The postcode (where the home is situated) is an indicator of socioeconomic status and is associated with morbidity, mortality, and the use of health services. The aim of this study was to analyze its effects on paediatric admissions and to determine the rates of the most common causes of paediatric admissions in Seville.
Matherials and methodsObservational cross-sectional study with two analysis units: under 15 year-old “admissions” in public hospitals in Seville (n=2660) and “city districts” of Seville (n=11). The independent variable analyzed was whether the postcode of the admitted patients was within a Regional Government designated “area with social transformation needs”. The analysis of the admissions was performed using X2-test, Fisher test and Student-t test, with the description of rates using the calculation of crude and specific rates, and by rate ratio.
ResultsChildren living in districts with a lower socioeconomic status were on average 7 months younger (p<0.001), and they were significantly more likely to be admitted via the emergency department (p<0.001). There was no statistical difference detected in either the length of hospital stay or mortality. The crude admission rate ratio was higher in districts with a lower socioeconomic status (1.8), with a higher specific rate ratio detected in admissions due to asthma, respiratory infections, inguinal hernia, and epilepsy/convulsions.
ConclusionsPaediatric hospital admission rates of the main diagnoses were higher in districts with a lower socioeconomic status. Children living in these districts were more likely to be admitted younger and via the emergency department.
El lugar de vivienda es un indicador del nivel socioeconómico que influye en la morbimortalidad y utilización de recursos sanitarios. Los objetivos de este estudio fueron analizar este efecto en las hospitalizaciones pediátricas y describir las tasas de hospitalización de los diagnósticos principales más frecuentes en la ciudad de Sevilla.
Material y métodosEstudio observacional y transversal con 2 unidades de análisis: «ingresos hospitalarios» en los hospitales públicos de Sevilla de menores de 15 años (n=2.660) y «distritos de Sevilla» (n=11). La variable independiente de estudio fue la residencia en distritos con o sin «zonas de necesidad de transformación social», obtenida del código postal. El análisis de las características hospitalarias se realizó mediante los test de la χ2, Fisher y t de Student, y la descripción de tasas mediante el cálculo de tasas cruda y específica, y del índice de tasas.
ResultadosLos ingresos pediátricos procedentes de distritos con menor nivel socioeconómico se produjeron a una edad media 7 meses menor (p<0,001) y con carácter urgente en mayor proporción (p<0,001). No se detectaron diferencias en la estancia media ni en la mortalidad intrahospitalaria. El índice de la tasa bruta de hospitalización fue superior en los distritos con menor nivel socioeconómico (1,8), con una mayor diferencia en las tasas específicas de hospitalización por asma, infecciones respiratorias, hernia inguinal y epilepsia/convulsiones.
ConclusionesLas tasas de hospitalización de los diagnósticos principales más frecuentes fueron mayores en distritos con menor nivel socioeconómico. Sus ingresos se produjeron a edades más tempranas y con mayor carácter urgente.
Health is largely conditioned by social determinants.1 The circumstances under which a person is born, grows, works and ages determines not only the 3 dimensions of health—physical, psychological and social2—but also life expectancy.3 Inequalities in health can be explained by the different living conditions of individuals, which depend on the political and socioeconomic context (structural determinants) and the opportunities in education and employment that will determine their work, housing, place of residence etc. (intermediary determinants).4 Inequalities in health are unfair and preventable, and their consequences have been amply proven. Exposure to unfavourable living conditions during childhood has a great impact on long-term health and development during adult life,5 and therefore interventions implemented in the early stages of life are the most cost-effective.6
Numerous studies use the place of residence as a socioeconomic determinant, using indicators such as educational attainment, unemployment, type of occupation or average income of the population of an area.7 There is evidence of an inverse correlation between mortality and socioeconomic level in the comparison between cities and between districts or neighbourhoods within a city.8,9 There is evidence that the postcode can be useful in representing a geographical area and as an indicator of socioeconomic level10; on the other hand, the studies conducted by the MEDEA group in Spain have been using census divisions to demonstrate the aforementioned correlation for different causes of death.11,12 Other studies have found evidence of a higher frequency of hospital visits in members of socially-disadvantaged groups,13,14 as well as an unequal use of different health care resources.15,16 But there are not many studies that assess the impact of the place of residence—used as an indicator of socioeconomic level—on the health of children in Spain.
