Foreign body (FB) ingestion is an uncommon reason for going to the Paediatric Emergency Department (PED). The aim of this study was to assess the clinical and epidemiological characteristics of foreign body ingestion and the management of these patients.
Patients and methodsRetrospective study, including children under 14 years old with suspected foreign body ingestion seen in the PED between 2010 and 2013. An analysis was made of the circumstances of the FB ingestion, its management in the PED, and patient outcomes.
ResultsOf the 226.666 presentations recorded, 1.608 (0.7%) were for a FB, 970 corresponding to ingestion of mainly fish bones (367, 38.7%) and coins (181, 18.7%), except in children under 1 year (plastic objects). The median age was 4.7 years, with boys being more common in those older than 4 years (58.5%). A total of 557 patients (57.3%) reported some symptom, and complementary tests were performed in 414 (42.7%). Another specialist was called in 315 (32.4%) cases, mainly from Ear, Nose and Throat (fish bones) or Surgery (coins). The FB was removed in 305 (31.4%) cases, which were mostly fish bones or sunflower seeds. Seventy-one patients (7.3%) were admitted, especially ingestion of fish bones or coins. No patient died.
DiscussionIngestion of fish bones or coins by young children is a relatively common presentation in the PED, and it is associated with frequent medical interventions. Although the overall prognosis is good, improving the health education of the population should be considered to reduce the frequency of these episodes.
La ingesta de un cuerpo extraño (CE) es un motivo de consulta poco frecuente en Urgencias. El objetivo es conocer las características clínico-epidemiológicas de las ingestas de CE y el manejo de estos pacientes.
Pacientes y métodosEstudio retrospectivo incluyendo a los pacientes menores de 14 años que consultaron en un Servicio de Urgencias de Pediatría en relación con la ingesta de un CE entre 2010 y 2013. Se analizaron las circunstancias que rodearon la ingesta del CE, el manejo en Urgencias y la evolución de los pacientes.
ResultadosDe los 226.666 episodios registrados, 1.608 (0,7%) estuvieron relacionados con un CE, correspondiendo 970 a ingestas, sobre todo espinas de pescado (367, 38,7%) y monedas (181, 18,7%), salvo en menores de un año (objetos de plástico). La mediana de edad fue 4,7 años, siendo mayoritariamente varones a partir de los 4 años (58,5%); 557 pacientes (57,3%) estaban sintomáticos y en 414 (42,7%) se realizó alguna exploración complementaria. Se requirió la participación de otro especialista en 315 (32,4%), fundamentalmente Otorrinolaringología (espinas) o Cirugía (monedas). En 305 (31,4%) se extrajo el CE, fundamentalmente espina o pipa de girasol. Ingresaron 71 pacientes (7,3%), sobre todo por ingestas de espinas o monedas. Ningún paciente falleció.
ConclusionesLa ingesta de espinas o monedas por parte de los niños pequeños es un motivo de consulta relativamente frecuente en Urgencias. Aunque el pronóstico global es bueno, se asocia a frecuentes intervenciones médicas. Debe considerarse mejorar la educación sanitaria de la población para disminuir la frecuencia de estos episodios.
Every year, more than 20.000 children aged 1–14 years die from unintentional injuries in developed countries.1,2 In Spain, these injuries, formerly referred to as accidents, are the third leading cause of death in the population aged less than 15 years.3
Unintentional injuries due to foreign bodies (FBs) involve the introduction in a body orifice, aspiration or ingestion of FBs. Ingestion is the most common mechanism and, combined with aspiration, a major cause of morbidity and mortality, especially in children aged less than 3 years.4
Foreign body ingestion is common in the paediatric age group. The 2011 annual report of the American Association of Poison Control Centers’ National Poison Data showed that more than 110.000 ingested foreign bodies were reported in the United States that year, of which more than 85% occurred in the paediatric population.5
The types of FB ingested vary widely based on the social and cultural characteristics of different geographical areas. The most frequently ingested objects in Western countries are coins,6–10 while in Asia they are fish bones.9–11 The clinical manifestations of FB ingestion are variable, as is its presentation in patients seeking emergency care. Nearly half of the patients are asymptomatic on arrival to the emergency department, excepting patients in whom the FB is lodged in the oropharynx.6,7 Otherwise, patients may present with respiratory, gastrointestinal or nonspecific symptoms that may delay the diagnosis and cause significant damage in the gastrointestinal tract. In addition, several diagnostic tests may be performed in many of these patients, or they may require different treatments or admission to the hospital.
