It has been postulated that migration could act as a modifying factor in the incidence of type 1 diabetes mellitus (T1DM), so the aim of this study is to determine if there are differences in the incidence of T1DM by origin.
Material and methodsRetrospective study of cases of T1DM onset in the population younger than 19 years old in Osona and Baix Camp between 2000 and 2012, using the medical histories of endocrinology units of the health centres and demographics from Catalonia Statistical Institute as sources.
ResultsThe child population in Osona and Baix Camp increased by 36.6%, with 18.9% in the local population, and 482% in the immigrant population, and most of this increase (90%) in the Maghreb immigrant group. A total of 118 diabetics onset were found, 66.9% in the local population, 32.2% Maghrebi population, and 0.9% in children from other countries, with a total incidence rate of 14.4 cases per 100,000 population/year (c/105p-y). The incidence is higher in the Maghrebi population compared to the local population, 37.1 vs 11.2 c/105p-y (P<.001), and in children under 5 years compared to the 5–18 years group, 18.9 vs 12.5 c/105p-y (P<.05), with no differences between sexes (P>.05). The relative risk is 3.1 for the Maghrebi population, and 1.5 for children under 5 years.
ConclusionsThe total incidence of T1DM remains stable, but is higher in the Maghrebi than in the local population, and in children under 5 years compared to 5–18 years group. These results open a study field of which risk factors could be affecting this immigrant population in their destination countries.
Se ha postulado que la migración podría actuar como factor modificador de la incidencia de diabetes tipo 1 (DM1), por lo que el objetivo de este estudio es determinar si existen diferencias en la incidencia de DM1 según el origen.
Material y métodosEstudio retrospectivo de los casos de debut diabético tipo 1 en menores de 19 años en las comarcas de Osona y Baix Camp entre los años 2000 y 2012, utilizando la historia clínica de las unidades de endocrinología y los datos demográficos del Institut d¿Estadística de Catalunya.
ResultadosLa población infantil en Osona y el Baix Camp aumentó un 36,6%, un 18,9% los autóctonos y un 482% los inmigrantes, a expensas mayoritariamente del colectivo magrebí (90%). Han acontecido 118 debuts diabéticos, 66,9% en nativos, 32,2% en magrebíes y 0,9% en niños de otros países, con una tasa de incidencia total de 14,4 casos/100.000 habitantes/año (c/105 h-a). La incidencia es mayor en magrebíes respecto a autóctonos, 37,1 vs. 11,2 c/105 h-a (p<0,001), y en menores de 5 años respecto a los de 5 a 18 años, 18,9 vs. 12,5 (p<0,05), sin observar diferencias entre sexos (p>0,05). El riesgo relativo es 3,1 para magrebíes y 1,5 para menores de 5 años.
ConclusionesLa incidencia total de DM1 se mantiene estable, pero es mayor en magrebíes que en nativos y en menores de 5 años respecto a los de 5–18 años. Estos resultados abren un campo de estudio sobre los factores de riesgo que podrían estar incidiendo sobre esta población en los países de destino.
In the past two decades, we have experienced large migratory movements in Europe as well as in Spain, leading to an increase in the immigrant population that has been associated with changes in health care. Most of the immigrant population comes from regions with a lower incidence of type 1 diabetes mellitus (T1DM) than that of Spain, so we were interested in analysing the changes in the incidence of this disease in the period corresponding to this spike in immigration, and specifically in two regions in Catalonia: Osona, located inland in a plain 499m above sea level with continental weather and persistent fog during the winter, and the Baix Camp, at sea level, with a characteristically Mediterranean warmer and sunny weather.
Materials and methodsWe conducted a retrospective study by reviewing the cases of onset of type 1 diabetes in individuals aged less than 19 years in Osona (Barcelona) and Baix Camp (Tarragona) over a period of 13 years (2000–2012), obtaining data from the medical records of the paediatric endocrinology units of the two regional public hospitals located at the capital of each region: the Hospital Universitari de Vic and the Hospital Universitari Sant Joan de Reus, which are the referral hospitals for all diabetes onset cases in the area. To calculate incidence rates, we obtained demographic data for the general population from the Institut d’Estadística de Catalunya (Institute of Statistics of Catalonia). The incidence rate is the number of new cases relative to the overall susceptible population and is expressed per 100000 inhabitants (younger than 19 years) per year. We applied a 95% confidence interval to the calculation of incidence rates. We defined T1DM onset and presence of ketoacidosis according to the criteria established by the ISPAD.1 We compared the data by means of the Student's t test, or with the Mann–Whitney U test if the size of the compared subsets was small. The level of statistical significance was set at 0.05. The relative risk (RR) was calculated as the ratio of the incidence of T1DM onset and the population under consideration. We expressed metabolic control, assessed by the level of glycated haemoglobin (HbA1c), as the mean HbA1c level for the last two years. We performed the statistical analysis with the software SPSS version 21 (IBM).