A systematic review of studies on the impact of social inequalities in child and adolescent health in Spain17 revealed a broad variability in the indicators used as social determinants and a scarcity of studies in preschool-aged children. The paediatric health issues studied most frequently were obesity,18 mental health19 and dental health,20 and the data demonstrated the negative impact of a low socioeconomic status. Studies conducted in the United States21,22 have also demonstrated this correlation with the same health problems as well as others, such as preterm birth, faltering weight, behavioural and learning disorders, traumatic injury, poisonings and asthma, with a higher number of hospital admissions in patients of lower socioeconomic status due to the latter.23,24 A prospective study in a cohort of newborns followed up over 10 years also found an increased frequency of respiratory and gastrointestinal diseases, traumatic injury and poisonings in patients with fewer resources.25 Last of all, there are studies that have found increased use of inpatient services, longer mean lengths of stay, increased inpatient costs26–28 and even a higher in-hospital mortality25,29in hospitalised paediatric patients from areas of a low socioeconomic level.
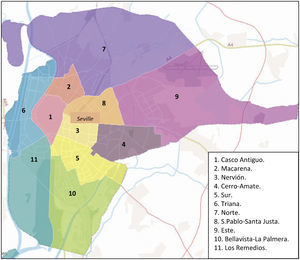
The growth of the outskirts of the city of Seville peaked around the second half of the 20th century, when most of the working-class neighbourhoods that exist today were developed and expanded.30 Seville is divided into 11 districts,31 of which 6 are above the 75th percentile in the distribution of mean per capita annual income32: Casco Antiguo, Nervión, San Pablo-Santa Justa, Bellavista-La Palmera, Triana and Los Remedios. Areas with social transformation needs (ASTNs) have been defined as urban areas whose inhabitants are in a structural situation of extreme poverty or social marginalization. This status is determined based on indicators such as housing, education, unemployment, hygiene-sanitation deficiencies, and manifestations of social disintegration.33 The Public Health Service of Andalusia has implemented an action plan adapted to the needs of ASTNs. In Seville, there are 11 identified ASTNs, located in the 5 districts with the lowest annual per capita income.34 These 5 districts border the city centre in the north, east and south-east.
The objectives of our study were: (1) to analyze the impact of place of residence in the hospitalization characteristics of paediatric admissions in Seville, and (2) to describe the rate of hospital admission for the most frequent primary diagnosis by city district.
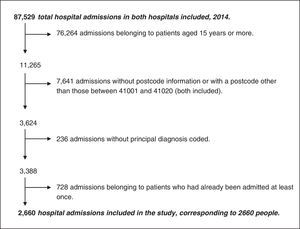
Materials and methodsWe conducted a cross-sectional observational study on the most frequent reasons for paediatric hospital admissions in the city of Seville in relation to place of residence. We pursued objective 1 by an analysis in which the unit of analysis was “hospital admission”, and objective 2 by a descriptive ecological study in which the unit of analysis was “districts of Seville”. We obtained the data from the discharge summaries, or “Minimum Basic Discharge Data Set” (Conjunto Mínimo Básico de Datos al Alta [CMBD])35 of the 2 public hospitals serving the residents of the city of Seville: the Hospital Universitario Virgen del Rocío and the Hospital Universitario Virgen Macarena. We included hospitalizations in which patients were discharged between January 1st, 2014 and December 31st, 2014. The exclusion criteria were: age 15 or more years, residential postcodes outside of the 41001–41020 range (postcodes outside the city of Seville), lack of data on the postcode or the primary diagnosis, and hospital readmission. For the sake of preserving the independence of observations, in cases of patients that were admitted to hospital more than once, we only included the first admission. A total of 2660 patients were included in the study after applying these criteria (Fig. 1).
