Hypersensitivity reactions to non-steroidal anti-inflammatory drugs (NSAIDs) are the most common reactions to drugs. The prevalence varies from 0.6 to 5.7% in the general population, but there are no data available in children. The aim of this study is to determine the frequency of patients diagnosed with hypersensitivity to NSAIDs, and describe their clinical characteristics, type of hypersensitivity, and tolerance to alternative drugs.
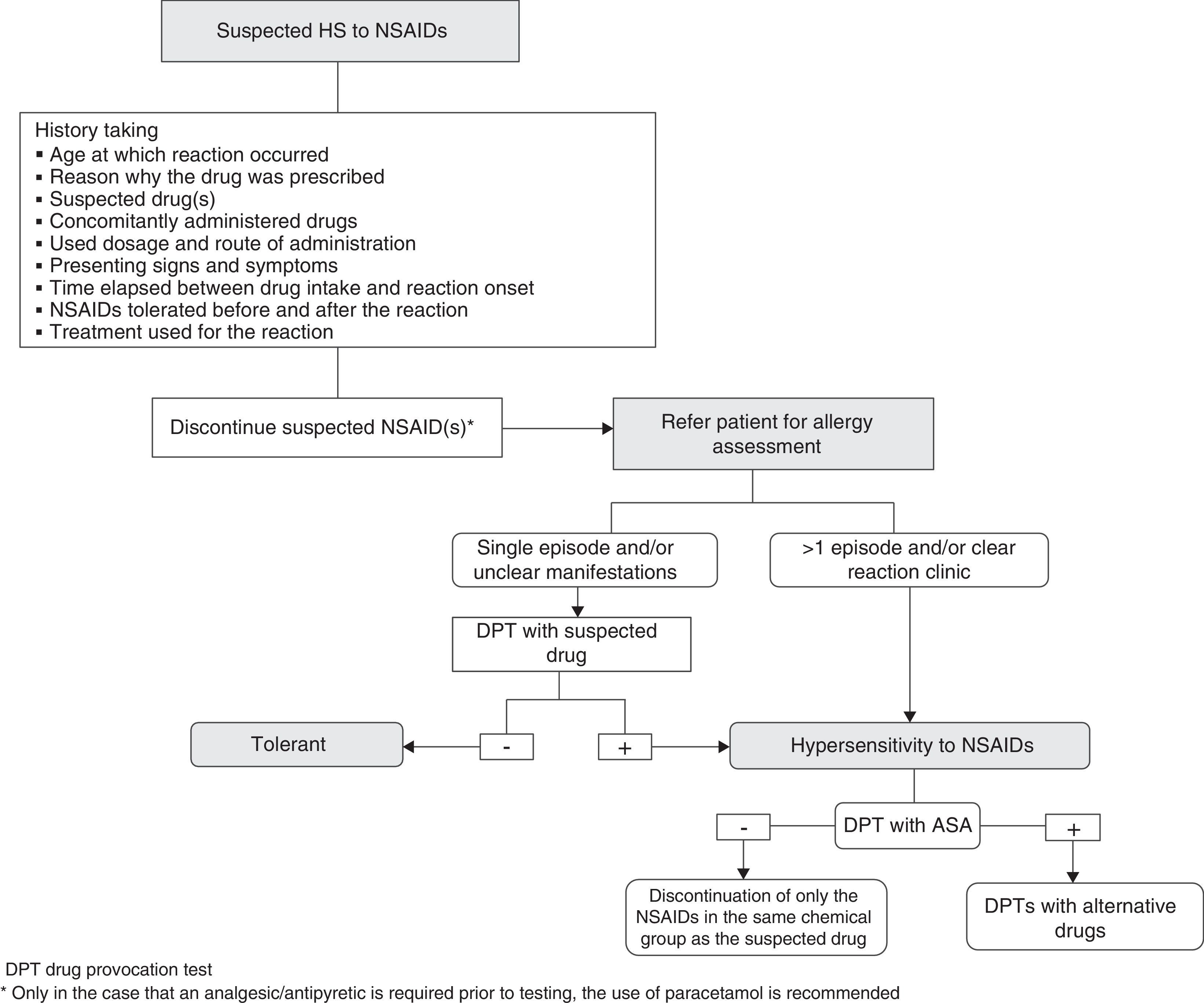
MethodsA retrospective study was conducted on children with suspected hypersensitivity to NSAIDs from January 2012 to December 2013. The diagnosis was confirmed by oral drug provocation test (DPT) to the drug involved in the group with a history of one episode, while in the group with a history of more than one episode with the same drug the diagnosis was based on clinical data. Subsequently, a DPT with acetylsalicylic acid (ASA) was done in order to classify hypersensitivity into selective or multiple. In those cases with a positive result, a DPT was performed with alternative drugs.