ResultsThe population under 19 years of age amounted to 53978 inhabitants in 2000, and had increased to 73443 by year 2012, mostly on account of immigration. This increase amounts to 36.6% of the population in this age group. Considering the local population and the immigrant population separately, we observe the following evolution: the native population grew from 51440 to 61202, with an increase of 18.9%, while the immigrant population grew from 2537 to 12240, which amounts to an increase of 482%, that is, it quadrupled (became 4.82 times larger). The distribution of the child and adolescent population by national origin has changed, as in 2000 95.3% of the population was of Spanish descent and only 4.7% corresponded to immigrants, while in 2012, 83.3% was of Spanish descent, with the proportion of immigrants increasing to 16.7%. As for the countries of origin in the areas under study, most immigrants were Maghrebi (90%), with a much smaller proportion of Central and South Americans (5%), Chinese (2%) and Sub-Saharan Africans (2%), so we narrowed down the analysis of the outcomes to the Maghrebi group alone.
In the thirteen years under study, there were 118 cases of diabetes onset in our two hospitals, which corresponds to a mean 9.1 cases of diabetes onset per year. When it came to age, during this period, in the age 0-to-4 year group 20 cases corresponded to children of Spanish descent and 24 to children of Maghrebi descent, while in the 5-to-18 years age group, 57 occurred in children of Spanish descent and 17 in children of Maghrebi descent.
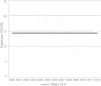
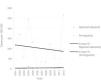
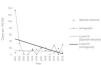
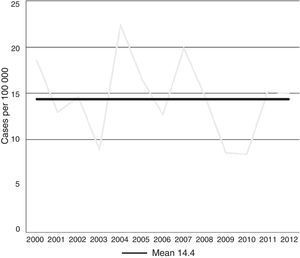
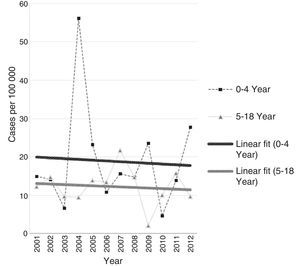
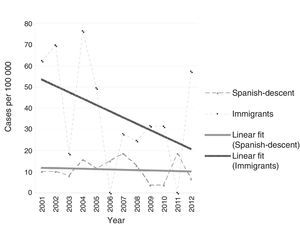
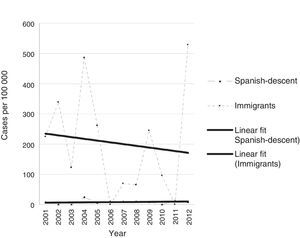
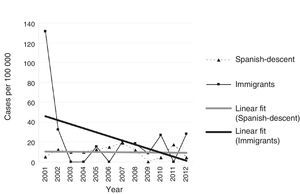
The incidence rate remained stable in the two regions for the overall population under 19 years of age during the period under study, at 14.4 cases per 100000 inhabitants per year (95% CI, 11.8–31.3; Fig. 1), whereas narrowing down the group to children aged less than 15 years, this incidence increases to 17.8 cases per 100000 inhabitants per year (95% CI, 14.7–39.2). The incidence did not vary by sex, and it was 15.1 in males (95% CI, 11.4–34.0) and 13.4 in females (95% CI, 9.8–30.5), a difference that was not statistically significant (P>.05). However, we did find significant differences between age groups, with an incidence of 18.9 cases per 100000 inhabitants per year (95% CI, 6.6–28.0) in children aged 0–4 years and of 12.5 cases per 100000 inhabitants per year (95% CI, 7.4–23.7) in the group aged 5 to 18 years (P<.05; Fig. 2). We found the largest differences in the incidence of T1DM in our analysis by the origin of patients, with an incidence of 37.1 cases per 100000 inhabitants per year (95% CI, 26.3–87.5) in children of Maghrebi descent, far higher than the incidence in children of Spanish descent, which was of 11.2 cases per 100000 inhabitants per year (95% CI, 7.4–21.3; P<.001; Fig. 3), with the high incidence of diabetes onset in the under-5 years Maghrebi population compared to the same subset in the local population contributing the most to this difference: 192.0 (95% CI, 115.2–460.8) versus 8.2 (95% CI, 4.6–20.0) cases per 100000 inhabitants per year (P>.001; Fig. 4). These differences in incidence by age group and national origin remained when we analysed the two regions separately.
