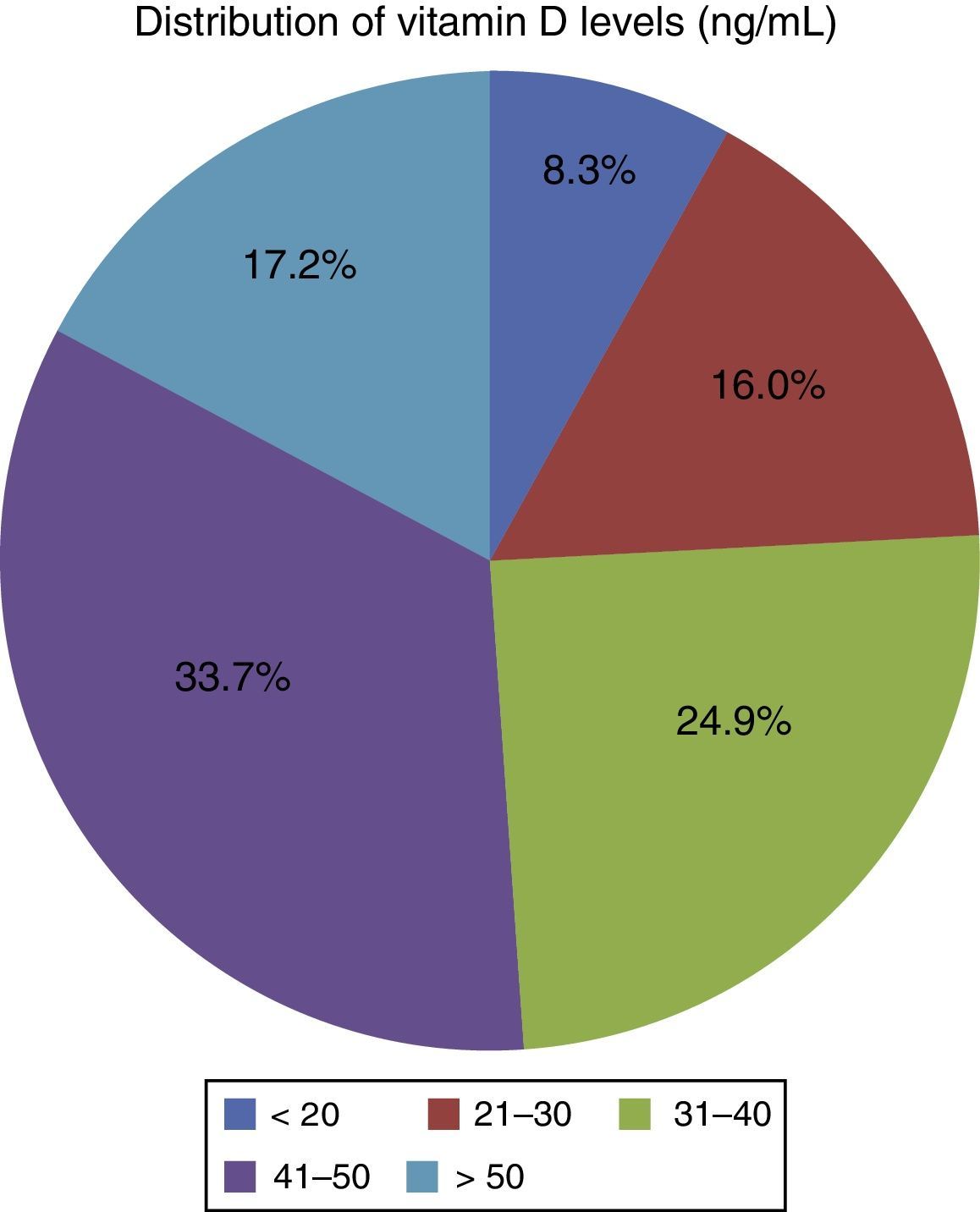
Of all children, 24.3% (41/169) had vitamin D levels below30ng/mL, with 16% (27/169) having values between 30 and 20ng/mL, and 8.3% (14/169) values below 20ng/mL (Fig. 1). Thus, group 1 was comprised of 41 children (M/F, 26/15) and group 2 of 128 children (M/F, 69/59).
Table 1 summarizes the associations of the different variables under study for groups 1 and 2.