ResultsOut of a total of 93 children studied, 26 were diagnosed with hypersensitivity to NSAIDs: 7 confirmed by oral DPT, and 19 based on clinical data. Multiple hypersensitivity was diagnosed in 50% of patients. Ibuprofen was involved in all reactions. The most common clinical manifestation was angioedema (44%). Acetaminophen was the best tolerated alternative drug.
ConclusionsMore than one quarter (28%) of the population studied was diagnosed with hypersensitivity to NSAIDs, and 50% had multiple hypersensitivity. Acetaminophen is a safe alternative in children with hypersensitivity to NSAIDs. Meloxicam may be an alternative in cases that do not tolerate acetaminophen.
Las reacciones de hipersensibilidad (HS) a los antiinflamatorios no esteroideos (AINE) son las reacciones a drogas más frecuentes. Su prevalencia en la población general varía del 0,6 al 5,7%, no teniendo datos en niños. El objetivo de este estudio fue determinar la frecuencia de pacientes diagnosticados de HS a AINE, características clínicas, tipo de HS y tolerancia a fármacos alternativos.
Material y métodosEstudio descriptivo retrospectivo de niños con sospecha de HS a AINE realizado entre enero de 2012 y diciembre de 2013. El diagnóstico se realizó mediante prueba de exposición controlada (PEC) al fármaco implicado cuando tenían historia de episodio único, y basado en la clínica si había habido más de un episodio con un mismo fármaco. Posteriormente se realizó una PEC al ácido acetilsalicílico, para diferenciar en HS selectiva o múltiple. En los casos con resultado positivo se hizo una PEC a fármacos alternativos.
ResultadosSe estudiaron 93 niños, de los que 26 fueron diagnosticados de HS a AINE (7 confirmados mediante PEC y 19 basados en la clínica). Un 50% presentó HS múltiple. El ibuprofeno estuvo involucrado en todas las reacciones. La clínica observada con mayor frecuencia en la PEC fue el angioedema (44%). El paracetamol fue el fármaco alternativo mejor tolerado.
ConclusionesUn 28% de la población estudiada fue diagnosticada de HS a AINE, y el 50% presentó una HS múltiple. El paracetamol es una alternativa segura en niños con HS a AINE. El meloxicam podría considerarse como una alternativa en los casos que no toleran el paracetamol.
Hypersensitivity reactions (HRs) to nonsteroidal anti-inflammatory drugs (NSAIDs) are the most frequently reported reactions to drugs, followed by reactions to beta-lactam antibiotics, and less frequently to other drugs.1,2 The prevalence varies in the different published series; ranging from about 0.6% to 5.7% in the general population, with no data published for the paediatric age group. According to the nomenclature of the EAACI-WAO, HS reactions to NSAIDs may be classified into allergic (mediated by an immunological mechanism) and non-allergic (non-immunological mechanism),3 with the latter being more frequent. The mechanism of action of NSAIDs involves inhibition of cyclooxygenase 1 (COX-1) and/or cyclooxygenase 2 (COX-2), depending on the group they belong to, and it has been proposed that the mechanism underlying reactions to NSAIDs is an impairment in the inhibition of COX-1 that results in the low production of prostaglandin E2 and an associated increase in the synthesis and release of cysteinyl leukotrienes, the latter of which would be responsible for the clinical and histological manifestations observed in these patients.4 Reactions can be classified based on the onset time after drug intake into immediate or delayed,3 and based on the chemical group to which the NSAIDs belong into selective HS when the reaction is elicited by one or several chemically related NSAIDs, and multiple HS when the reaction is elicited by at least two NSAIDs belonging to different chemical groups.2
The aim of this study was to determine the frequency of children that receive a diagnosis of HS to NSAIDs and to analyse their clinical features, type of HS, and tolerance to alternative drugs.
Materials and methodsPatientsWe conducted a retrospective descriptive study of children with suspected HS to NSAIDs that received care at the allergy department of the Hospital Sant Joan de Déu of Barcelona between January 2012 and December 2013. The study included patients aged 1–18 years with a history of reactions such as exanthema, urticaria, angioedema, rhinitis, asthma, or anaphylaxis associated with NSAID intake.