The independent variables were age, sex, postcode, district and ASTN. The dependent variables were type of admission, hospital, length of stay, type of discharge and primary diagnosis coded according to the International Classification of Diseases (ICD-9-MC).36 We built the district and ASTN variables from the postcode variable based on the distribution of postcodes by district established by the City Council of Seville (Fig. 2)31 and the postcodes that contain the neighbourhoods classified as ASTNs by the Government of Andalusia,34 respectively (Table 1). The administrative division of the city of Seville (into districts) does not coincide exactly with the postal division (into postcodes). The criterion we used to assign postcodes to districts was that 75% or more of the streets were being contained in one district. This criterion was met for all postcodes except 41008 (55.1% of streets in Macarena), 41016 (70.8% of streets in Este) and 41019 (52.4% of streets in Norte). We assigned postcode 41019 to the Este district given its physical proximity, and the other 2 postcodes to the district that contained the larger percentage of streets.
Distribution of postcodes, districts and areas with social transformation needs in the city of Seville.
| Postcode | District | Neighbourhoods considered ASTNs |
|---|---|---|
| 41001 | Casco Antiguo | None |
| 41002 | Casco Antiguo | None |
| 41003 | Casco Antiguo | None |
| 41004 | Casco Antiguo | None |
| 41005 | Nervión | None |
| 41006 | Cerro-Amate | Los Pájaros-Amate, La Plata |
| 41007 | San Pablo-Santa Justa | None |
| 41008 | Macarena | None |
| 41009 | Macarena | Polígono Norte |
| 41010 | Triana | None |
| 41011 | Remedios | None |
| 41012 | Bellavista-La Palmera | None |
| 41013 | Sur | Las Letanías, Polígono Sur |
| 41014 | Bellavista-La Palmera | None |
| 41015 | Norte | La Bachillera, El Vacie, Los Carteros |
| 41016 | Este | Carretera Torreblanca, Torreblanca de los Caños, San Rafael |
| 41017 | Este | Carretera Torreblanca, Torreblanca de los Caños, San Rafael |
| 41018 | Nervión | None |
| 41019 | Este | None |
| 41020 | Este | None |
To calculate the rates of different primary diagnoses at admission, we took into account those diagnoses that amounted to 1% or more of the total 2660 admissions included in the study (Table 2). Code 518.81 (acute respiratory failure, 5.49%) was included in the asthma, bronchitis or pneumonia categories if the latter featured as a secondary diagnosis. We grouped into single categories the codes corresponding to bronchitis, bronchiolitis and bronchospasm; the codes for pneumonia; the codes for epilepsy and unspecified convulsions; the codes for hypertrophy of tonsils and of adenoids; and the codes low birth weight, prematurity and intrauterine growth restriction (IUGR). We assigned codes 780–799 (“symptoms, signs, and ill-defined conditions”) to other, better-defined categories if any of the latter were recorded as a secondary diagnosis. Although the total number of patients with asthma as the main reason for admission did not reach 1%, we decided to preserve this category on account of the existing literature on its association with place of residence.23,24 We excluded primary diagnoses coded as 780.6 (“fever and other physiologic disturbances of temperature regulation”) or 599 (“other disorders of urethra and urinary tract”) even though they did slightly exceed 1%, due to the nonspecificity of the former, and to incomplete coding in the latter.
Primary diagnoses included in the calculation of the rate of admissions.
| Primary diagnosis | ICD-9-CM code | Patients (n) | Percentage (%) |
|---|---|---|---|
| Asthma | 518.81a, 493 | 17 | 0.6 |
| Bronchitis, bronchiolitis or bronchospasm | 518.81a, 519.11, 519.19, 466 | 263 | 9.89 |
| Pneumonia | 518.81a, 480–486 | 52 | 1.95 |
| Epilepsyand other convulsions | 345, 780.39 | 120 | 4.51 |
| Gastroesophageal reflux | 530.81b | 64 | 2.41 |
| Hypertrophy of tonsils and/or adenoid vegetations | 474.1, 474.2 | 135 | 5.08 |
| Appendicitis | 540 | 95 | 3.57 |
| Inguinal hernia without obstruction or gangrene | 550.9 | 28 | 1.05 |
| Preterm birth, prematurity or IUGR | 764, 765b | 222 | 8.35 |
| Maternal infection affecting newborn | 760.2b | 42 | 1.58 |
We assessed the impact of the place of residence on the distribution and characteristics of hospital admissions by means of a bivariate analysis in which ASTN was the independent variable. We conducted a bivariate analysis of sex and primary diagnosis that led us to include a detailed analysis based on sex. The statistical tests used in the analyzes were the χ2, Fisher exact test and Student t, carried out with the software R i386 3.3.0; we defined statistical significance as a p-value of less than 0.05.