The RR of developing T1DM in our region is 3.1 times higher for the overall Maghrebi population compared to the local population, and 1.5 times higher for children aged fewer than 5 years compared to children aged 5–18 years, independent of national origin. When we made the analysis by age group, we found that the incidence in the 5-to-18 years group was higher in individuals of Maghrebi versus Spanish descent: 17.8 (95% CI, 9.3–44.0) versus 10.2 (95% CI, 7.5–23.1) cases per 100000 inhabitants per year, with a RR of 1.7. The difference was substantially larger for the 0-to-4 years age group in the Maghrebi population compared to the corresponding local population: 192.0 (95% CI, 115.2–460.8) vs. 8.2 (95% CI, 4.6–20.0) cases per 100000 inhabitants per year (P<.001), which corresponds to a RR in the Maghrebi under-5 years subset of 23.4 compared to the Spanish subset for the same age. However, we observed a decreasing trend in incidence in the Maghrebi population in the period under study, for while the number of cases per year remained stable, the population of Maghrebi children susceptible to developing the disease also grew, which results in a gradually decreasing trend in incidence over the 13 years under study. Thus, if we divide the period under study in four-year bands, leaving out year 2000, the evolution of the incidence in children of Maghrebi descent (in cases per 100000 inhabitants/year) was 56.5 (95% CI, 34.1–190.2) in 2001–2004, 25.4 (95% CI, 9.4–64.8) in 2005–2008, and 29.9 (95% CI, 15.4–78.2) in 2009–2012. Meanwhile, the incidence remained stable in children of Spanish descent. The decrease in the incidence of diabetes onset in the immigrant population is explained mostly by a decrease in the incidence in the under-5 years population, although the incidence also decreased in the group aged 5-to-18 years (Figs. 4 and 5). We found that in 2000, the first year in the study, there were extreme incidence values in the Maghrebi population (118.2 cases per 105 inhabitants/year; 95% CI, 0.0–370.2), mostly on account of the under-5 years (636.9 cases per 105 inhabitants/year; 95% CI, 0.0–2153.8) and due to the small size of this subpopulation, which is why we omitted this year in the charts (Figs. 2–5), starting the graphical representation at year 2001 to smooth the incidence trendlines.
We analysed other factors, such as the presence of ketoacidosis at onset. Out of the total cases, 45.8% presented with ketoacidosis at onset compared to 54.2% that did not. We found statistically significant differences in the presence of ketoacidosis by age group, as it was found in 48.1% of the under-5 years group and in 51.9% of de 5-to-18 years group (P=.025). However, we did not find differences based on origin, with ketoacidosis present in 48.7% of the Maghrebi descent group and 44.3% of the Spanish descent group (P>.05).
Metabolic control did not vary by age or origin of the individuals included in the study. The mean level of HbA1c in the last two years was similar in the 0-to-4 years and the 5-to-18 years age groups (8.8% and 8.6%, respectively; P=.036). The Spanish and Maghrebi origin groups also had similar HbA1c levels (8.5% and 9.0%, respectively; P=.066).
DiscussionIf we refer to the world-wide incidence study of Karvonen et al. in which Spain is represented by data from the Catalonia register, with an incidence classified as high of 12.6 (expressed in cases per 100000 inhabitants per year), our age 5-to-18 years subset would have a similar incidence at 12.5; however, the incidence in Spanish natives would be lower, of 11.1. The incidence in the under-5 years subset, of 18.9, and in the Maghrebi descend subset, of 37.1, would both exceed previously reported rates, especially in the Maghrebi descent group, which would be at the level of very high-incidence countries such as Sweden or Finland (27.5 and 36.5 cases per 105inhabitants/year, respectively) and in the Maghrebi subset of under-5 years, with an incidence that has not yet been reported in any country (192.0 cases per 105inhabitants/year). Although we found this very high incidence in Maghrebi immigrants residing in Spain and we have not found any published registers for the incidence of diabetes in Morocco, we did find records for neighbouring countries where the incidence is intermediate, such as Algeria and Tunisia, with an incidence of 5.7 and 4.9–8.8 cases per 100000 inhabitants per year, respectively. Although we cannot know how reliable the registers showing these low incidence rates may be, the high incidence found in individuals of Maghrebi descent residing in Spain is still striking.2
If we consider the percent distribution of the overall population aged less than 19 years, with 17% of Maghrebi descent and 83% of Spanish descent, we would expect a similar distribution in the population with T1DB if national origin were not a risk factor for the disease; however, we found that the percentage of diabetes onset cases was nearly double in the Maghrebi population (33%) while there was a relative reduction in the Spanish population (67%).