Many of these episodes are preventable.12 In fact, guidelines on how to avoid these accidents are provided to parents and caregivers during health checkups. Still, FB ingestion continues to be a frequent reason for emergency department visits.5 An understanding of the clinical and epidemiological characteristics of these accidents and their management could facilitate the design of more efficacious preventive measures and improve the care provided to these children. However, there are no studies on large samples in our setting.
The primary objective of this study was to determine the clinical and epidemiological characteristics of children that seek care in emergency departments due to FB ingestion. The secondary objective was to identify circumstances associated with a higher probability of some type of intervention being performed on these patients (testing, treatment or hospital admission).
Patients and methodsWe conducted a retrospective study with the inclusion of patients aged less than 14 years that sought care in relation to a FB ingestion at the Paediatric Emergency Department (PED) of a tertiary level teaching hospital.
We obtained information on the patients and FB ingestion episodes from the electronic health records of the PED and the public health system. We collected data on the following variables: type of FB, age, sex, personal history, time elapsed since ingestion, symptoms, patient condition on arrival to PED, initial management, diagnostic tests, treatment received, discharge destination and outcome.
Foreign bodies were classified as follows:
- 1.
Pointed, sharp or elongated objects:
- –
Pointed or sharp: piercing and cutting FBs (fish bones, chicken bones, pins, needles, razor blades, straightened paper clips, nails and toothpicks).
- –
Long: FBs 2–3 or more cm in length in children aged less than 1 year, or 3–5 or more cm in length in older children (toothbrushes, spoons, …).
- 2.
Coin.
- 3.
Blunt object: FB without a sharp point or edge (buttons, balls, …), excluding coins.
- 4.
Radiolucent object: object that is not pointed, sharp or elongated and not seen in X-ray images, such as steel or plastic objects.
- 5.
Button battery.
- 6.
Other type of battery.
- 7.
Magnetic object.
- 8.
Food bolus: food that has been chewed and mixed with saliva.
- 9.
Food: parts of foods, such as cherry or olive stems.
- 10.
Unclear or unknown.
In order to identify situations associated with a higher probability of having some intervention performed on the patient, we analysed the performed tests, consultations with other specialists, treatments administered and discharge destination of children that sought care for FB ingestion.
The study was approved by the Clinical Research Ethics Committee of the Hospital. Since data were retrieved and recorded on an anonymous basis and no intervention was performed on the patients, we did not need to obtain the informed consent of each patient.
We performed the statistical analysis with the software SPSS 22.0 for Windows (SPSS Inc., Chicago, USA). We have expressed qualitative variables as absolute frequencies and percentages. We used the chi square test to analyse the association between qualitative variables. We compared continuous quantitative variables that were normally distributed with Student's t test. For variables that did not have a normal distribution, we used the Kruskal–Wallis and the Mann–Whitney U tests.
ResultsDuring the period under study, there were 226.666 visits of children under age 14 years to the PED. Of these visits, 1.608 (0.7%; 95% CI, 0.68–0.74) involved an unintentional injury associated with a FB, and of these, 970 (60.3%; 95%, 57.9–62.3) corresponded to FB ingestions.
Circumstances of foreign body ingestionNinety-eight percent of the patients that sought care in our hospital for a FB ingestion had no relevant personal history, such as psychiatric disorders (8; 0.8%) or intellectual disability (7; 0.7%). Most patients (851; 87.7%) went directly to the PED of our hospital. Of the 119 patients referred for evaluation, 85 (71.4%) were referred from primary care and 34 (28.5%) from other hospitals in the area.
There was a mild predominance of visits on weekdays, a difference that was not statistically significant.
The time elapsed between FB ingestion and the visit to our hospital was documented for 535 episodes. The median was 2.0h, and it ranged between 15min and 720h, with approximately 60% of patients visiting in the first two hours. More than 48h had elapsed in approximately 7%, and most of these patients were those that had ingested a coin or a blunt object.
