Pertussis is a disease that has the most severe presentation in the first 6 months of life.1 Recently, there has been a progressive increase in the incidence of pertussis in developed countries, including severe cases in infants.2 This trend has spurred the implementation of new vaccination strategies to prevent pertussis, such as vaccination of pregnant women in the third trimester of gestation. This is the most cost-effective strategy to prevent severe cases in infancy.3 Vaccination of pregnant women prevents between 78% and 91% of cases of pertussis in infants aged less than 2 months4 and is 90% effective in preventing hospital admission.5 In February 2015, the Basque Country introduced routine vaccination of all pregnant women in the region, and the vaccination coverage rate achieved since has been estimated at 80%.6
The aim of our study, approved by the Ethics Committee of our hospital (CEIC Code EI5/32), was to analyse the impact of vaccination of pregnant women against pertussis on the resurgence of this disease and the severity of disease in the paediatric emergency department (PED) of a tertiary care hospital.
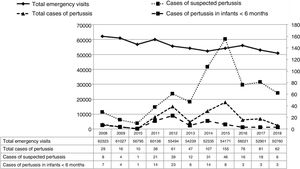
We conducted a retrospective cohort study between 2008 and 2018 in the PED of a tertiary care hospital that manages approximately 55 000 emergency visits a year of children aged less than 14 years. We compared the characteristics and discharge destination of patients with a microbiological diagnosis of pertussis (species-specific polymerase chain reaction [PCR] and/or culture in Bordet agar until 2015 and species-specific PCR thereafter) before and after the introduction of routine vaccination of pregnant women. The indications to request microbiological testing for confirmation were clinical (clinical suspicion in patients aged 0–14 years by the physician in charge, independently of patient age and the clinical presentation), and there were no changes in the criteria for ordering these tests during the study period. We defined the January 2008 to July 2015 interval as the prevaccination period, the last six months of 2015 as the window period and the 3-year interval from 2016 to 2018 the postvaccination period. We defined the impact on the resurgence of pertussis as the change in the episodes of pertussis with microbiological confirmation (and specifically in episodes in infants aged less than 6 months) and the change in the associated hospital admission rate.
During the period under study, there were 616 204 emergency visits, out of which 202 corresponded to cases of pertussis with microbiological confirmation (0.03%; 95% confidence interval [CI], 0.03−0.04), none diagnosed exclusively based on a positive culture in Bordet agar: 147 (73.1%) in the prevaccination period, 15 (7.5%) in the window period and 40 (19.8%) in the postvaccination period. There were more cases of pertussis diagnosed in the prevaccination period: 1.1 cases per 10 000 recorded visits to the PED in 2008 compared to 8.5 per 10 000 visits in 2015. This rate decreased to 2.1 cases per 10 000 visits in the postvaccination period. Of the 202 patients with a microbiological diagnosis of pertussis, 86 were infants aged less than 6 months (42.8%): 74 in the prevaccination period (50.3% of the cases of pertussis diagnosed during this period), 3 cases (20%) in the window period and 9 in the postvaccination period (22.5% of the total cases diagnosed in the postvaccination period, a significant decrease compared to the prevaccination period; P < .01). The mothers of 6 of the 9 previously healthy patients aged less than 6 months given a diagnosis of pertussis in the postvaccination period (66.7%) had been vaccinated during pregnancy. In addition, there was a change in the number of orders of microbiological tests for confirmation of pertussis: there was a substantial increase through the prevaccination period followed by a decrease after introduction of routine vaccination of pregnant women, although it did not reach the initial level of the prevaccination period (Fig. 1). One possible explanation is that severe cases in infants, while having decreased significantly in frequency, have not been eradicated and physicians maintained a higher level of suspicion in the postvaccination period. Overall, 62 patients were admitted to hospital, 58 in the prevaccination period (39.5% of cases of pertussis diagnosed in the same period) and 4 in the postvaccination period (10% of cases of pertussis diagnosed in the same period; P < .01).