To calculate the rate of hospital admissions, we created a second unit of analysis from the 11 districts of the city, with the districts group based on whether or not they contained ASTNs. The source of the data used to calculate the denominators was the census of Seville inhabitants of January 01, 2015.37 We used the total population aged less than 15 years, and for the 2 neonatal diagnoses included in the study, the number of children born in 2014. Using these populations, we calculated specific rates for each district and for the groups of districts with and without ASTNs. We compared the rates of districts with and without ASTNs by calculating rate ratios.
ResultsTable 3 shows univariate analysis of the demographic and hospital variables. The age group with the highest rate of hospital admissions corresponded to children aged less than 5 years (61.95%). The mean age at hospital admission in children from districts with ASTNs was 3.80 years, compared to 4.37 years in children from districts without ASTNs (Student t; p<0.001). There were more admissions of boys (56.69% boys vs 43.23% girls). We did not find a statistically significant association between sex and residence in an ASTN (χ2 test; p=0.475), or sex and any of the primary diagnoses, save for pneumonia, which was more frequent in girls: 2.7% vs. 1.4% (χ2 test; p=0.017). The proportion of urgent admissions was higher in the admissions of patients from districts with ASTNs compared to districts without: 73.50% vs 66.10% (χ2 test; p<0.001). We did not find statistically significant differences in the type of discharge (Fisher exact test; p=0.909). Of all in-hospital deaths, 50% (n=10) were of patients from ASTNs. The mean length of stay was similar in both groups: 5.68 days for admitted patients from ASTNs vs 5.54 days for patients that did not reside in an ASTN (Student t; p=0.744).
Univariate analysis of age, sex, hospital of admission, type of admission, department of admission, type of discharge and area with social transformation needs (ASTN).
| Variable | Frequency (n) | Percentage (%) |
|---|---|---|
| Age | ||
| 0–4 years | 1648 | 61.95 |
| 5–9 years | 456 | 17.14 |
| 10–14 years | 556 | 20.90 |
| Sex | ||
| Female | 1150 | 43.23 |
| Male | 1508 | 56.69 |
| Undetermined | 2 | 0.08 |
| Hospital | ||
| Macarena | 1164 | 43.76 |
| Rocío | 1496 | 56.24 |
| Type of admission | ||
| Urgent | 1853 | 69.66 |
| Scheduled | 807 | 30.34 |
| Department of admission | ||
| Neonatology | 319 | 11.99 |
| Paediatrics | 1495 | 56.20 |
| Other | 846 | 31.81 |
| Type of discharge | ||
| Home | 2621 | 98.53 |
| Transfer | 27 | 1.02 |
| Against medical advice | 1 | 0.04 |
| Death | 10 | 0.37 |
| Not documented | 1 | 0.04 |
| From a district with ASTN | ||
| Yes | 1272 | 47.82 |
| No | 1388 | 52.18 |
We did not find statistically significant differences in the bivariate analysis of the “hospital admissions” based on the presence of ASTNs for any of the primary diagnosis. For neonatal admissions, we only included admissions of newborns aged less than 28 days (n=512), and found p-values that neared statistical significance for low birth weight, preterm birth or IUGR (χ2 test; p=0.051). When it came to newborns affected by maternal infection, the p-value rose to 0.627. However, the descriptive analysis of the overall rates of admission and the specific rates by districts of Seville did show differences in the distribution of hospital use based on district (Tables 4 and 5). The overall rate of admission for all the primary diagnoses included in the study was higher in districts that contained ASTNs (overall rate ratio=1.8). With the exception of hypertrophy of the tonsils and/or adenoids, all the specific rates of admission were higher in districts with ASTNs, and these differences were larger for respiratory infections, asthma, epilepsy/convulsions and inguinal hernia, with ratios equal or greater than 1.8 (Table 6).