Comparison of variables under study between the group with vitamin D deficiency and the group with no deficiency.
| Group 1(n=41) | Group 2(n=128) | P value | |
|---|---|---|---|
| Age (decimal age) | 0.82±0.81 | 0.80±0.67 | 0.26 |
| Sex | 0.28b | ||
| Male | 63.4% (26)a | 53.9% (69) | |
| Female | 36.6% (15) | 46.1% (59) | |
| Month at admission (median) | 5 | 7 | 0.01c |
| Length (z-score) | 0.30±1.02d | 0.17±1.59 | 0.66e |
| Weight (z-score) | −0.23±1.01 | −0.34±1.12 | 0.63 |
| BMI (z-score) | −0.46±1.11 | −0.59±1.15 | 0.62 |
| Head circumference (z-score) | −0.07±1.44 | −0.08±1.49 | 0.71 |
| Growth rate (cm/year) | 35.32±15.41 | 39.36±41.08 | 0.74 |
| Smoking during pregnancy | 13.9% (5) | 10.2% (13) | 0.53 |
| Infections/month | 0.65±0.76 | 0.38±0.41 | 0.08 |
| Previous hospitalisations | 35.1% (13) | 32.0% (41) | 0.72 |
| Breastfeeding | 73.7% (28) | 77.2% (98) | 0.65 |
| Supplementation | 25.0% (9) | 50.8% (62) | 0.01c |
| Number of months | 2.61±3.92 | 3.56±2.53 | 0.05f |
| Sun exposure (hours/week) | 10.11±8.19 | 12.36±9.07 | 0.24 |
| Caucasian ethnicity | 45.9% (17) | 78.9% (97) | 0.01c |
| No hijab use | 83.8% (31) | 98.3% (119) | 0.01c |
| Maternal phototype | 0.10 | ||
| 2 | 17.6% (2) | 34.5% (41) | |
| 3 | 44.1% (15) | 47.9% (57) | |
| 4 | 26.5% (9) | 12.6% (15) | |
| 5 | 8.8% (3) | 3.4% (4) | |
| 6 | 2.9% (1) | 1.7% (2) | |
| Child's phototype | 0.01c | ||
| 1 | 2.7% (1) | 0.0% (0) | |
| 2 | 27.0% (10) | 48.8% (59) | |
| 3 | 37.8% (14) | 39.7% (48) | |
| 4 | 16.2% (6) | 7.4% (9) | |
| 5 | 13.5% (5) | 2.5% (3) | |
| 6 | 2.7% (1) | 1.7% (2) | |
| Abnormal findings in examination | 45.7% (16) | 18.3% (22) | 0.01c |
The most salient findings involved the median month of admission, with a higher proportion of admissions in the winter and spring for the group with low vitamin D levels (median, May) compared to a higher proportion of admissions in the summer and autumn in the group with normal levels (median, July).
We found a greater frequency of previous infections in group 1 (P=0.08) along with a predominance of skin phototypes higher in the Fitzpatrick scale (P<0.01). The frequency of clinical signs of rickets (anterior fontanelle with soft edges, mild frontal bossing, deformation of lower limbs) was higher in these children than in the control group.
Group 2 membership was significantly associated with administration of vitamin D prophylaxis and its duration, mothers of Caucasian descent, and mothers that did not wear a hijab regularly. We did not find statistically significant differences in the vitamin D levels of patients whose mothers wore a hijab based on the type of feeding (human milk vs formula). On the other hand, we did not find significant differences between groups based on the number of hours of sun exposure and the type of feeding, even for breastfed children that did not receive supplementation (P=0.65) (Table 1).
DiscussionDue to the abundance of sunlight in locations of the Mediterranean region such as Valencia (which had 2789h of sunlight in 2013),5 there is a widespread belief, in the general population as well as among healthcare professionals, that vitamin D levels are adequate. Contrary to this belief, our study found that 24.3% of children aged less than 2 years admitted to our hospital for mild acute diseases had levels below 30ng/mL.
We should also mention that another study conducted in the city of Valencia in 2007 found levels below 10ng/mL in 8.3% of infants aged less than 6 months.22 These studies prove that vitamin D deficiency continues to be a problem in Valencia.
In the Iberian Peninsula, at a latitude of 43° North and 36° South, exposure of 30% of the total body surface area to ultraviolet B radiation (UBV) for 10–15min between the hours of 10 am and 3 pm during non-winter months is enough to produce 1000IU of vitamin D.23 Our data seem to support that season is related to vitamin D levels, as inadequate levels were more common in the winter and spring. This finding could be explained by the decrease in sunlight that occurs in the winter, which would prevent the synthesis of optimal amounts of vitamin D and result in hypovitaminosis during the spring.
Consistent with the literature, the vitamin D levels were negatively correlated to the skin phototype of the child, with the risk of hypovitaminosis seemingly increasing with the phototype.24 When this factor is associated with specific maternal cultural habits involving clothing that restricts sun exposure or a diet rich in phytates, low levels of vitamin D in the mother pose an evident risk to the child. There is evidence that maternal vitamin D levels are directly correlated to neonatal levels and child growth and development.24–26 Unlike other authors, we did not find statistically significant differences between the groups in the weekly number of hours of direct sun exposure (P=0.24).