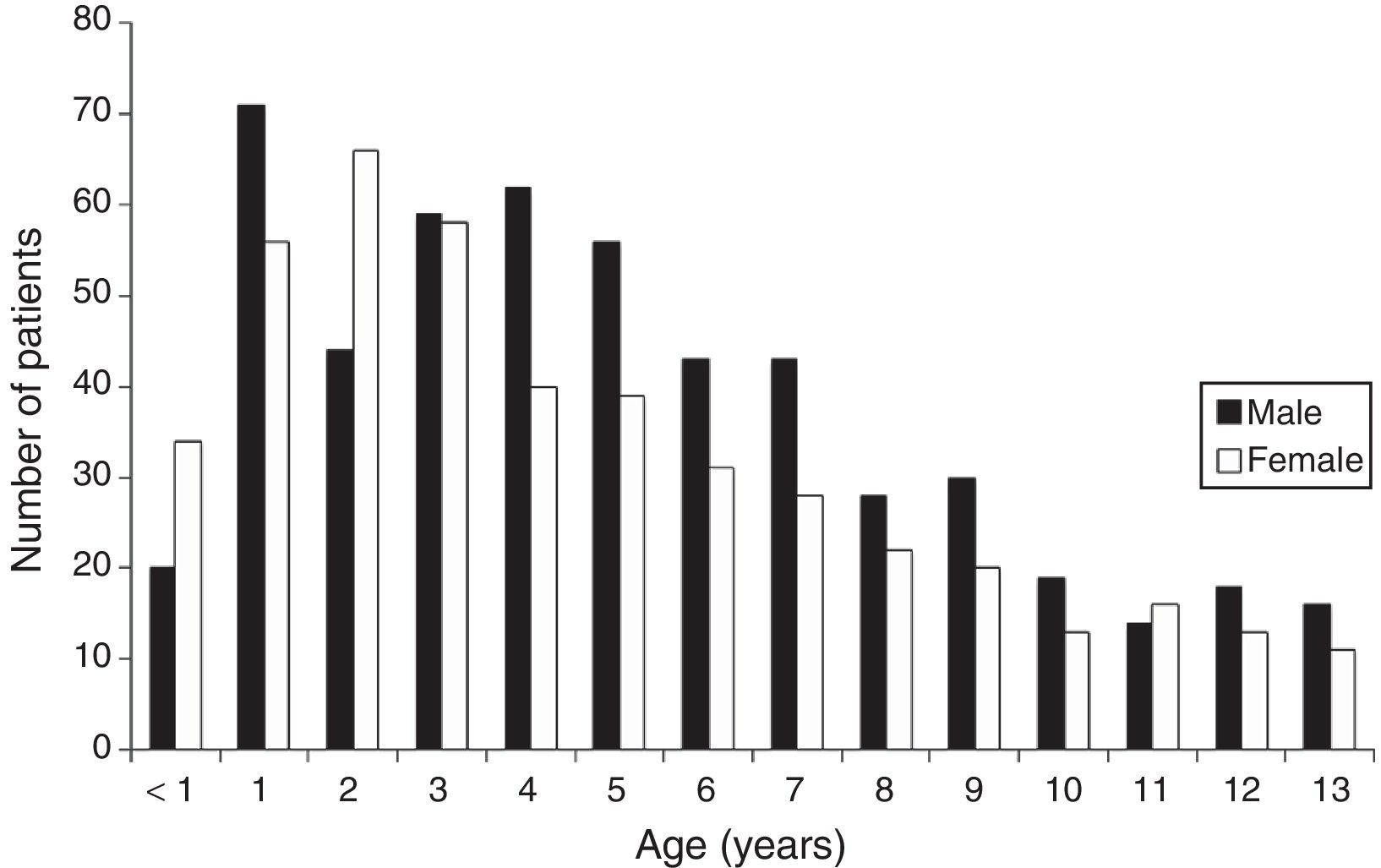
Overall, the predominant age group was 1–4 years (456; 47%), and the median age was 4.7 years (interquartile range, 2.6–7.6). The youngest patient was 4 months old.
There was a slightly higher proportion of males (523; 53.9%) stemming from a predominance of males starting at age 4 years (58.5% vs 47.5% in children aged less than 4 years; P=0.001; Fig. 1).