DiagnosisThe patients were separated into two groups to determine their diagnosis. The first group included those patients with a single episode that underwent a DPT with the suspected drug, and the second group the patients with a history of more than one episode caused by a single drug diagnosed with HS to NSAIDs based on clinical data (history of clear reactions) that did not undergo DPT with the suspected drug or drugs.
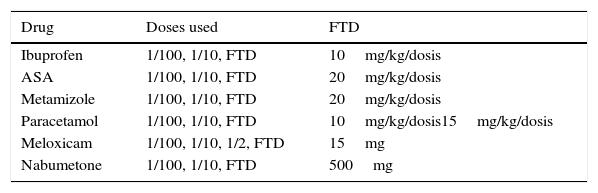
Drug provocation tests were performed in the inpatient department under the supervision of an expert allergist and consisted in the oral administration of the drug at increasing doses, given at least 90min apart, until the full therapeutic dose (FTD; mg/kg/dose) was reached (Table 1). In patients with a history of respiratory symptoms, spirometry was performed prior to initiating the test, considering a baseline FEV1 of at least 70% of the predicted value as normal. Spirometry was repeated before each of the dose increases. After completion of the test, patients were kept under observation for 6h, during which they were tested by spirometry every 2h.
NSAIDs assessed by means of a drug provocation test (DPT).
| Drug | Doses used | FTD |
|---|---|---|
| Ibuprofen | 1/100, 1/10, FTD | 10mg/kg/dosis |
| ASA | 1/100, 1/10, FTD | 20mg/kg/dosis |
| Metamizole | 1/100, 1/10, FTD | 20mg/kg/dosis |
| Paracetamol | 1/100, 1/10, FTD | 10mg/kg/dosis15mg/kg/dosis |
| Meloxicam | 1/100, 1/10, 1/2, FTD | 15mg |
| Nabumetone | 1/100, 1/10, FTD | 500mg |
ASA, acetylsalicylic acid; FTD, full therapeutic dose.
The DPT was considered positive if the patient developed any of the following signs or symptoms: (a) cutaneous (urticaria, angioedema); (b) respiratory (rhinorrhoea, nasal congestion, conjunctivitis or asthma); (c) a decline of at least 15% in FEV1 detected by spirometry, and (d) anaphylaxis.