Overall and specific rates of paediatric admission by Seville district (admissions/100,000 inhabitants aged less than 15 years).
| Area | Population (<15 years) | Asthma | Bronchitis/bronchiolitis | Pneumonia | GER | Appendicitis | Inguinal hernia | Adenoid/tonsil HT | Epilepsy and convulsions | All admissions | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| District | n | Rate | n | Rate | n | Rate | n | Rate | n | Rate | n | Rate | n | Rate | n | Rate | n | Rate | |
| Casco Antiguo | 7643 | 2 | 26.17 | 25 | 327.10 | 5 | 65.42 | 4 | 52.34 | 6 | 78.50 | 3 | 39.25 | 8 | 104.67 | 13 | 170.09 | 204 | 2669.11 |
| Macarena | 9580 | 9 | 93.95 | 55 | 574.11 | 9 | 93.95 | 10 | 104.38 | 15 | 156.58 | 7 | 73.07 | 7 | 73.07 | 23 | 240.08 | 474 | 4947.81 |
| Nervión | 7080 | 0 | 0.00 | 15 | 211.86 | 0 | 0.00 | 4 | 56.50 | 2 | 28.25 | 1 | 14.12 | 8 | 112.99 | 4 | 56.50 | 115 | 1624.29 |
| Cerro-Amate | 14,042 | 0 | 0.00 | 36 | 256.37 | 7 | 49.85 | 6 | 42.73 | 15 | 106.82 | 3 | 21.36 | 37 | 263.50 | 16 | 113.94 | 375 | 2670.56 |
| Sur | 11,551 | 1 | 8.66 | 21 | 181.80 | 7 | 60.60 | 6 | 51.94 | 12 | 103.89 | 0 | 0.00 | 13 | 112.54 | 13 | 112.54 | 234 | 2025.80 |
| Triana | 6262 | 0 | 0.00 | 8 | 127.75 | 3 | 47.91 | 6 | 107.93 | 6 | 107.93 | 0 | 0.00 | 11 | 197.88 | 5 | 89.94 | 106 | 1906.82 |
| Norte | 11,455 | 3 | 26.19 | 38 | 331.73 | 9 | 78.57 | 8 | 69.84 | 6 | 52.38 | 7 | 61.11 | 7 | 61.11 | 13 | 113.49 | 349 | 3046.70 |
| San Pablo-Santa Justa | 7936 | 0 | 0.00 | 10 | 126.01 | 2 | 25.20 | 2 | 25.20 | 3 | 37.80 | 1 | 12.60 | 12 | 151.21 | 2 | 25.20 | 97 | 1222.28 |
| Este | 19,479 | 2 | 10.27 | 46 | 236.15 | 7 | 35.94 | 11 | 56.47 | 21 | 107.81 | 6 | 30.80 | 17 | 87.27 | 25 | 128.34 | 543 | 2787.62 |
| Bellav-La Palmera | 7824 | 0 | 0.00 | 5 | 63.91 | 1 | 12.78 | 5 | 63.91 | 5 | 63.91 | 0 | 0.00 | 13 | 166.16 | 5 | 63.91 | 126 | 1610.43 |
| Remedios | 3570 | 0 | 0.00 | 4 | 112.04 | 2 | 56.02 | 2 | 56.02 | 4 | 112.04 | 0 | 0.00 | 2 | 56.02 | 1 | 28.01 | 37 | 1036.41 |
| With ASTN | 66,107 | 15 | 22.69 | 196 | 296.49 | 39 | 59.00 | 41 | 62.02 | 69 | 104.38 | 23 | 34.79 | 81 | 122.53 | 90 | 136.14 | 1975 | 2987.58 |
| Without ASTN | 40,315 | 2 | 4.96 | 67 | 166.19 | 13 | 32.25 | 23 | 57.05 | 26 | 64.49 | 5 | 12.40 | 54 | 133.95 | 30 | 74.41 | 685 | 1699.12 |
| Seville | 106,422 | 17 | 15.97 | 263 | 247.13 | 52 | 48.86 | 64 | 60.14 | 95 | 89.27 | 28 | 26.31 | 135 | 126.85 | 120 | 112.76 | 2660 | 2499.48 |
ASTN, area with social transformation needs; Bellav, Bellavista; GER, gastroesophageal reflux; HT, hypertrophy.