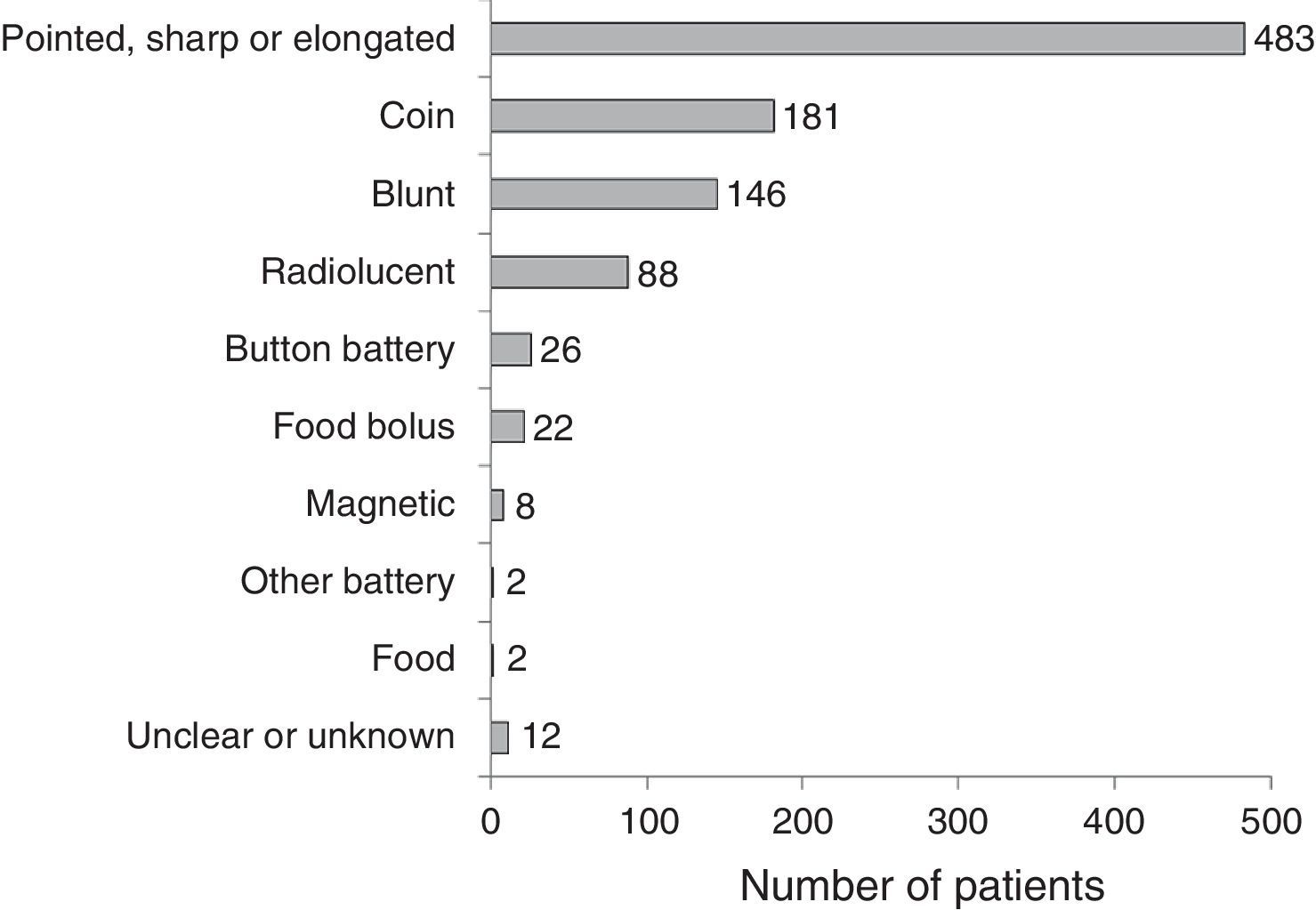
Foreign body characteristicsSingle FB ingestion was suspected in 932 patients (96.1%), and the maximum number of FBs ingested was nine. Multiple FB ingestions most commonly involved coins, button batteries and magnets.
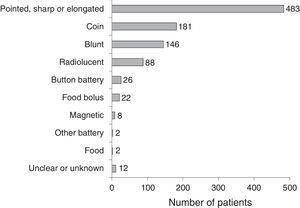
There was broad variability in the characteristics of the FBs (Fig. 2), and the most frequently found objects were pointed, sharp or elongated. Among this type, 367 were fish bones (76%). Patients referred from primary care or other hospitals had usually ingested fish bones or coins.