The sole difference in the clinical presentation of pertussis between the pre- and the postvaccination periods was the increase in the age of patients with a diagnosis of pertussis in the postvaccination period (median age, 29 months vs 5 months in the prevaccination period; P < .05) (Table 1). A boy aged 1 month died in the prevaccination period of malignant pertussis. The rest had favourable outcomes free of sequelae.
Characteristics of patients given a diagnosis of pertussis before and after the introduction of routine vaccination of pregnant women.
| Pertussis cases, prevaccination period | Pertussis cases, postvaccination period | P | |
|---|---|---|---|
| N = 147 (100%) | N = 40 (100%) | ||
| Age in months (median) | 5 | 29 | < .01 |
| Sex (male); n (%) | 69 (46.9) | 19 (47.5) | NS |
| Cases < 6 months; n (%) | 74 (50.3) | 9 (22.5) | < .01 |
| Complete vaccination status; n (%) | 112 (76.2) | 37 (92.5) | NS |
| Preterm birth; n (%) | 4 (2.7) | 2 (5) | NS |
| Cases in family; n (%) | 20 (13.6) | 8 (20) | NS |
| [0,1–4] | |||
| [0,1–4]Symptoms | |||
| Cough; n (%) | 147 (100) | 40 (100) | NS |
| Fever; n (%) | 17 (11.6) | 3 (7.5) | NS |
| Respiratory distress; n (%) | 30 (20.4) | 4 (10) | NS |
| Apnoea; n (%) | 24 (16.3) | 4 (10) | NS |
| Change in colour; n (%) | 100 (68) | 24 (60) | NS |
| Loss of consciousness; n (%) | 2 (1.4) | 2 (5) | NS |
| Vomiting; n (%) | 53 (36.1) | 19 (47.5) | NS |
| [0,1–4] | |||
| [0,1–4]Physical examination | |||
| General malaise; n (%) | 3 (2) | 1 (2.5) | NS |
| Respiratory distress; n (%) | 13 (8.8) | 1 (2.5) | NS |
| Abnormal findings of auscultation; n (%) | 20 (13.6) | 1 (2.5) | NS |
| Change in colour; n (%) | 2 (1.4) | 1 (2.5) | NS |
| [0,1–4] | |||
| Admission | 58 (39.5) | 4 (10) | < .01 |
| Ward; n (%) | 46 (31.3) | 4 10) | |
| Intensive care unit; n (%) | 12 (8.2) | 0 (0) | |
| [0,1–4] | |||
| [0,1–4]Length of stay (median) | |||
| Ward | 9 | 7.5 | NS |
| Intensive care unit | 11.5 | ||
| Repeat visit; n (%) | 20 (12.7) | 8 (20) | NS |
NS, not significant.
Data expressed as absolute frequencies and percentages.
The main limitations of our study are that it was conducted in a single hospital and the limitations intrinsic to its retrospective design. Nevertheless, since that all visits are recorded in the digital records database, including the electronic health records of patients and the notes entered in patient charts regarding the course of disease and the subsequent follow-up, the quality of the collected data was good. Although caution should be exerted in extrapolating our findings to other settings or populations, they could be valid for populations with similar demographic characteristics in a similar health care environment.
Our study confirms that the routine vaccination of pregnant women has reversed the resurgence of pertussis by reducing the number of cases in infants aged less than 6 months and the number of associated hospital admissions.5
We take this opportunity to thank Dr Alaitz Urtiaga.
Please cite this article as: Gangoiti I, Martinez-Fernandez E, Garmendia O, Diez A, Mintegi S. Impacto de la vacunación en embarazadas sobre la reemergencia de la tosferina y su forma de presentación en urgencias. An Pediatr (Barc). 2020;93:129–131.
Previous presentations: This study was presented at the XXIV Annual Meeting of the Sociedad Española de Urgencias de Pediatría and the 67th Congress of the Asociación Española de Pediatría.