A boy age 13 years was brought to hospital by the medical emergency team following two episodes of loss of consciousness. The patient had vomited stomach contents mixed with blood between both episodes.
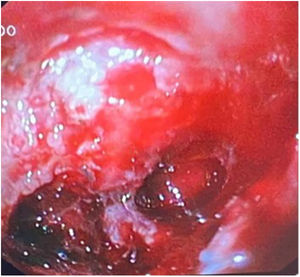
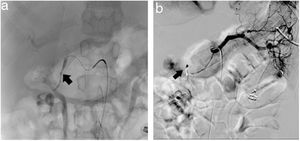
On arrival, he was unstable, and the following tests were ordered: head CT scan, complete blood count and panel, and upper gastrointestinal endoscopy (UGIE). The latter revealed a large, excavated defect in the duodenal bulb (Forrest Ib lesion) (Fig. 1) and oesophagitis (Los Angeles grade D). Massive bleeding developed during the procedure, prompting performance of resuscitation manoeuvres and injection of adrenaline and polidocanol in the preserved mucosa. Due to the persistence of bleeding, we performed an angiography with embolization of the gastroduodenal artery (Fig. 2), after which there was no further evidence of bleeding. Treatment with high-dose proton pump inhibitors (PPIs) was initiated. Further evaluation ruled out malignant disease, Helicobacter pylori was not detected the histological examination, and the basal serum concentration of gastrin and the findings of the single-photon emission CT scan were normal.
The patient remained in treatment for 7 months, with a follow-up UGIE, after discontinuation of PPI treatment, evincing antral gastritis with features suggestive of H. pylori infection, although the cultures remained negative. Serologic testing for detection of H. pylori was ordered and turned out positive. Given the high frequency of H. pylori associated with this condition, the decision was made to start empiric eradication therapy.1
Giant duodenal ulcers are rare but potentially severe lesions in the paediatric age group.2 Infection by H. pylori is the most frequent cause, and should be tested for in every case.3
Previous meeting: the case was presented as an oral communication at the II Virtual Scientific Meeting of the Sociedad de Pediatría de Asturias, Cantabria y Castilla y León (SCCALP), held online on November 4–5, 2021.