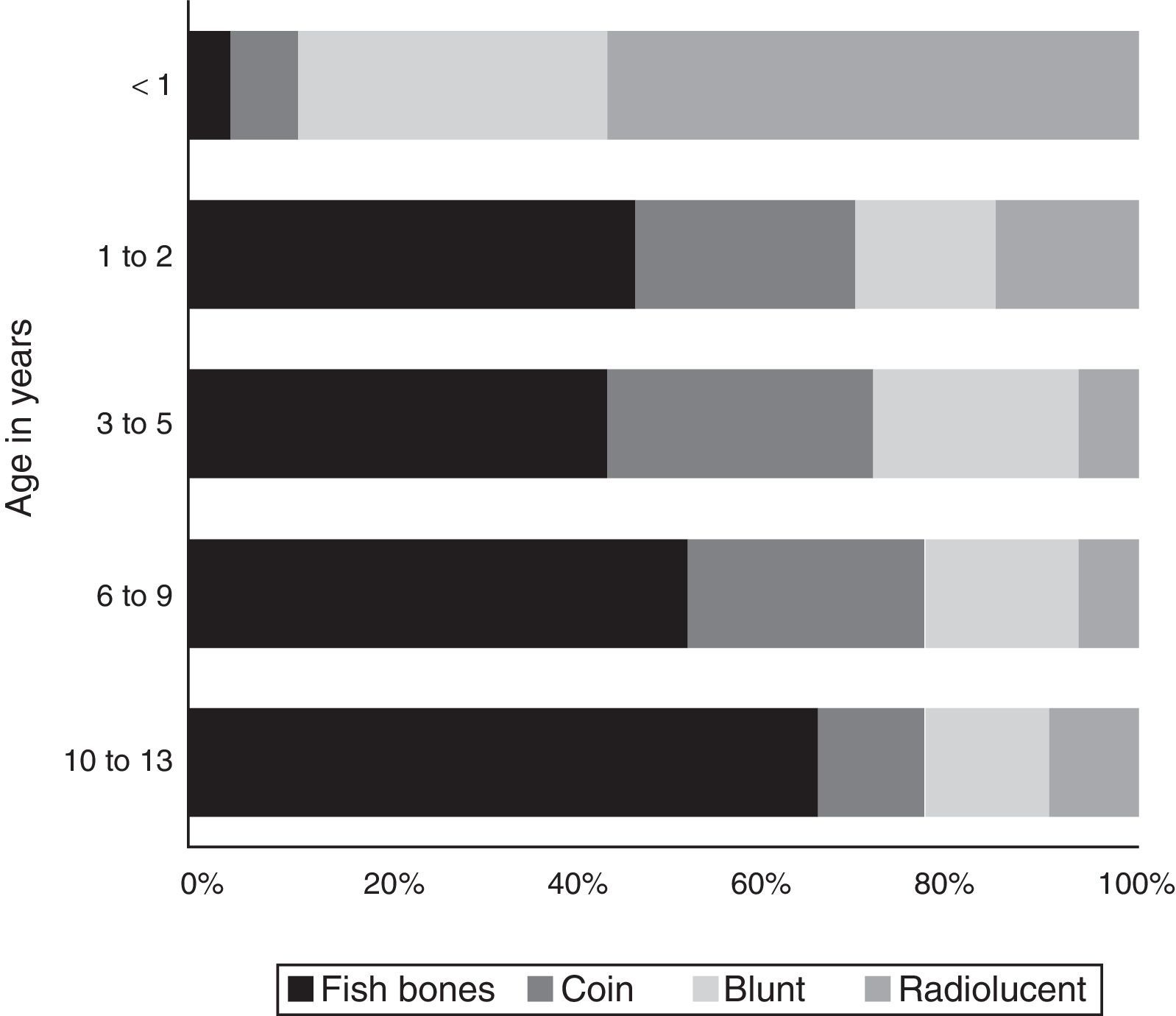
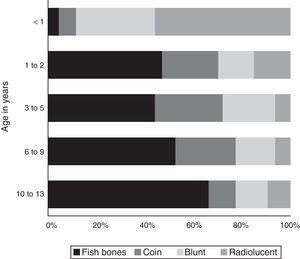
The type of FB also varied significantly by age (Fig. 3).
Overall, fish bones were the most frequently ingested FB, except in infants younger than 1 year, who most frequently ingested radiolucent and blunt objects (pieces of plastic, labels or toy parts), and children aged 13 years, who most frequently ingested sunflower seeds. Coins were the second most frequently ingested type of FB in the 2–9 years age band, and especially in children aged 2–5 years.