We ought to underscore the very high incidence found in the under-5 years age group in the Maghrebi population compared to the Spanish population (192.0 vs. 8.2 cases per 105inhabitants/year). While the absolute frequency of diabetes onset cases in children aged less than 5 years during the period under study was 24 for a susceptible population in the denominator of 12498, for the purposes of analysis it would be convenient to have a base population of 100000 children under five years to obtain a more accurate incidence, which would allow better comparisons with homologous age groups from other geographical areas.
Current recorded incidence rates in Spain vary widely by autonomous community, ranging from 11.5 cases per 100000 inhabitants per year in Asturias to 27.6 cases per 100000 inhabitants per year in Castilla-La Mancha.3 When it came to our study, the incidence rate for the overall sample was in the high range at 14.4 cases per 100000 inhabitants per year; however, we found a strikingly high incidence the Maghrebi population of 37.1 cases per 100000 inhabitants per year, corresponding to a RR 3.1 times higher than the RR in children of Spanish descent and up to 23.4 times higher in Maghrebi children aged less than 5 years. The potential impact of immigration in the pathophysiology of diabetes development is generating considerable interest and studies on the subject are starting to be published, especially in countries with a high incidence such as Sweden. Hussen et al. analysed the incidence of T1DM in individuals born in Sweden based on parental origin, and found that individuals born to two native Swedes had an increased RR of having T1DM compared to individuals with one foreign-born parent, in who the risk decreased by 15–30% with an even greater risk reduction if both parents had been born abroad. These differences were confirmed for immigrants from Asia, South and North America and Western and Eastern Europe. Conversely, the RR of developing T1DM was 20–40% higher in immigrants of African descent, especially those from North or East Africa, a region that includes Morocco, which is therefore consistent with our results. This increased risk has also been observed in African immigrants residing in Sweden. These findings suggest that genetic predisposition interacts with environmental factors in the new country of residence,4 an observation that had already been made by Hjern and Söderström, who found an increased incidence in individuals of East African descent born in Sweden compared to a reduced incidence in individuals born in Africa that migrated at a later point.5 Söderström et al. also found an increased incidence in individuals born in Sweden to parents from low-incidence countries compared to adopted individuals, which suggests that some of the environmental factors at play in high-incidence countries may act during intrauterine development or in very early infancy, triggering the pathophysiological process that leads to T1DM.6 The Hussen group recently added that the risk of developing T1DM in children born to immigrant mothers also increases with the amount of time the mother has been in Sweden, that is, the longer the time of residence in Sweden, the greater the risk of developing T1DM, which also points at the importance of environmental factors or lifestyle changes as determinants in the aetiology of T1DM.7 Gillespie et al. have previously reported that while the global incidence of T1DM is increasing, the frequency of high-risk HLA DR3-DQ2/DR4-DQ8 haplotypes in patients with a T1DM diagnosis has been decreasing, which increases the relevance of the hypothesis that environmental factors play a greater role in the increase in global incidence than genetic factors.8,9
Although studies conducted in the past have reported a greater prevalence of ketoacidosis at the time of diagnosis in the under-5 years age group, our analysis did not lead to the same results, as the prevalence of ketoacidosis was slightly lower than in the 5-to-18 years age group; and unlike what has been described for the United States,10 our analysis of prevalence by origin found a similar proportion in Spanish natives than in the immigrant population.
Consistent with the data reported by Okrainec et al., who found no difference in the incidence of diabetes complications between locals and immigrants, we did not find differences in the level of metabolic control based on national origin.11
Finally, we conclude that the children and adolescent population of Maghrebi descent that resides in our area has a risk of developing T1DM that is three times as high as that of the Spanish population of the same age, and up to 23 times higher for children aged less than 5 years, which opens a field of investigation on the risk factors that may be affecting this population in the destination countries, with the greatest impact on the under-5 years age group.
Conflicts of interestThe authors have no conflict of interests to declare.
Please cite this article as: Torrabías-Rodas M, Feliu-Rovira A, Porcar-Cardona I, Altimiras-Roset J. Alta incidencia de diabetes tipo 1 en población magrebí de Osona y Baix Camp. An Pediatr (Barc). 2017;86:176–181.