Selective versus multiple hypersensitivityTo determine the type of HS, the patients underwent a DPT with acetylsalicylic acid (ASA) or, if they had a previous history of a reaction to ASA, to a different potent COX-1 inhibitor. Hypersensitivity was classified as selective if the patient reacted to one or more NSAIDs belonging to the same chemical group, and as multiple if the patient reacted to two or more chemically nonrelated NSAIDs.
Tolerance to alternative drugsFinally, patients underwent DPTs to drugs considered to be safe alternatives, such as paracetamol or meloxicam. If patients could tolerate low doses of paracetamol, their tolerance to high doses was also assessed.
ResultsWe analysed a total of 93 patients in whom HS to NSAIDs was suspected, out of which the diagnosis was confirmed in 26 (28%), while 66 (71%) tolerated the suspected drug in the DPT. One patient was excluded from the study because he had poorly controlled asthma.
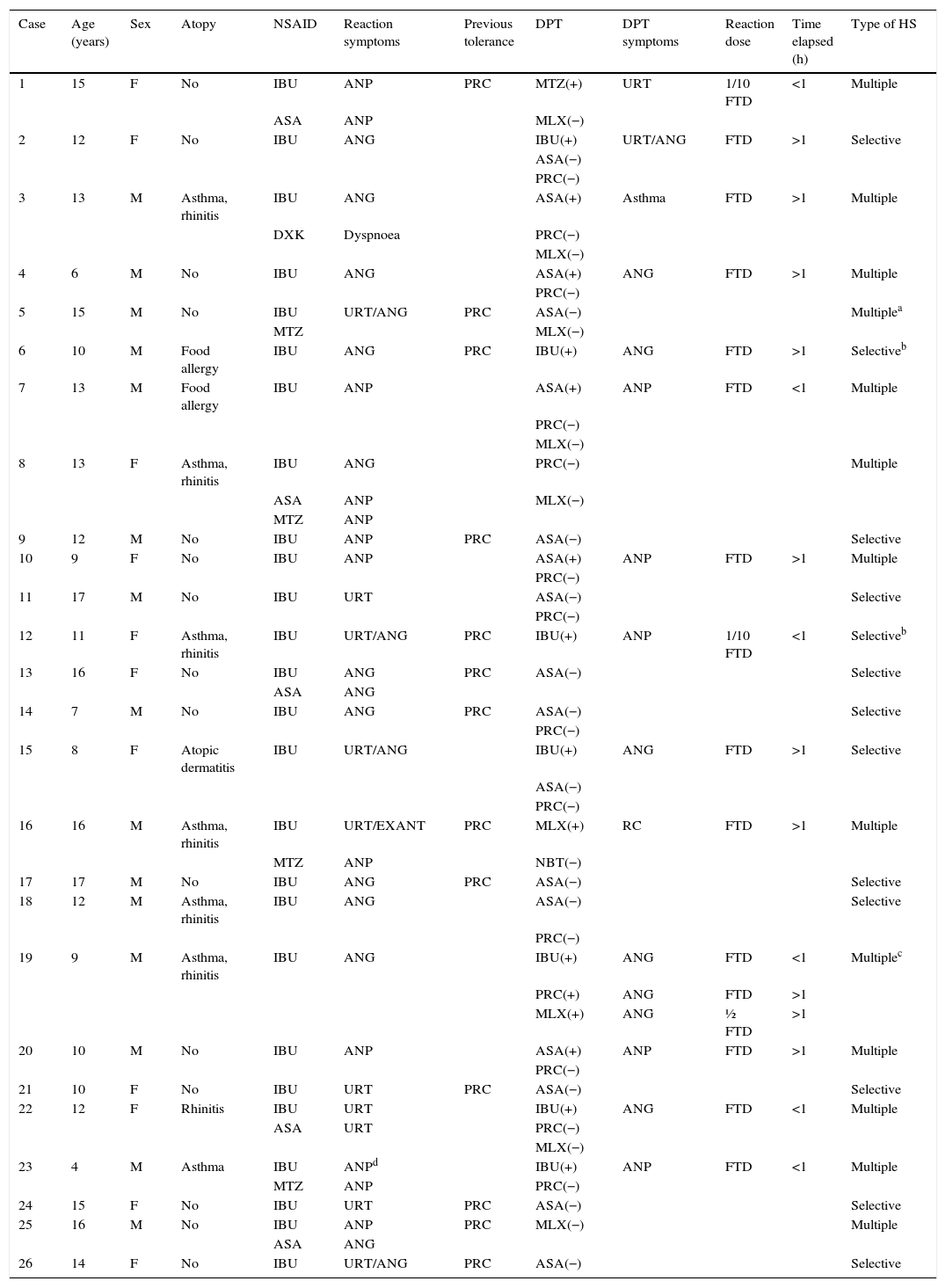
Of the 26 patients with HS, 42% were female and 58% male; their mean age was 12 years (range, 4–17 years); 17 reported having had some type of reaction after intake of a single NSAID and nine to two or more NSAIDs; ibuprofen was involved in all reactions, in addition, four patients reported having reacted to ASA, three to metamizole, one to dexketoprofen and one to ASA and metamizole.
Diagnosis of hypersensitivity to nonsteroidal anti-inflammatory drugsA total of 7 (27%) patients received a diagnosis of HS to NSAIDs confirmed by a DPT with the suspected drug, and 19 (73%) based on clinical data.
Drug provocation testForty-nine DPTs were performed: 8 with the suspected drug (7 with ibuprofen and one with ASA), 17 with a potent COX-1 inhibitor (16 with ASA and 1 with metamizole) and 24 with alternative drugs (14 with paracetamol, 9 with meloxicam, 1 with nabumetone in a patient that did not tolerate the other two alternatives).
Of all the tests performed, 16 (32.7%) were positive: seven with ibuprofen, five with ASA, two with meloxicam, one with metamizole and one with paracetamol.
Half of the patients were classified as having multiple HS and the other half as having selective HS (Table 2).
Patients that received a diagnosis of hypersensitivity to NSAIDs.