Overall and specific hospitalization rates for neonatal primary diagnoses in Seville (admissions/1000 births in 2014).
| Area | Population (born in 2014) | LBW-prematurity-IUGR | NB-maternal infection | ||
|---|---|---|---|---|---|
| District | n | Rate | n | Rate | |
| Casco Antiguo | 501 | 16 | 31.94 | 6 | 11.98 |
| Macarena | 650 | 30 | 46.15 | 0 | 0.00 |
| Nervión | 446 | 10 | 22.42 | 2 | 4.48 |
| Cerro-Amate | 895 | 49 | 54.75 | 13 | 14.53 |
| Sur | 655 | 21 | 32.06 | 5 | 7.63 |
| Triana | 353 | 8 | 22.66 | 2 | 5.67 |
| Norte | 726 | 28 | 38.57 | 1 | 1.38 |
| San Pablo-Santa Justa | 462 | 11 | 23.81 | 1 | 2.16 |
| Este | 1071 | 31 | 28.94 | 9 | 8.40 |
| Bellavista-La Palmera | 550 | 15 | 27.27 | 3 | 5.45 |
| Remedios | 230 | 3 | 13.04 | 0 | 0.00 |
| With ASTN | 3997 | 159 | 39.78 | 28 | 7.01 |
| Without ASTN | 2542 | 63 | 24.78 | 14 | 5.51 |
| Seville | 6539 | 222 | 33.95 | 42 | 6.42 |
IUGR, intrauterine growth restriction; NB, newborn, LBW, low birth weight.
Specific rate ratios by area with social transformation needs (rate in area with ASTNs/rate in areas without ASTNs).
| Primary diagnosis | Rate |
|---|---|
| Asthma | 4.6 |
| Bronchitis/bronchiolitis | 1.8 |
| Pneumonia | 1.8 |
| GER | 1.1 |
| Appendicitis | 1.6 |
| Inguinal hernia | 2.8 |
| Hypertrophy tonsils/adenoids | 0.9 |
| Epilepsy and seizures | 1.8 |
| LBWNB-preterm birth-IUGR | 1.6 |
| NB-maternal infection | 1.3 |
| All admissions | 1.8 |
Girls and boys residing in the lower socioeconomic level districts of Seville are admitted to the public referral hospitals more frequently, with a higher proportion of urgent admissions versus scheduled ones, and a lower mean age. Thus, place of residence does have an impact on some of the hospitalization characteristics of paediatric admissions, as well as in the rates of hospitalization for the most frequent reasons for admission.
These results are consistent with the literature, which has evidence of an increased frequency of paediatric admissions in patients of lower socioeconomic status.13,14,38 However, we did not find statistically significant differences in mean length of stay, conversely to other studies.26–28 Different studies have found contradictory evidence as regards the association between in-hospital mortality and socioeconomic status.25,26,29 In our study, in-hospital mortality was not associated with socioeconomic status.
Admissions were most frequent in patients aged less than 5 years (61.95%). The mean age at admission of children from districts with ASTNs was 7 months younger (p<0.001) and nearly 3 out of 4 of hospital admissions in this group were urgent (p<0.001). This could be explained by an increased morbidity or greater severity of disease, or by greater difficulties in the outpatient management of disease, especially for illnesses that depend more on this type of care, such as asthma.14 We did not find statistically significant differences in the analysis by sex of place or precedence or the primary diagnoses included in the study (with the exception of pneumonia, more frequent in girls), so we did not conduct a more detailed analysis based on sex.