Human milk contains approximately 2IU/100mL of vitamin D, compared to concentrations of 40–56IU/100mL in infant formulas and 68–72IU/100mL in follow-on formulas.27 Based on these data, we would assume that breastfeeding without vitamin supplementation carries a higher risk of vitamin D deficiency, but we did not find a higher prevalence of deficiency in breastfed children, grouped on the basis of receiving or not receiving vitamin D prophylaxis, compared to formula-fed children.
Other factors under study, such as sex, age, weight, length, head circumference and BMI, were not affected by vitamin D levels. However, several studies have found an association between obesity (BMI) and the prevalence of hypovitaminosis D due to the accumulation of the vitamin in fatty tissues and the resulting reduction in its bioavailability.28,29
We found that signs of rickets were more frequent in children with concentrations below 30ng/mL (P<0.01), but the physical examination does not seem to suffice to suspect deficiency in the early stages, as the abnormalities that we found (mild frontal bossing, wide anterior fontanelle with soft edges, minimal deformation of lower limbs with or without proximal muscle weakness) are difficult to identify because they are nonspecific and highly subjective, and may be overlooked in routine health checkups.
Given the importance of maintaining optimal vitamin D levels in the pediatric age group and the high prevalence of vitamin D deficiency, health institutions recommend the routine administration 400IU of vitamin D a day to all infants aged less than 1 year, either through diet with an oral preparation, or through the parenteral route.9–11,30–33
A 2007 Cochrane review provided strong evidence in support of daily supplementation with 400IU of vitamin D in the first 12 months of life for the prevention of rickets,34 while the evidence currently available does not suffice to recommend supplementation in older children.
Contrary to what we expected, we could not precisely define the at-risk population based on the factors under study, but we were able to corroborate that the administration of prophylaxis correlated to higher vitamin D levels, which supports its recommendation.
At present, the definition of the normal levels of vitamin D is the subject of heated debate. Due to the use of different laboratory methods to measure the concentration of 25(OH)D and the difficulties involved in establishing the limits for reference levels in every age group, there is no consensus on the serum concentrations that define vitamin D insufficiency in infants and children.34,35 Some authors and scientific institutions consider that vitamin D levels are insufficient when the serum concentration of 25(OH)D is less than 20ng/mL, and that they are deficient when the concentration is less than 12ng/mL.36,37
However, some studies have found data that contradict this definition, such as the presence of bone changes in radiographs of dark-skinned infants with levels ranging between 16 and 18ng/mL, or a decrease in bone density in adolescents with values below 16ng/mL in Sweden,38,39 leading other recognized authors to define optimal levels of 25(OH)D as a range of 30–90ng/mL, insufficient levels as a range of 20–30ng/mL, and deficiency as levels below 20ng/mL.16–19,23,30
These definitions have been extrapolated from studies in the adult population that associated the serum concentrations of vitamin D, parathyroid hormone, and calcium and bone resorption, and were based on the levels at which the production of parathyroid hormone, the intestinal reabsorption of calcium and bone calcium resorption were lowest.40
The objectives, population and methods of our study do not allow for it to make a relevant contribution to this interesting debate, and further studies with better resources, a higher level of standardization and homogeneous and reproducible laboratory methods are needed to improve the current level of evidence on the optimal vitamin D levels for infants and older children.
ConclusionsEven though there is enough sunlight in Valencia to guarantee adequate vitamin D synthesis, approximately 25% of the children in the study had levels below30ng/mL and clinical manifestations that could be overlooked in routine health checkups. Adherence to current recommendations for vitamin D prophylaxis was only found in 50% of the infants. Our results should make pediatricians more aware of the need of routine vitamin D supplementation in the first year of life, even in sunny cities in the Mediterranean region.
Conflicts of interestThe authors have no conflicts of interest to declare.
We want to thank Dr. María José López, from the pediatrics department of the Hospital Clínico de Valencia, for her patience in assisting us; the nursing staff of the pediatric ward for their cooperation; and Dr. Francisco José Santonja, from the Department of Statistics and Operational Research of the Universidad de Valencia, for his help in the statistical analysis.
Please cite this article as: Togo A, Espadas Maciá D, Blanes Segura S, Sivó Díaz N, Villalba Martínez C. ¿Existe déficit de vitamina D en los niños de una ciudad soleada del Mediterráneo? An Pediatr (Barc). 2016;84:163–169.