| Case | Age (years) | Sex | Atopy | NSAID | Reaction symptoms | Previous tolerance | DPT | DPT symptoms | Reaction dose | Time elapsed (h) | Type of HS |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 15 | F | No | IBU | ANP | PRC | MTZ(+) | URT | 1/10 FTD | <1 | Multiple |
| ASA | ANP | MLX(−) | |||||||||
| 2 | 12 | F | No | IBU | ANG | IBU(+) | URT/ANG | FTD | >1 | Selective | |
| ASA(−) | |||||||||||
| PRC(−) | |||||||||||
| 3 | 13 | M | Asthma, rhinitis | IBU | ANG | ASA(+) | Asthma | FTD | >1 | Multiple | |
| DXK | Dyspnoea | PRC(−) | |||||||||
| MLX(−) | |||||||||||
| 4 | 6 | M | No | IBU | ANG | ASA(+) | ANG | FTD | >1 | Multiple | |
| PRC(−) | |||||||||||
| 5 | 15 | M | No | IBU | URT/ANG | PRC | ASA(−) | Multiplea | |||
| MTZ | MLX(−) | ||||||||||
| 6 | 10 | M | Food allergy | IBU | ANG | PRC | IBU(+) | ANG | FTD | >1 | Selectiveb |
| 7 | 13 | M | Food allergy | IBU | ANP | ASA(+) | ANP | FTD | <1 | Multiple | |
| PRC(−) | |||||||||||
| MLX(−) | |||||||||||
| 8 | 13 | F | Asthma, rhinitis | IBU | ANG | PRC(−) | Multiple | ||||
| ASA | ANP | MLX(−) | |||||||||
| MTZ | ANP | ||||||||||
| 9 | 12 | M | No | IBU | ANP | PRC | ASA(−) | Selective | |||
| 10 | 9 | F | No | IBU | ANP | ASA(+) | ANP | FTD | >1 | Multiple | |
| PRC(−) | |||||||||||
| 11 | 17 | M | No | IBU | URT | ASA(−) | Selective | ||||
| PRC(−) | |||||||||||
| 12 | 11 | F | Asthma, rhinitis | IBU | URT/ANG | PRC | IBU(+) | ANP | 1/10 FTD | <1 | Selectiveb |
| 13 | 16 | F | No | IBU | ANG | PRC | ASA(−) | Selective | |||
| ASA | ANG | ||||||||||
| 14 | 7 | M | No | IBU | ANG | PRC | ASA(−) | Selective | |||
| PRC(−) | |||||||||||
| 15 | 8 | F | Atopic dermatitis | IBU | URT/ANG | IBU(+) | ANG | FTD | >1 | Selective | |
| ASA(−) | |||||||||||
| PRC(−) | |||||||||||
| 16 | 16 | M | Asthma, rhinitis | IBU | URT/EXANT | PRC | MLX(+) | RC | FTD | >1 | Multiple |
| MTZ | ANP | NBT(−) | |||||||||
| 17 | 17 | M | No | IBU | ANG | PRC | ASA(−) | Selective | |||
| 18 | 12 | M | Asthma, rhinitis | IBU | ANG | ASA(−) | Selective | ||||
| PRC(−) | |||||||||||
| 19 | 9 | M | Asthma, rhinitis | IBU | ANG | IBU(+) | ANG | FTD | <1 | Multiplec | |
| PRC(+) | ANG | FTD | >1 | ||||||||
| MLX(+) | ANG | ½ FTD | >1 | ||||||||
| 20 | 10 | M | No | IBU | ANP | ASA(+) | ANP | FTD | >1 | Multiple | |
| PRC(−) | |||||||||||
| 21 | 10 | F | No | IBU | URT | PRC | ASA(−) | Selective | |||
| 22 | 12 | F | Rhinitis | IBU | URT | IBU(+) | ANG | FTD | <1 | Multiple | |
| ASA | URT | PRC(−) | |||||||||
| MLX(−) | |||||||||||
| 23 | 4 | M | Asthma | IBU | ANPd | IBU(+) | ANP | FTD | <1 | Multiple | |
| MTZ | ANP | PRC(−) | |||||||||
| 24 | 15 | F | No | IBU | URT | PRC | ASA(−) | Selective | |||
| 25 | 16 | M | No | IBU | ANP | PRC | MLX(−) | Multiple | |||
| ASA | ANG | ||||||||||
| 26 | 14 | F | No | IBU | URT/ANG | PRC | ASA(−) | Selective |
ASA, acetylsalicylic acid; ANP, anaphylaxis; ANG: angioedema; FTD, full therapeutic dose; DXK, dexketoprofen; EXANT, exanthema; IBU, ibuprofen; MLX, meloxicam; MTZ, metamizole; NBT, nabumetone; PRC, paracetamol; RC: rhinoconjunctivitis; URT, urticaria.
Case 5 received a diagnosis of multiple HS despite tolerating ASA in the DPT due to a previous history of episodes associated with metamizole.
The DPT with ASA was not performed in cases 6 and 12, so the diagnosis of selective HS is provisional.