Of the entire population of Seville aged less than 15 years, 62.1% lived in districts containing ASTNs, that is, those with lower socioeconomic level. To control for the effect of the unequal distribution of the paediatric population of the city on hospital admissions, we calculated the rate of hospitalization for the most frequent reasons for admission. The ratio for the overall hospitalization rate was higher in districts with lower socioeconomic level (1.8). The Macarena and Norte districts had the highest specific rates of hospitalization, with the Macarena district having the highest rate for 6 of the 10 primary diagnoses analyzed. All specific hospitalization rates in the analysis by district were greater in districts of lower socioeconomic level, except for the diagnosis of hypertrophy of the tonsils and/or adenoids. This difference was larger for diagnoses involving respiratory illness, inguinal hernia and epilepsy/convulsions, for which the specific hospitalization rates were equal to or exceeded the overall rate by ASTN. We ought to highlight the considerable difference we found in the rate of asthma-related admissions in patients from districts with a lower socioeconomic level (rate ratio=4.6), which is consistent with other studies.14,23,24 In opposition, we found smaller differences in the hospitalization rate ratios for diseases associated with invasive diagnostic and therapeutic procedures (gastroesophageal reflux, appendicitis and hypertrophy of tonsils and/or adenoids), except for inguinal hernia, which could be explained by its association with preterm birth, which is more common in districts with a lower socioeconomic level.
The Cerro-Amate district had the highest rate of admissions for the 2 neonatal diagnoses included in the study. As has been described in other studies,21,22,25 districts with lower socioeconomic levels had the highest rates of hospitalization for low birth weight, prematurity or IUGR. The predominance of the pattern of informal care that revolves around women in disadvantaged areas (where the burden of care is higher due to being in charge of a greater number of components), the stress caused by circumstances associated with economic adversity, the higher frequency of unskilled jobs that require greater physical exertion and difficulties in adhering to prenatal care are some of the factors that could explain this finding. As for admissions due to maternal infection, the absence or low number of observations of such admissions in some districts, and the fact that the hospital stay of newborns in the maternity ward is not documented as an admission, may have led us to underestimate the size of the difference for this diagnosis.
One of the limitations of our study is the exclusive use of data from the public hospitals in Seville, which may underestimate the rate of hospitalization in districts of a higher socioeconomic level. This limitation may have missed up to 16.1% of paediatric admissions in the city.39 The use of the postcode as the variable that defines place of residence has additional limitations, as the postal division of Seville does not completely match the administrative division. This may have contributed to selection bias, mainly in 3 out of the 20 postcodes of Seville. The use of large geographical units for the calculation of rates and the bivariate analysis may have underestimated the differences that exist between smaller geographical areas, such as neighbourhood or census sections, and especially those declared ASTNs.40 Last of all, the extrapolation of admission rates calculated with aggregate data may lead to the ecological fallacy.
This study is one of the few conducted in Spain that analyzes the impact of the place of residence as a socioeconomic factor in the main reasons for paediatric admission and, to our knowledge, the first that has taken place since the start of the current economic crisis. One of its strengths is the use of the CMBD as a data source, as it provides objectivity and comparability for future research. The records of the 2 referral hospitals of Seville provided a large number of admissions for the analysis, avoiding duplication and preserving the independence of observations by excluding readmissions. The availability of demographic data for the city37 facilitated the direct calculation of rates without the need for standardization. On the other hand, the definition and identification of ASTNs by the Department of Equality and Wellbeing of Andalusia (Consejería para la Igualdad y Bienestar de Andalucía)34 allowed us to use an official socioeconomic criterion.
The deleterious effects of poverty on the health of children are numerous, and they have long-lasting repercussions in their developing bodies.6,21,22 While we are aware that using paediatric hospitalisations as a method to evince this association excludes a considerable part of the health care spectrum, and especially primary care, this approach could provide a starting point to guide future lines of research on this subject. The role of paediatricians is essential in the identification, prevention and treatment of these consequences, but also in raising awareness in policy makers to prevent the impact of inequalities on health starting at such early ages.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank Dr José Sala Turrens for giving us access to the CMBD database of the Virgen del Rocío and Virgen Macarena hospitals (Seville), which was the main source of data for this study.
Please cite this article as: Tornero Patricio S, Charris-Castro L, Granero Asencio M, Daponte Codina A. Influencia del código postal en las hospitalizaciones pediátricas en Sevilla. An Pediatr (Barc). 2017;87:320–329.