The FB was found in 585 cases (60.3%). Of these, 275 were located in the oropharynx (47%; 95% CI, 43.0–51.5), 43 in the oesophagus (7.4%; 95% CI, 5.5–9.7%), 64 in the stomach (10.9%, 95% CI, 8.7–13.7) and 58 distal to the pylorus a (9.9%; 95% CI, 7.7–12.6). In 145 patients in whom only a metal detector was used to locate the FB, the location was infradiaphragmatic (24.8%; 95% CI, 21.5–28.4).
Nearly 100% (261; 94.5%) of the FBs located in the oropharynx were of the pointed, sharp or elongated type (mainly fish bones), while the majority of FBs of other types were found distal to this location.
Clinical manifestationsNo patient showed signs of life endangerment or required resuscitation manoeuvres or airway management on arrival to the PED. Slightly more than half (556; 57.3%) were symptomatic, with the most frequent symptoms being gastrointestinal (pain, dysphagia, FB sensation, …). The presence or absence of symptoms was associated with the location and type of FB. Symptoms were present in 97.1% of patients with an oropharyngeal location, 79.1% of cases with oesophageal location, 18.8% of patients with a gastric location, 13.8% of patients with locations distal to the pylorus, and 13.8% of patients with an unspecified infradiaphragmatic location (P<0.001). The FBs most frequently associated with symptoms were food boluses (90.9%) and pointed, sharp or elongated objects (87.7%).
Tests, treatment and discharge destinationSome type of diagnostic test was performed in 414 patients (42.7%): metal detector scan (267; 27.5%), X-ray (256; 26.4%), oesophagogram (9; 0.9%) and computed tomography scan (3; 0.3%). Two tests were performed in 120: metal detector scanning and radiography. The tests used differed based on the type of FB. Metal detectors were used mainly in the management of patients that sought care for the ingestion of coins (59.2%) or of blunt metal objects (24.7%). Radiography was mainly performed in patients that had ingested blunt objects (29.3%), coins (28.9%) and pointed, sharp or elongated objects (15.6%). Oesophagograms were performed mainly in patients that had ingested food boluses (55.5%).
Gastrointestinal endoscopy is considered a diagnostic and therapeutic technique and was performed in 43 patients (4.4%), mainly for the management of patients that had ingested coins (28; 65.1%).
The performance of tests varied based on patient origin (43.9% of patients that visited the PED directly, 28.2% of patients referred from primary care, and 47.1% of those referred from other hospitals).
Watchful waiting with no treatment in the PED was the approach used in 641 patients (66.1%), and it was most frequent in children referred from primary care (50.1%). In the remaining patients, the most commonly used interventions were urgent or deferred extraction (305 [31.4%], in most cases removal of a fish bone or sunflower seed), medical treatment (2; 0.2%) and insertion of a nasogastric tube (2; 0.2%).
Twenty patients (2.1%) expelled the FB at the PED, either spontaneously or during extraction attempts.
In 655 patients (67.5%) the intervention of another specialist was not required, and the departments consulted most frequently were Otorhinolaryngology (232 patients [23.9%]; 220 for ingestion of pointed, sharp or elongated FB, mostly fish bones), Surgery (77 patients [7.9%]; 32 for ingestion of coins) or both (6 patients [0.6%]).
More than 90% (899) of patients were discharged home from the PED, and hospital admission was more frequent in patients that had been referred from other hospitals (39.1%). Forty patients (4.1%) were moved to the operating theatre from the PED, especially for coin ingestion (22; 55%). Thirty-one patients (3.2%) were admitted for observation to the Paediatric Emergency Observation Unit (17; 1.8%) or an inpatient ward (14, 1.4%), who were mostly patients that had ingested coins or pointed, sharp or elongated objects. None of the patients were admitted to the paediatric intensive care unit.
OutcomeSixty-nine patients (7.1%) returned to the hospital after the initial visit, with a predominance of patients that had ingested coins (49.3%). Of the patients that made return visits to the PED, 46 (69.7%) had some type of diagnostic test performed in their second visit (every patient that had ingested a button battery and around 70% of patients that had ingested a coin or blunt object).
Of all patients that made return visits, three (0.3%) required surgical intervention (due to coin, button battery and fish bone ingestion).
No patients died during the period under study.