The clinical manifestations observed during DPTs were angioedema (7), anaphylaxis (5), urticaria (1), asthma (1), rhinoconjunctivitis (1) and angioedema and urticaria (1); all reactions, including anaphylactic ones, were mild and were controlled with the administration of an antihistamine (hydroxyzine) and an oral corticosteroid (prednisone or prednisolone); none of the patients required adrenaline. Thirteen children reacted to the FTD, one to half of the FTD, and two to 1:10 of the FTD. The time elapsed between drug intake and the onset of the reaction was less than 1h in seven children and more than 1h in nine.
Previous history of atopyEleven patients had a history of atopy: asthma and rhinitis (6); food allergy (2); asthma (1); atopic dermatitis (1); seven of them belonged to the multiple HS group and four to the selective HS group.
DiscussionIn this study, we found that only 28% of the children that were assessed for a suspected HS to NSAIDs received such a diagnosis. Prior to the assessment, 30% reported having had reactions to more than one NSAID, yet 50% received a diagnosis of multiple HS after testing, which demonstrates the importance of performing DPTs not only as a means of confirming the diagnosis, but also to determine potential cross-reactivity and tolerance to other NSAIDs.3,5
Ibuprofen was the culprit drug in all reactions, consistent with other studies performed in children1,6; this finding may be due to the fact that this is one of the most frequently used NSAIDs in the paediatric age group.
All patients tolerated paracetamol except for one patient diagnosed with multiple HS. Other studies on children have also demonstrated that this drug is well tolerated, and consider it a safe alterantive5,7; however, a clinical phenotype of patients with multiple HS to NSAIDs has been described in the literature in which up to 25% may not tolerate weak COX-1 inhibitors, especially at high doses,3 so it is important to ascertain that the patient can tolerate low as well as high doses. One study of 24 Asian children with a previous history of atopy and a diagnosis of multiple HS to NSAIDs found that 25% could not tolerate paracetamol.8 There seems to be an association between multiple HS with a history of atopy and poor tolerance to paracetamol, and it is believed that genetic factors may be at play in its pathogenesis.2 In our study, 42% of patients had a previous history of atopy, especially of allergic respiratory disease, with a mild predominance of patients with multiple HS.
Other drugs that were evaluated as alternatives for patients with multiple HS were selective COX-2 inhibitors; studies conducted in adults have demonstrated that they are well tolerated by most patients and that they can be considered as an alternative for those that do not tolerate paracetamol9; one study in forty-one children aged 9–14 years assessed tolerance to meloxicam and found reactions in two patients.10 In our study, nine out of thirteen patients with multiple HS underwent a DPT with meloxicam, and two could not tolerate it; while there is still insufficient evidence for the paediatric age group, meloxicam could be considered an alternative in patients with multiple HS that cannot tolerate paracetamol.
Another drug that we evaluated as an alternative for a patient that did not tolerate meloxicam was nabumetone; a study in adults found that it was tolerated by 93% of patients with multiple HS,11 although there are no studies on its use in children.
Angioedema was the most common clinical reaction observed during the provocation tests, consistent with similar findings in other published case series.1,8
To conclude, 28% of the sample under study was diagnosed with HS to NSAIDs, and, of those, 50% had multiple HS. Paracetamol may be considered a safe alternative, as it was tolerated by 96.2% of the children; however, tolerance to it must be confirmed by a DPT. Meloxicam may be an option in patients that do not tolerate paracetamol; however, we must note that its use is not indicated in children younger than 15 years. While HS reactions to NSAIDs are the most frequent adverse reactions in the general population, they tend to be underestimated in everyday practice, as they may be attributed to antibiotics that are being used concomitantly or even to some infectious agents, resulting in the delayed referral of these patients for assessment after having had more than one episode caused by a single drug. This was corroborated by our study, in which 73% of the patients diagnosed with HS to a NSAID had had more than one episode with the same drug and a clear reaction history; for this reason, we propose a simple practical algorithm in case HS to a NSAID is suspected that may be helpful to primary care physicians (Fig. 1).
At present there are not enough studies on HS to NSAIDs in children and on safe alternatives, so the management of these patients remains a challenge.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Calvo Campoverde K, Giner-Muñoz MT, Martínez Valdez L, Rojas Volquez M, Lozano Blasco J, Machinena A, et al. Reacciones de hipersensibilidad a antiinflamatorios no esteroideos y su tolerancia a fármacos alternativos. An Pediatr (Barc). 2016;84:148–153.
Previous presentation: This study was presented at the XXXVIII Congreso de la Sociedad Española de Inmunología Clínica, Alergología y Asma Pediátrica; May 2014; Madrid, Spain.