Juvenile dermatomyositis (JDM) and scleroderma are two systemic autoimmune diseases that, in more than 70% of cases, cause gastrointestinal (GI) symptoms, such as dysphagia, heartburn or upper GI bleeding. In both diseases, GI involvement is associated with a poor prognosis,1,2 and in a substantial proportion of cases it is only initially detectable through the assessment of oesophageal motility.
At present, high-resolution oesophageal manometry (HROM) is the gold standard for assessment of complex oesophageal motility disorders. It is a painless technique that does not require sedation or hospital admission. It consists in the assessment of the neuromuscular activity involved in the functioning of the oesophagus from the hypopharynx to the cardias. The results are interpreted according to the Chicago classification of oesophageal motility disorders, version 4.0. High-resolution manometry and the Chicago classification have allowed the fine-tuning and standardization of the diagnosis of oesophageal motility disorders.3
To date, the literature on GI involvement in these two paediatric diseases is scarce, with even less data available for the abnormalities detected in diagnostic tests such as HROM. Some studies have found that abnormal oesophageal motility in JDM or scleroderma was associated with a poor prognosis and with disease progression.4–6
Therefore, testing for assessment of GI involvement is recommended at the time of diagnosis to establish the baseline and also during the follow-up to allow early adjustment of treatment in these patients.
In light of the above, our objective was to analyse oesophageal involvement by means of HROM in patients with JDM and scleroderma.
We conducted a retrospective review of the health records of patients with JDM or scleroderma managed in our hospital assessed with HROM between January 2018 and December 2022.
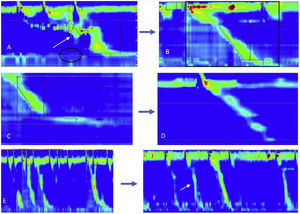
The study included 9 patients (5 cases of JDM; 4 cases of scleroderma, out of which 3 were systemic and 1 localised), 8 were female, the median age of onset was 9 years and the median time elapsed from onset to diagnosis was 2 months. Only one patient with JDM had reported symptoms at the time of diagnosis (dysphagia with consumption of solids), while another 2 (1 with JDM and 1 with scleroderma) developed symptoms during the follow-up (dysphagia only with solids, heartburn). The HROM, performed at the time of diagnosis in every case, weas abnormal in 8 patients (normal in only 1 patient with JDM). The most frequent abnormalities in both groups were: ineffective oesophageal motility (66%), hypotensive lower oesophageal sphincter tone (33%) and significant increase in tertiary contraction waves (66%). Three patients (2 with JDM and 1 with scleroderma) underwent a second HROM assessment with a median time of 2 years elapsed from diagnosis. In the patient with scleroderma, the manometric findings normalised after treatment. When it came to the patients with JDM, there were no changes in one, while in the other, manometry evinced worsening of oesophageal motility that was consistent with the worsening of symptoms (Fig. 1).
Patient 1 (A), (B): female patient in whom the follow-up assessment evinced improvement of symptoms, and the HROM at diagnosis (A) showed a hypotensive sphincter tone with tertiary contraction waves, with the patient requiring several swallowing attempts to move the bolus. The follow-up manometry (B) showed a normal lower oesophageal sphincter and a decrease in tertiary contraction waves, and the patient was able to push the bolus appropriately with a single swallow, with visualization of a peristaltic wave. Patient 2 (C), (D): male patient whose symptoms were stable at the time of the follow-up visit, in whom the follow-up HROM (D) did not evince any significant differences compared to the HROM assessment at diagnosis (C). Patient 3 (E), (F): female patient that reported worsening of symptoms in the follow-up visit, with more severe dysphagia and coughing upon consumption of liquids. The follow-up HROM (F) evinced an increase in tertiary contractions.
The evidence we have presented shows that even when asymptomatic, patients with JDM or scleroderma frequently have features of impaired oesophageal motility on HROM. These findings are novel and there is no similar evidence in the literature, so our hospital has decided to undertake a prospective study to increase our knowledge about the changes in oesophageal motility in patients with these diseases, both at diagnosis and after initiation of appropriate treatment. This will allow us to determine whether high-resolution manometry can be useful for the early detection of disease progression and for treatment optimization.
Previous meetings: This study was presented as an oral communication at the XVII Annual Meeting of the Asociación de cirujanos pediátricos de Andalucía (ACPA), November 25–26, 2022, Almería, Spain (https://www.acpa-andalucia.com/_files/ugd/f903c6_35db2d067fd74e80a98ddb532beba0f2.pdf%20XV%20congreso%20de%20la%20Sociedad%20Española%20de%20Reumatología%20pediátrica%20(SERPE)), and as a poster (which received an award) at the XV Congress of the Sociedad Española de Reumatología pediátrica (SERPE), November 24–26, 2022, Bilbao, Spain (https://serpe2022.com/esquema-programa/).