DiscussionUnintentional injury associated with FB ingestion is a relatively frequent reason for seeking care at PEDs, especially in children aged less than 5 years. There is considerable variation in the characteristics of ingested FBs. Families typically seek emergency care promptly, and the prognosis is generally good, although many children undergo various diagnostic tests and different treatments. We did not find an increased incidence in association with psychiatric disorders or disabilities.
Despite the variability, we could clearly identify the two most common patterns in our region. The most frequent reason for seeking care was the presence of local symptoms secondary to ingestion of fish bones in children aged more than 1 year. The fact that the most frequent type of FB observed in our study differed from those reported in other studies in Western countries6–10 may be due to our coastal location, where there is an increased consumption of fish, as happens in other parts of the world.9–11,13 This fact is strongly associated with the dietary habits of the population. These children are often symptomatic and it is not rare for them to require the involvement of other specialists (mainly ear, nose throat specialists) in their assessment and treatment. Given the frequency of these cases, it may be worth considering improving the training of paediatricians for their assessment. On the other hand, families should be made aware of the frequency of these accidents, providing better health education on aspects that should not be forgotten in order to improve prevention. Another aspect that should not be obviated is instructing families to promptly seek care in the event of fish bone ingestion in order to prevent the development of secondary oedema, thus facilitating both detection on physical examination and subsequent removal.
The second most frequent type of visit corresponds to children aged 2–5 years brought to the PED after ingesting a coin and presenting with no symptoms. Coins are the type of FB reported most frequently in cases of FB ingestion seen in emergency services in Western countries.6–10 Although these cases rarely give rise to complications5,14 or even death,15 it is imperative to provide improved education to family members and caregivers, emphasising the fact that children aged less than 6 years should never be allowed to play with coins.
In fact, while the final outcomes were good, ingestion of both fish bones and coins accounted for the majority of hospital admissions. Furthermore, diagnostic tests were needed in nearly half of the patients that sought care at the PED, and their use was particularly frequent in cases of coin ingestion. A salient finding in our study was the frequent use of metal detectors. Detectors are devices that use electromagnetic pulses to detect the presence of metallic or ferromagnetic objects, and their usefulness in the detection of metal FBs has been proven.16–18 Thus, the visits that most frequently required urgent intervention were those relating to fish bone and coin ingestions. Combined with the fact that these are the most frequently ingested FBs, this evinces the need to focus prevention efforts on this type of ingestions. Still, considering the wide variability in the ingested FBs, we cannot neglect general preventive measures, although recommendations must be tailored specifically to different age groups. For instance, the number of visits by children aged less than 2 years due to ingestion of plastic objects or parts is alarming. Foreign body aspiration is one of the leading causes of death in this age group.4 On the other hand, the numerous visits of patients aged more than 12 years related to sunflower seed ingestion must make us consider the appropriate way to reach out to this population.
There are several limitations to our study. Due to its retrospective design, some of the less serious cases may have not been identified, and some data may not have been recorded. Nevertheless, the availability of electronic databases for patient management and for the storage of electronic medical records for all paediatric patients minimises this limitation and has sufficed to achieve the objectives of our study. On the other hand, since this was a single-centre study, its conclusions must be generalised with caution, but considering the extent of coastal areas in other European countries and the culture-related consumption of fish, it would not be surprising if similar results were found in other coastal regions in Europe. Last of all, since we conducted the study in a PED, this may have led to limited recording of data regarding less-severe episodes. Nevertheless, we believe the episodes reviewed can help identify the most important areas for improvement in relation to FB ingestion in the paediatric age group.
In conclusion, visits related to FB ingestion are relatively frequent in PEDs, and we identified the most frequent patterns of FB ingestion. Although the prognosis is good, the number of visits to emergency departments and of diagnostic tests and procedures performed in these patients underscores the importance of developing appropriate educational interventions for this population, especially in relation to fish bones and coins.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Lobeiras A, Zugazabeitia A, Uribarri N, Mintegi S. Consultas relacionadas con la ingesta de un cuerpo extraño en Urgencias. An Pediatr (Barc). 2017;86:182–187.
Previous presentation: this study was presented as a brief oral communication, “Peculiaridades de los cuerpos extraños ingeridos y su manejo en un Servicio de Urgencias Pediátricas”, at the XX Annual Meeting of the Sociedad Española de Urgencias Pediátricas; April 16–18, 2015.